Health
Recovered ‘brain dead’ man dancing at sister’s wedding reminds us organ donors are sometimes alive

TJ Hoover and his sister on her wedding day
From LifeSiteNews
Since brain dead people are not dead, it is not surprising that the only multicenter, prospective study of brain death found that the majority of brains from ‘brain dead’ people were not severely damaged at autopsy.
In 2021, a supposedly brain dead man, Anthony Thomas “TJ” Hoover II, opened his eyes and looked around while being wheeled to the operating room to donate his organs. Hospital staff at Baptist Health hospital in Richmond, Kentucky assured his family that these were just “reflexes.”
But organ preservationist Natasha Miller also thought Hoover looked alive. “He was moving around – kind of thrashing. Like, moving, thrashing around on the bed,” said Miller in an NPR interview. “And then when we went over there, you could see he had tears coming down. He was visibly crying.” Thankfully, the procedure was called off, and Hoover was able to recover and even dance at his sister’s wedding this past summer.
Last month, this case was brought before a U.S. House subcommittee investigating organ procurement organizations. Whistleblowers claimed that even after two doctors refused to remove Hoover’s organs, Kentucky Organ Donor Affiliates ordered their staff to find another doctor to perform the surgery.
Because brain death is a social construct and not death itself, I can tell you exactly how many “brain dead” patients are still alive: all of them. When brain death was first proposed by an ad hoc committee at Harvard Medical School in 1968, the committee admitted that these people are not dead, but rather “desperately injured.” They thought that these neurologically injured people were a burden to themselves and others, and that society would be better served if we redefined them as being “dead.” They described their reasoning this way:
Our primary purpose is to define irreversible coma as a new criterion for death. There are two reasons why there is need for a definition: (1) Improvements in resuscitative and supportive measures have led to increased efforts to save those who are desperately injured. Sometimes these efforts have only partial success so that the result is an individual whose heart continues to beat but whose brain is irreversibly damaged. The burden is great on patients who suffer permanent loss of intellect, on their families, on the hospitals, and on those in need of hospital beds already occupied by these comatose patients. (2) Obsolete criteria for the definition of death can lead to controversy in obtaining organs for transplantation.
Since brain dead people are not dead, it is not surprising that the only multicenter, prospective study of brain death found that the majority of brains from “brain dead” people were not severely damaged at autopsy – and 10 actually looked normal. Dr. Gaetano Molinari, one of the study’s principal investigators, wrote:
[D]oes a fatal prognosis permit the physician to pronounce death? It is highly doubtful whether such glib euphemisms as “he’s practically dead,” … “he can’t survive,” … “he has no chance of recovery anyway,” will ever be acceptable legally or morally as a pronouncement that death has occurred.
But history shows that despite Dr. Molinari’s doubts, “brain death,” a prognosis of possible death, went on to be widely accepted as death per se. Brain death was enshrined into US law in 1981 under the Uniform Determination of Death Act. Acceptance of this law has allowed neurologically disabled people to be redefined as “dead” and used as organ donors. Unfortunately, most of these people do not, like TJ Hoover, wake up in time. They suffer death through the harvesting of their organs, a procedure often performed without the benefit of anesthesia.
Happily, some do manage to avoid becoming organ donors and go on to receive proper medical treatment. In 1985, Jennifer Hamann was thrown into a coma after being given a prescription that was incompatible with her epilepsy medication. She could not move or sign that she was awake and aware when she overheard doctors saying that her husband was being “completely unreasonable” because he would not donate her organs. She went on to made a complete recovery and became a registered nurse.
Zack Dunlap was declared brain dead in 2007 following an ATV accident. Even though his cousin demonstrated that Zack reacted to pain, hospital staff told his family that it was just “reflexes.” But as Zack’s reactions became more vigorous, the staff took more notice and called off the organ harvesting team that was just landing via helicopter to take Zack’s organs. Today, Zack leads a fully recovered life.
Colleen Burns was diagnosed “brain dead” after a drug overdose in 2009, but wasn’t given adequate testing and awoke on the operating table just minutes before her organ harvesting surgery. Because the Burns family declined to sue, the hospital only received a slap on the wrist: the State Health Department fined St. Joseph’s Hospital Health Center in Syracuse, New York, just $6,000.
In 2015, George Pickering III was declared brain dead, but his father thought doctors were moving too fast. Armed and dangerous, he held off a SWAT team for three hours, during which time his son began to squeeze his hand on command. “There was a law broken, but it was broken for all the right reasons. I’m here now because of it,” said George III.
Trenton McKinley, a 13-year-old boy, suffered a head injury in 2018 but regained consciousness after his parents signed paperwork to donate his organs. His mother told CBS News that signing the consent to donate allowed doctors to continue Trenton’s intensive care treatment, ultimately giving him time to wake up.
Doctors often say that cases like these prove nothing, and that they are obviously the result of misdiagnosis and medical mistakes. But since all these people were about to become organ donors regardless of whether their diagnoses were correct, I doubt they find the “mistake” excuse comforting.
However, Jahi McMath was indisputably diagnosed as being “brain dead” correctly. She was declared brain dead by three different doctors, she failed three apnea tests, and she had four flat-line EEGs, as well as a cerebral perfusion scan showing “no flow.” But because her parents refused to make her an organ donor and insisted on continuing her medical care, McMath recovered to the point of being able to follow commands. Two neurologists later testified that she was no longer brain dead, but a in minimally conscious state. Her case shows that people correctly declared “brain dead” can still recover.
READ: Woman with no brainwave activity wakes up after hearing her daughter’s voice
Brain death is not death because the brain death concept does not reflect the reality of the phenomenon of death. Therefore, any guideline for its diagnosis will have no basis in scientific facts. People declared brain dead are neurologically disabled, but they are still alive. “Brain dead” organ donation is a concealed form of euthanasia.
Heidi Klessig MD is a retired anesthesiologist and pain management specialist who writes and speaks on the ethics of organ harvesting and transplantation. She is the author of “The Brain Death Fallacy” and her work may be found at respectforhumanlife.com.
Daily Caller
Daily Caller EXCLUSIVE: Trump’s Broad Ban On Risky Gain-Of-Function Research Nears Completion


From the Daily Caller News Foundation
By Emily Kopp
President Donald Trump could sign a sweeping executive order banning gain-of-function research — research that makes viruses more dangerous in the lab — as soon as May 6, according to a source who has worked with the National Security Council on the issue.
The executive order will take a broad strokes approach, banning research amplifying the infectivity or pathogenicity of any virulent and replicable pathogen, according to the source, who requested anonymity to speak candidly about the anticipated executive action. But significant unresolved issues remain, according to the source, including whether violators will be subject to criminal penalties as bioweaponeers.
The executive order is being steered by Gerald Parker, head of the White House Office of Pandemic Preparedness and Response Policy, which has been incorporated into the NSC. Parker did not respond to requests for comment.
Dear Readers:
As a nonprofit, we are dependent on the generosity of our readers.
Please consider making a small donation of any amount here. Thank you!
In the process of drafting the executive order, Parker has frozen out the federal agencies that have for years championed gain-of-function research and staved off regulation — chiefly Anthony Fauci’s former institute, the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
The latest policy guidance on gain-of-function research, unveiled under the Biden administration in 2024, was previously expected to go into effect May 6. According to a March 25 letter cosigned by the American Society for Microbiology, the Association for Biosafety and Biosecurity International, and Council on Governmental Relations, organizations that conduct pathogen research have not received direction from the NIH on that guidance — suggesting the executive order would supersede the May 6 deadline.
The 2024 guidance altered the scope of experiments subject to more rigorous review, but charged researchers, universities and funding agencies like NIH with its implementation, which critics say disincentivizes reporting. Many scientists say that researchers and NIH should not be the primary entities conducting cost–benefit analyses of pandemic virus studies.
Parker previously served as the head of the National Science Advisory Board for Biosecurity (NSABB), a group of outside experts that advises NIH on biosecurity matters, and in that role recommended that Congress stand up a new government agency to advise on gain-of-function research. Former Centers for Disease Control and Prevention Director Robert Redfield has also endorsed moving gain-of-function research decision making out of the NIH to an independent commission.
“Given the well documented lapses in the NIH review process, policymakers should … remove final approval of any gain-of function research grants from NIH,” Redfield said in a February op-ed.
It remains to be seen whether the executive order will articulate carveouts for gain-of-function research without risks of harm such as research on non-replicative pseudoviruses, which can be used to study viral evolution without generating pandemic viruses.
It also remains to be seen whether the executive order will define “gain-of-function research” tightly enough to stand up to legal scrutiny should a violator be charged with a crime.
Risky research on coronaviruses funded by the NIH at the Wuhan Institute of Virology through the U.S. nonprofit EcoHealth Alliance typifies the loopholes in NIH’s existing regulatory framework, some biosecurity experts say.
Documents obtained through the Freedom of Information Act in 2023 indicated that EcoHealth Alliance President Peter Daszak submitted a proposal to the Pentagon in 2018 called “DEFUSE” describing gain-of-function experiments on viruses similar to SARS-CoV-2 but downplayed to his intended funder the fact that many of the tests would occur in Wuhan, China.
Daszak and EcoHealth were both debarred from federal funding in January 2025 but have faced no criminal charges.
“I don’t know that criminal penalties are necessary. But we do need more sticks in biosafety as well as carrots,” said a biosecurity expert who requested anonymity to avoid retribution from his employer for weighing in on the expected policy. “For instance, biosafety should be a part of tenure review and whether you get funding for future work.”
Some experts say that it is likely that the COVID-19 crisis was a lab-generated pandemic, and that without major policy changes it might not be the last one.
“Gain-of-function research on potential pandemic pathogens caused the COVID-19 pandemic, killing 20 million and costing $25 trillion,” said Richard Ebright, a Rutgers University microbiologist and longtime critic of high-risk virology, to the Daily Caller News Foundation. “If not stopped, gain-of-function research on potential pandemic pathogens likely will cause future lab-generated pandemics.”
Health
WHO member states agree on draft of ‘pandemic treaty’ that could be adopted in May

From LifeSiteNews
The WHO draft ‘pandemic accord’ includes data sharing between governments and pharmaceutical companies to develop ‘pandemic-related health products,’ though it would not apply to the US.
Representatives of WHO member states have agreed on a draft of the “pandemic accord” that is scheduled to be voted on next month.
“The nations of the world made history in Geneva today,” Dr. Tedros Adhanom Ghebreyesus, Director-General of the WHO, said after the member states agreed on the draft of the pandemic treaty on Wednesday.
“In reaching consensus on the Pandemic Agreement, not only did they put in place a generational accord to make the world safer, they have also demonstrated that multilateralism is alive and well, and that in our divided world, nations can still work together to find common ground, and a shared response to shared threats. I thank WHO’s Member States, and their negotiating teams, for their foresight, commitment and tireless work. We look forward to the World Health Assembly’s consideration of the agreement and – we hope – its adoption,” the WHO leader continued.
The agreement was reached by the Intergovernmental Negotiating Body (INB), the committee set up by the WHO to negotiate the treaty, after more than three years of negotiations.
According to the WHO’s press release, the core pandemic treaty draft includes the establishment of “a pathogen access and benefit sharing system,” allowing the sharing of data between governments and pharmaceutical companies aimed at quickly developing and supplying “pandemic-related health products” during a pandemic. These “health products” could be dangerous mRNA injections, similar to those rolled out and imposed on large parts of the world population during the COVID-19 crisis.
The WHO claims that the “proposal affirms the sovereignty of countries to address public health matters within their borders, and provides that nothing in the draft agreement shall be interpreted as providing WHO any authority to direct, order, alter or prescribe national laws or policies, or mandate States to take specific actions, such as ban or accept travellers, impose vaccination mandates or therapeutic or diagnostic measures or implement lockdowns.”
The WHO seems to be responding to critics of the Pandemic Treaty, who have argued it is a power grab by the WHO. It would give the global organization unchecked power whenever it declares that any health risk is a “pandemic.” However, the new draft has not yet been made public, making a thorough assessment impossible.
WHO director-general Ghebreyesus engaged in his typical fear-mongering, stating, “Virus is the worst enemy. (It) could be worse than a war.”
READ: WHO director Tedros calls for ‘more aggressive’ action against COVID shot critics
While the WHO pandemic treaty and the amendments to the International Health Regulations (IHR) failed to pass last year, the new version of the agreement could be passed by a two-thirds majority at the annual World Health Assembly (May 19-27, 2025) next month.
However, the U.S. was not part of the negotiations and would not be bound by the agreement since President Donald Trump withdrew the country from the international body in January 2025 after taking office for his second term. Argentine President Javier Milei announced in February that his country will also leave the WHO, following Trump’s example. If more countries were to leave the WHO, the pandemic agreement could be ineffective in practice, even if it were to pass in May.
-

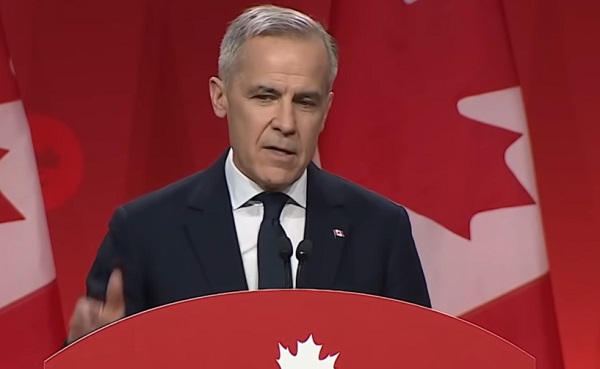
 2025 Federal Election2 days ago
2025 Federal Election2 days agoRCMP Whistleblowers Accuse Members of Mark Carney’s Inner Circle of Security Breaches and Surveillance
-

 Also Interesting2 days ago
Also Interesting2 days agoBetFury Review: Is It the Best Crypto Casino?
-
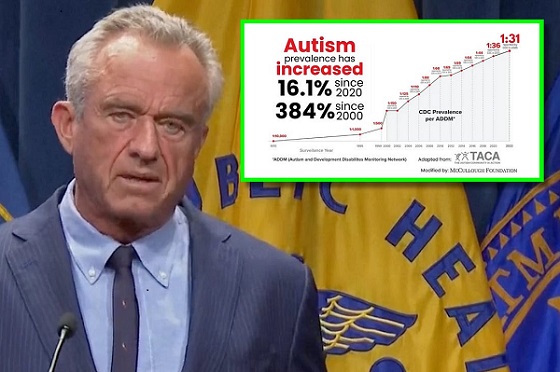
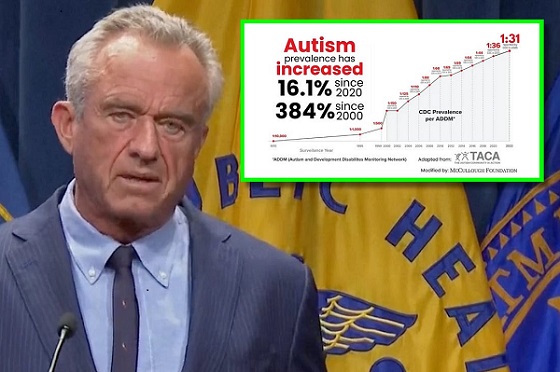 Autism2 days ago
Autism2 days agoRFK Jr. Exposes a Chilling New Autism Reality
-

 COVID-192 days ago
COVID-192 days agoCanadian student denied religious exemption for COVID jab takes tech school to court
-

 International2 days ago
International2 days agoUK Supreme Court rules ‘woman’ means biological female
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoBureau Exclusive: Chinese Election Interference Network Tied to Senate Breach Investigation
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoNeil Young + Carney / Freedom Bros
-

 Health2 days ago
Health2 days agoWHO member states agree on draft of ‘pandemic treaty’ that could be adopted in May