Health
Red Deer Regional Health Foundation Announces Cath Lab Opening 5 Years Ahead of Schedule

The Red Deer Regional Health Foundation, in collaboration with AHS, is proud to announce the fast-tracked opening of a Cardiac Catheterization Lab (Cath Lab) at Red Deer Regional Hospital Centre.
With a permanent facility scheduled for completion in five years, this critical fixture will allow for care on an accelerated timeline, offering life-saving cardiac care to the residents of Central Alberta.
Manon Therriault, CEO of the Red Deer Regional Health Foundation, emphasized the significance
of this development. “In cardiac care, time isn’t just money—it’s muscle. The earlier patients receive treatment, the better their chances of recovery. This Cath Lab, coming approximately five years earlier than expected, could save up to 160 lives.”
The Cath Lab, which will be housed in a retrofitted space within the current hospital, will allow local cardiac patients to receive urgent care in Red Deer instead of requiring transfers to hospitals in Calgary or Edmonton. In the future, the lab will be transformed into a cutting-edge Vascular and Neurology Lab.
The Red Deer Regional Health Foundation is providing financial support for the essential
architectural, mechanical, and electrical upgrades. “This Cath Lab represents an immediate leap
forward in improving local healthcare. We’re not waiting to make a difference in the lives of Central Albertans,” said Therriault.
“Through this Memorandum of Understanding with our Foundation partners, we’re underscoring our commitment to enhancing the cardiac care available at Red Deer Regional Hospital Centre,” says Karen Foudy, AHS Senior Operating Officer for Red Deer Regional Hospital Centre. “By
establishing an interim catheterization laboratory, we will be able to provide a new service to
patient’s years ahead of the completion of the Red Deer Regional Hospital Centre Redevelopment
Project which will help reduce the need for cardiac patients to travel to other facilities. This will also support our efforts to recruit and retain the talented healthcare professionals needed to provide care every day to our patients.”
2025 Federal Election
MEI-Ipsos poll: 56 per cent of Canadians support increasing access to non-governmental healthcare providers

-
Most believe private providers can deliver services faster than government-run hospitals
-
77 per cent of Canadians say their provincial healthcare system is too bureaucratic
Canadians are increasingly in favour of breaking the government monopoly over health care by opening the door to independent providers and cross-border treatments, an MEI-Ipsos poll has revealed.
“Canadians from coast to coast are signalling they want to see more involvement from independent health providers in our health system,” explains Emmanuelle B. Faubert, economist at the MEI. “They understand that universal access doesn’t mean government-run, and that consistent failures to deliver timely care in government hospitals are a feature of the current system.”
Support for independent health care is on the rise, with 56 per cent of respondents in favour of allowing patients to access services provided by independent health entrepreneurs. Only 25 per cent oppose this.
In Quebec, support is especially strong, with 68 per cent endorsing this change.
Favourable views of accessing care through a mixed system are widespread, with three quarters of respondents stating that private entrepreneurs can deliver healthcare services faster than hospitals managed by the government. This is up four percentage points from last year.
Countries like Sweden and France combine universal coverage with independent providers and deliver faster, more accessible care. When informed about how these health systems run, nearly two in three Canadians favour adopting such models.
The poll also finds that 73 per cent of Canadians support allowing patients to receive treatment abroad with provincial coverage, which could help reduce long wait times at home.
Common in the European Union, this “cross-border directive” enabled 450,000 patients to access elective surgeries in 2022, with costs reimbursed as if they had been treated in their home country.
There’s a growing consensus that provincial healthcare systems are overly bureaucratic, with the strongest agreement in Alberta, B.C., and Quebec. The proportion of Canadians holding this view has risen by 16 percentage points since 2020.
Nor do Canadians see more spending as being a solution: over half say the current pace of healthcare spending in their province is unsustainable.
“Governments shouldn’t keep doubling down on what isn’t working. Instead, they should look at what works abroad,” says Ms. Faubert. “Canadians have made it clear they want to shift gears; now it’s up to policymakers to show they’re listening.”
A sample of 1,164 Canadians aged 18 and older was polled between March 24th and March 28th, 2025. The margin of error is ±3.3 percentage points, 19 times out of 20.
The results of the MEI-Ipsos poll are available here.
* * *
The MEI is an independent public policy think tank with offices in Montreal, Ottawa, and Calgary. Through its publications, media appearances, and advisory services to policymakers, the MEI stimulates public policy debate and reforms based on sound economics and entrepreneurship.
Health
Trump admin directs NIH to study ‘regret and detransition’ after chemical, surgical gender transitioning

From LifeSiteNews
Ample evidence has surfaced in recent years to warrant the White House’s investigation
The Trump administration has made a break with the long-standing government policy of near 100% affirmation of the transgender industry’s efforts and has directed the National Institutes of Health (NIH) to study the negative impacts on mental and physical health of so-called “gender transitioning” on adults and children.
The Department of Health and Human Services (HHS), which oversees NIH, “has been directed to fund research on a few specific areas” regarding “chemical and surgical mutilation” of children and adults,” according to multiple reports.
In particular, the Trump administration wants to investigate “regret and detransition following social transition as well as chemical and surgical mutilation of children and adults” and “outcomes from children who have undergone social transition and/or chemical and surgical mutilation.”
The new directives to the biomedical agency were reportedly included in an email to several NIH directors from then-Acting NIH Director Matthew Memoli shortly after Trump took office.
“This is very important to the President and the Secretary (of HHS, Robert F. Kennedy Jr.),” Memoli wrote.
Unhappy about the Trump administration’s move to uncover the hidden, shadowy side of the burgeoning transgender industry, pro-transgender activists working within the medical research community were quick to criticize the move.
The term “chemical or surgical mutilation” was “deeply offensive,” said Harry Barbee, assistant professor at the Johns Hopkins Bloomberg School of Public Health.
“This terminology has no place in serious scientific or public health discourse,” Barbee complained. “The language has been historically used to stigmatize trans people. Even the phrase(s) ‘regret’ and ‘detransition’ can be weaponized.”
“What they’re looking for is a political answer not a scientific one,” Adrian Shanker, who served as deputy assistant secretary for health policy at HHS under President Biden, told NPR. “That should be an alarm for everyone who cares about the scientific integrity of the National Institutes of Health.”
While those who derive a living focusing on developing and expanding the transgender industry resent the implication that there might be a dark side to their efforts, more than ample evidence has surfaced in recent years to warrant the White House’s investigation on behalf of vulnerable Americans, especially children, who have shown to be highly susceptible to what has been called the “transgender contagion.”
Many oft-ignored detransitioners attest to the physical and mental harm of reinforcing gender confusion as well as to the bias and negligence of the medical establishment on the subject, many of whom take an activist approach to their profession and begin cases with a predetermined conclusion in favor of “transitioning.”
A study published earlier this year in the Oxford Journal of Sexual Medicine found that undergoing sex-change surgery, far from reducing depression rates among the gender dysphoric, substantially increased rates not only of depression but of anxiety, suicidal ideation, and substance use disorders.
This study, along with scores of others conducted in recent years, explodes the media-enforced narrative that so-called “gender affirming” medical treatments are necessary for the happiness and well-being of the gender-confused.
Short video displays deep regret after sex-change treatments and surgery
A short video – just 34 seconds long – displays the extreme distress and anxiety of those who resorted to surgery and hormone treatments to “transition” earlier in their lives, only to experience deep regret later on.
The video presents a cautionary tale, dispelling the myth that parents need to allow their children to transition in order to be happy.
“Society is marketing a horrifically harmful, fashionable new trend to children that brings about a life of depression, confusion, drug use and STD’s,” the caption reads. “Please inform yourselves and help your children.”
Former transgender: ‘Regret’ and ‘detransitioning’ are the new trans frontier
Walt Heyer, a former “transgender woman” who for many years has maintained a global outreach to those who experience sex change regret, has been sounding the alarm about the one-size-fits-all approach of the trans medical industry for years.
“The science of surgical interventions is not yet settled regarding the long-term consequences of transgender therapy,” Heyer noted during a 2017 Symposium at the University of Hong Kong. “As of today, we don’t have any objective, conclusive research.”
“I feel ‘regret’ and ‘detransitioning’ will become the next transgender frontier,” Heyer said. “So be prepared.”
“There is an ever-increasing number of former transgenders, like myself, who are now requesting gender reversals,” he said.
“As a former female transgender, I can see the exploding social trend that has developed into a significant transgender contagion —now even an epidemic— that has captivated young children as well as young adults who have come to believe they’re the opposite sex on just the weight of social media and feelings … in some cases taking drastic measures to change their bodies,” Heyer said.
“More and more, I get reports from families telling me that their teen children suddenly came out as a transgender without any prior history of discomfort with their biological sex,” said Heyer, describing what has come to be called “rapid onset gender dysphoria.”
“Current psychotherapeutic practice involves the immediate affirmation of the young person’s self-diagnosis,” he lamented.
Heyer explained that many surgically transformed men and women suffer from a complex number of sexual, emotional, psychiatric and psychological comorbid disorders such as autogynephilia, dissociative disorders like schizophrenia, body dysmorphic disorder, and a host of other undiagnosed disorders that were not resolved by the recommended therapy of changing genders.
Heyer spoke from his own experience as he explained that if such disorders were considered and treated adequately, sexual transitioning would probably be greatly reduced. The role of these “comorbid” conditions tends to surface later as trans individuals begin to question their decision to transition to the opposite sex.
“We find this out from the ‘regretters,’” Heyer said. “We don’t find it out early on. We find it out afterward when they’re seeking help … and we find out that these comorbid disorders existed early on.”
A significant body of evidence now shows that “affirming” gender confusion carries serious harms, especially when done with impressionable children who lack the mental development, emotional maturity, and life experience to consider the long-term ramifications of the decisions being pushed on them or full knowledge about the long-term effects of life-altering, physically transformative, and often irreversible surgical and chemical procedures.
Studies find that more than 80 percent of children suffering gender dysphoria outgrow it on their own by late adolescence, and that “transition” procedures fail to resolve gender-confused individuals’ heightened tendency to engage in self-harm and suicide – and even exacerbate it, including by reinforcing their confusion and neglecting the actual root causes of their mental strife.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCSIS Warned Beijing Would Brand Conservatives as Trumpian. Now Carney’s Campaign Is Doing It.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoInside Buttongate: How the Liberal Swamp Tried to Smear the Conservative Movement — and Got Exposed
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoIs HNIC Ready For The Winnipeg Jets To Be Canada’s Heroes?
-
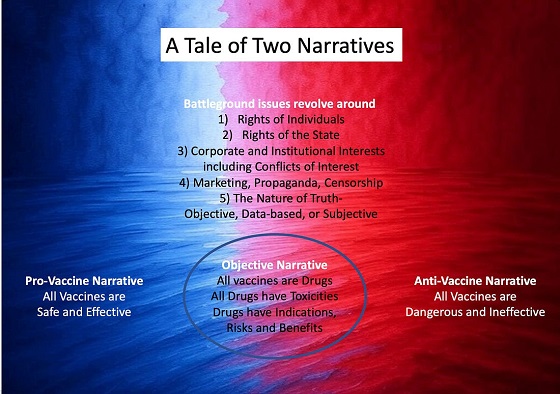
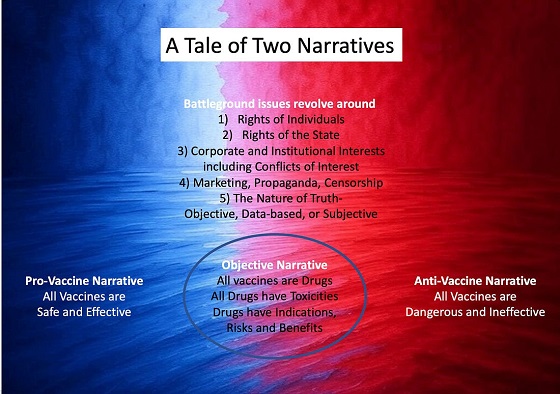 Dr. Robert Malone2 days ago
Dr. Robert Malone2 days agoThe West Texas Measles Outbreak as a Societal and Political Mirror
-

 COVID-191 day ago
COVID-191 day agoCOVID virus, vaccines are driving explosion in cancer, billionaire scientist tells Tucker Carlson
-

 Health2 days ago
Health2 days agoHorrific and Deadly Effects of Antidepressants
-

 illegal immigration1 day ago
illegal immigration1 day agoDespite court rulings, the Trump Administration shows no interest in helping Abrego Garcia return to the U.S.
-

 International2 days ago
International2 days agoTulsi Gabbard tells Trump she has ‘evidence’ voting machines are ‘vulnerable to hackers’