Addictions
Trudeau gov’t earmarks over $27 million for ‘safe supply’ drug program linked to overdoses and violence

From LifeSiteNews
The taxpayer money will help fund 22 drug distribution projects in British Columbia and Ontario.
Prime Minister Justin Trudeau’s Liberal government is planning to spend over $27 million on “safe supply” drug programs this year.
This week, Health Canada revealed that the Trudeau government has budgeted over $27 million in funding for “safe supply” drug programs that have been linked to increased violence and overdose deaths across Canada, according to information obtained by Rebel News.
“With regard to planned funding by the government related to ‘safe’ or ‘safer’ supply programs: How much does the government plan on spending on such programs, broken down by department, agency, and initiative in the current fiscal year and in each of the next five fiscal years?” Conservative Member of Parliament (MP) Tako Van Popta had questioned in April.
“Safe supply” is the term used to refer to government-prescribed drugs given to addicts under the assumption that a more controlled batch of narcotics reduces the risk of overdose. Critics of the policy argue that giving addicts drugs only enables their behavior, puts the public at risk, disincentivizes recovery from addiction and has not reduced — and sometimes even increased — overdose deaths when implemented.
Three months later, on June 17, the House of Commons revealed that the Trudeau government plans to spend an excess of $27 million to fund 22 drug distribution projects in British Columbia and Ontario.
The two largest recipients of federal funding are in Ontario, with Toronto’s South Riverdale Community Health Centre receiving $2.7 million and Kitchener’s K-W Working Centre for the Unemployed receiving $2.1 million.
In British Columbia, the largest recipient is the AVI Health and Community Services Society SAFER North Island in Campbell River at $2.02 million.
The Trudeau government’s funding for increased drug use comes after the program proved such a disaster in British Columbia that the province recently requested Trudeau recriminalize drugs in public spaces. Nearly two weeks later, the Trudeau government announced it would “immediately” end the province’s drug program.
Beginning in early 2023, Trudeau’s federal policy, in effect, decriminalized hard drugs on a trial-run basis in British Columbia.
Under the policy, the federal government began allowing people within the province to possess up to 2.5 grams of hard drugs without criminal penalty, but selling drugs remained a crime.
Since being implemented, the province’s drug policy has been widely criticized, especially after it was found that the province broke three different drug-related overdose records in the first month the new law was in effect.
The effects of decriminalizing hard drugs in various parts of Canada have been exposed in Aaron Gunn’s recent documentary, Canada is Dying, and in U.K. Telegraph journalist Steven Edginton’s mini-documentary, Canada’s Woke Nightmare: A Warning to the West.
Gunn says he documents the “general societal chaos and explosion of drug use in every major Canadian city.”
“Overdose deaths are up 1,000 percent in the last 10 years,” he said in his film, adding that “(e)very day in Vancouver four people are randomly attacked.”
Addictions
BC overhauls safer supply program in response to widespread pharmacy scam

A B.C. pharmacy scam investigation has led the provincial government to return to a witnessed consumption model for safer supply
More than 60 pharmacies across B.C. are alleged to have participated in a kickback scheme linked to safer supply drugs, according to a provincial report released Feb. 19.
On Feb. 5, the BC Conservatives leaked a report that showed the findings of an internal investigation by the B.C. Ministry of Health. That investigation showed dozens of pharmacies were filling prescriptions patients did not require in order to overbill the government. These safer supply drugs were then diverted onto the black market.
After the report was leaked, the province committed to ending take-home safer supply models, which allow users to take hydromorphone pills home in bottles. Instead, it will require drug users to consume prescribed opioids in a witnessed program, under the oversight of a medical professional.
Gregory Sword, whose 14-year-old daughter Kamilah died in August 2022 after taking a hydromorphone pill that had been diverted from B.C.’s safer supply program, expressed outrage over the report’s findings.
“This is so frustrating to hear that [pharmacies] were making money off this program and causing more drugs [to flood] the street,” Sword told Canadian Affairs on Feb. 20.
The investigation found that pharmacies exploited B.C.’s Frequency of Dispensing policy to maximize billings. To take advantage of dispensing fees, pharmacies incentivized clients to fill prescriptions they did not require by offering them cash or rewards. Some of those clients then sold the drugs on the black market. Pharmacies earned up to $11,000 per patient a year.
“I’m positive that [the B.C. government has] known this for a long time and only made this decision when the public became aware and the scrutiny was high,” said Elenore Sturko, Conservative MLA for Surrey-Cloverdale, who released the leaked report in a statement on Feb. 5.
“As much as I am really disappointed in how long it’s taken for this decision to be made, I am also happy that this has happened,” she said.
The health ministry said it is investigating the implicated pharmacies. Those that are confirmed to have been involved could have their licenses suspended, be referred to law enforcement or become ineligible to participate in PharmaCare, the provincial program that helps residents cover the costs of prescription drugs.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Witnessed dosing
The leaked report says that “a significant portion of the opioids being freely prescribed by doctors and pharmacists are not being consumed by their intended recipients.” It also says “prescribed alternatives are trafficked provincially, nationally and internationally.”
Critics of the safer supply program say it enables addiction, while supporters say it reduces overdoses.
Sword, Kamilah’s father, is suing the provincial and federal governments, arguing B.C.’s safer supply program made it possible for youth such as his daughter to access drugs.
Madison, Kamilah’s best friend, also became addicted to opioids dispensed through safer supply programs. Madison was just 15 when she first encountered “dillies” — hydromorphone pills dispensed through safer supply, but widely available on the streets. She developed a tolerance that led her to fentanyl.
“I do know for sure that some pharmacies and doctors were aware of the diversion,” Madison’s mother Beth told Canadian Affairs on Feb. 20.
“When I first realized what my daughter was taking and how she was getting it, I phoned the pharmacy and the doctor on the label of the pill bottle to inform them that the patient was selling their hydromorphone,” Beth said.
Masha Krupp, an Ottawa mother who has a son enrolled in a safer supply program, has said the safer supply program in her city is similarly flawed. Canadian Affairs previously reported on this program, which is run by Recovery Care’s Ottawa-based harm reduction clinics.
“I read about the B.C. pharmacy scheme and wasn’t surprised,” Krupp told Canadian Affairs on Feb. 20. Krupp lost a daughter to methadone toxicity while she was in an addiction treatment program at Recovery Care.
“Three years [after starting safer supply], my son is still using fentanyl, crack cocaine and methadone, despite being with Dr. [Charles] Breau and with Recovery Care for over three years,” Krupp testified before the House of Commons Standing Committee on Health on Oct. 22, 2024.
Krupp has been vocal about the dangers of dispensing large quantities of opioids without proper oversight, arguing many patients sell their prescriptions to buy stronger street drugs.
“You can’t give addicts 28 pills and say, ‘Oh here you go,’” she said in her testimony. “They sell for three dollars a pop on the street.”
Krupp has also advocated for witnessed consumption of safer supply medications, arguing supervised dosing would prevent diversion and ensure proper oversight of pharmacies.
“I had talked about witnessed dosing for safe supply when I appeared before the parliamentary health committee last October,” she told Canadian Affairs this week.
“I’m grateful that finally … this decision has been made to return to a witness program,” said Sturko, the B.C. MLA.
In 2020, B.C. implemented a witnessed consumption model to ensure safer supply opioids were consumed as prescribed and to reduce diversion. In 2021, the province switched to take-home models. Its stated aim was to expand access, save lives and ease pressure on health-care facilities during the pandemic.
“You’re really fighting against a group of people … working within the bureaucracy of [the B.C. NDP] government … who have been making efforts to work towards the legalization of drugs and, in doing that, have looked only for opportunities to bolster their arguments for their position, instead of examining their approach in a balanced way,” said Sturko.
“These are foreseeable outcomes when you do not put proper safeguards in place and when you completely ignore all indications of negative impacts.”
Sword also believes some drug policies fail to prioritize the safety of vulnerable individuals.
“Greed is the ultimate evil in society and this just proves it,” he said. “We don’t care about these drugs getting into the wrong hands as long as I get my money.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
Addictions
Calls for Public Inquiry Into BC Health Ministry Opioid Dealing Corruption
The leaked audit shows from 2022 to 2024, a staggering 22,418,000 doses of opioids were prescribed by doctors and pharmacists to approximately 5,000 clients in B.C., including fentanyl patches.
A confidential investigation by British Columbia’s Ministry of Health, Financial Operations and Audit Branch has uncovered explosive allegations of fraud, abuse, and organized crime infiltration within PharmaCare’s prescribed opioid alternatives program. Internal audit findings, obtained by The Bureau, suggest that millions of taxpayer dollars are being diverted into illicit drug trafficking networks rather than serving harm reduction efforts.
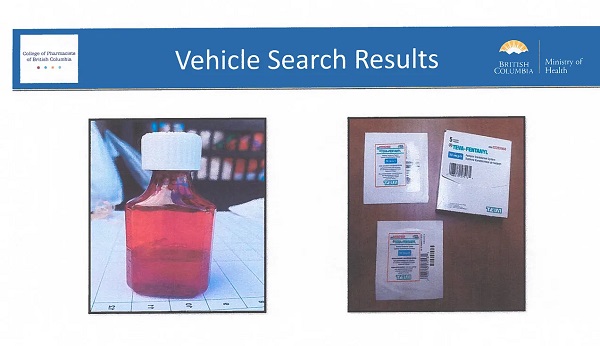
The leaked documents include photographs from vehicle searches that show collections of fentanyl patches and Dilaudid (hydromorphone) apparently packaged for resale after being stolen from the taxpayer-funded “safer supply” program. This program expanded dramatically following a federal law change implemented by Prime Minister Justin Trudeau’s government in 2020, which broadened circumstances in which pharmacy staff could dispense opioids, according to the document’s evidence.
“Prior to March 17, 2020, only pharmacists in BC were permitted to deliver [addiction therapy treatment] drugs,” the audit says.
B.C.’s safer supply program was launched in March 2020 as a response to the opioid overdose crisis, declared in 2016. It allows people with opioid-use disorder to receive prescribed drugs to be used on-site or taken away for later use.
The Special Investigations Unit and PharmaCare Audit Intelligence team identified a disturbing link between doctors, pharmacists, assisted living residences, and organized crime, where prescription opioids meant to replace illicit drugs are instead being diverted, sold, and trafficked at scale.
“A significant portion of the opioids being freely prescribed by doctors and pharmacists are not being consumed by their intended recipients,” the document states.
It suggests that financial incentives have created a business model for organized crime, asserting that “prescribed alternatives (safe supply opioids) are trafficked provincially, nationally, and internationally,” and that “proceeds of fraud” are being used to pay incentives to doctors, pharmacists, and intermediaries.
BC Conservative critic Elenore Sturko, a former RCMP officer, began raising concerns about the program two years ago after hearing anecdotes about prescribed opioids being trafficked. She asserts that the program is a failure in public policy and insists that Provincial Health Officer Dr. Bonnie Henry be dismissed for having “denied and downplayed” problems as they emerged. Sturko also argues that B.C. must change its drug policy in light of U.S. President Donald Trump’s stance linking the trafficking of fentanyl and other opioids to potential trade sanctions against Canada.
The document shows that PharmaCare’s dispensing fee loophole has incentivized pharmacies to maximize billings per patient, with some locations charging up to $11,000 per patient per year—compared to just $120 in normal cases.
Perhaps most alarming is the deep infiltration of B.C.’s safer supply program by criminal networks. The Ministry of Health report lists “Gang Members/Organized Crime” as key players in the prescription drug pipeline, which includes “Doctors, pharmacies, and assisted living residences.”
This revelation confirms long-standing fears that B.C.’s “safe supply” policy—originally designed to prevent deaths from contaminated street drugs—is instead sometimes supplying criminal organizations with pharmaceutical-grade opioids.
The leaked audit shows from 2022 to 2024, a staggering 22,418,000 doses of opioids were prescribed by doctors and pharmacists to approximately 5,000 clients in B.C., including fentanyl patches.
Beyond organized crime’s direct involvement, pharmacies themselves have exploited regulatory gaps to generate massive profits from PharmaCare’s policies:
- Pharmacies offer kickbacks to doctors, housing staff, and medical professionals to steer patients toward specific locations.
- Financial incentives fuel fraud, with multiple investigations identifying 60+ pharmacies offering incentives to clients.
- Non-health professionals, including housing staff, are witnessing OAT (opioid agonist treatment) dosing, violating patient safety protocols.
The Bureau is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
For the full experience, please upgrade your subscription and support a public interest startup. We break international stories and this requires elite expertise, time and legal costs.
-

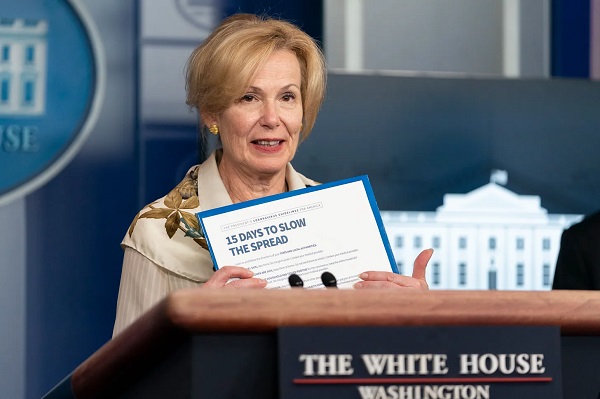
 COVID-192 days ago
COVID-192 days agoRed Deer Freedom Convoy protestor Pat King given 3 months of house arrest
-
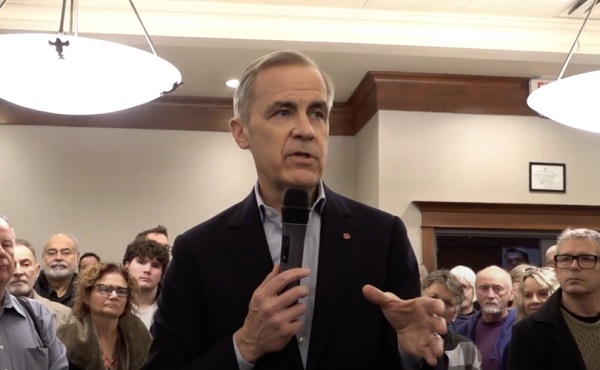
 Carbon Tax2 days ago
Carbon Tax2 days agoMark Carney has history of supporting CBDCs, endorsed Freedom Convoy crackdown
-

 Censorship Industrial Complex1 day ago
Censorship Industrial Complex1 day agoBipartisan US Coalition Finally Tells Europe, and the FBI, to Shove It
-
 Health2 days ago
Health2 days agoTrump HHS officially declares only two sexes: ‘Back to science and common sense’
-

 International2 days ago
International2 days agoSenate votes to confirm Kash Patel as Trump’s FBI director
-

 Indigenous12 hours ago
Indigenous12 hours agoTrudeau gov’t to halt funds for ‘unmarked graves’ search after millions spent, no bodies found
-

 Business1 day ago
Business1 day agoFederal Heritage Minister recommends nearly doubling CBC funding and reducing accountability
-

 Business1 day ago
Business1 day agoArgentina’s Javier Milei gives Elon Musk chainsaw