Alberta
Province says improving primary health care system will take pressure off emergency care
Strengthening health care: Improving access for all
Alberta’s government is stabilizing and strengthening primary health care across the province so that everyone can access care when and where they need it.
Primary health care is the first point of contact Albertans have with the health care system, and includes health professionals such as family doctors, nurse practitioners and pharmacists.
Last fall, health care leaders, Indigenous partners and experts from across Canada and around the world came together to form advisory panels as part of the Modernizing Alberta’s Primary Health Care System (MAPS) initiative. The panels identified immediate, medium- and long-term improvements to strengthen Alberta’s primary health care system.
Alberta’s government will begin moving forward on the recommendations in the final report to improve access to primary health care for all Albertans. The recommendations will be implemented through a phased approach, with several moving forward immediately, followed by medium- and longer-term improvements that will enhance community-based primary health care across Alberta.
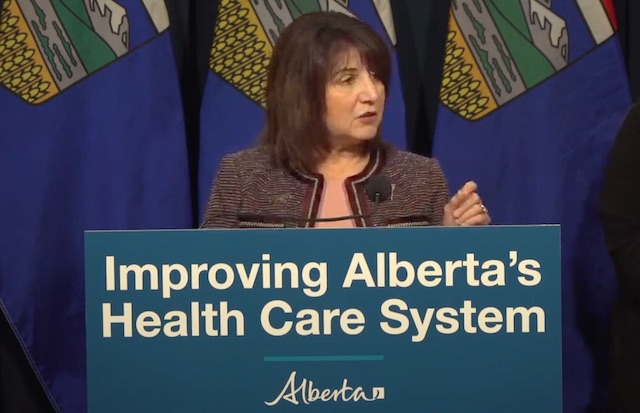
“Today marks an important step in the work I am undertaking to enhance primary care as the foundation of our health care system. The Modernizing Alberta’s Primary Health Care System (MAPS) reports clearly identify the challenges our system is facing, and their release signals this government’s commitment to take immediate and ongoing action to support and stabilize primary health care in our province. I look forward to the ongoing work of implementing needed changes with our health care partners and providers.”
Several immediate actions are being taken, all of which are consistent with recommendations from the panels. These actions are critical to ensuring Albertans have better access to health care when and where they need it. Alberta Health continues to work toward implementing recommendations over the medium and long term.
“The MAPS recommendations represent a huge leap forward for our primary health system – strengthening and clarifying governance, community involvement, and recognizing the importance of integrated team-based care that allows Albertans to access primary care from the most appropriate team member at the right time, in the right place. This is how we can ensure equitable access to care across our province.”
Strengthening primary health care
Alberta’s government is acting immediately on recommendations to improve primary health care and increase Albertans’ access to the medical care they need, including:
- Creating a primary health care division within Alberta Health.
- Allocating $57 million over three years to provide family doctors and nurse practitioners with support to help manage their increasing number of patients. Each provider has the potential to receive up to $10,000 annually.
- Working with the Alberta Medical Association to create a task force to recommend a new payment model for family physicians that encourages comprehensive primary care – where a patient has a regular family doctor who they develop a long-term relationship with and who works with them to ensure all their health care needs are met.
- Developing a memorandum of understanding with the Alberta Medical Association to collaborate on a transition to a new physician compensation model, modernize primary care governance and enable family doctors to spend more time with patients and less time on paperwork and immediately stabilize primary care.
- Expanding online mental health services, allowing doctors to bill for virtual mental health checks and therapy, and compensating them for extra time spent with patients virtually.
- Ensuring doctors get paid if patients can’t prove insurance coverage, reducing administrative burden. This is known as “good faith” claims.
- Introducing a payment system that will support nurse practitioners to open their own clinics, take on patients and offer services based on their scope of practice, training and expertise. Nurse practitioners have completed graduate studies ensuring that they are properly trained to examine patients, provide diagnoses and prescribe medication.
“We know that a strong primary health care system is foundational for better health care for Albertans, and that starts with access to a family physician and a team of dedicated providers. Primary care requires dedicated planning, resourcing and coordination. We are pleased to join the task force and believe continued collaboration and immediate action will bring us closer to our collective vision.”
“The Nurse Practitioner Association of Alberta is elated to see the newly released MAPs report, which provides direction for primary care reform and includes the full integration of nurse practitioners. The Government of Alberta is taking a significant and essential step in improving access to primary care for Albertans. This announcement is a win-win for Albertans and nurse practitioners, as it recognizes the valuable contributions of NPs delivering high-quality care for Albertans and their ability to decrease the stress on the health care system. We are excited about the future of primary care in Alberta.”
“These actions are welcome news for rural Alberta. Ensuring Albertans have access to health care professionals when and where they need it is essential. This work will help to solve some of the unique challenges for rural Albertans by encouraging health professions to practise in rural parts of the province.”
Strengthening Indigenous health care
Indigenous Peoples face many barriers to access appropriate health care. To support better health outcomes, the government will build more meaningful connections with Indigenous leaders and communities to identify improvements that reflect the unique nature of their communities. Immediate actions include:
- Creating an Indigenous health division within Alberta Health.
- Creating a $20-million fund for Indigenous communities to design and deliver innovative primary health care services and projects.
- Creating an Indigenous patient complaints investigator and Elders roster to investigate incidences of racism during the delivery of health care and provide culturally safe support to Indigenous patients throughout the patient complaint process.
- Investing in a community-based Indigenous patient navigator program to support Indigenous peoples throughout their health care journey.
“It is unacceptable that Indigenous Peoples continue to face so many barriers when accessing primary health care. It is crucial that all First Nations, Métis and Inuit peoples have equitable access to community-based primary health care that is culturally safe, respects their unique needs and is free of racism. These immediate actions will help us achieve that goal.”
“The panel’s recommendations provide a clear and stable pathway to create a safe, culturally appropriate primary health care system that includes Indigenous people as partners and leaders at every stage of the development, governance and delivery of health care services. The best solutions exist within our respective communities, tailored for our unique needs and priorities. The commitments made today are an important first step toward improving health equity for Indigenous Peoples, regardless of where they live in Alberta.”
Quick facts
- Advisory panels were established through MAPS in fall 2022 to identify primary health care improvements in the short term and over the next 10 years.
- Final reports from the panels were submitted in spring 2023.
- The strategic advisory panel final report contains 11 recommendations to refocus the system around primary health care with an emphasis on:
- access to team-based care
- integration between primary health care and community care
- a foundation of a coordinated and accountable primary health care system
- The Indigenous advisory panel final report contains 22 recommendations under five themes:
- improve health equity for Indigenous Peoples
- address Indigenous racism in health care
- build culturally safer primary health care and an Indigenous workforce
- create system innovation and support community capacity
- Indigenous ownership, stewardship, design and delivery of health care services
- Budget 2023 allocated $125 million over three years to implement recommendations from MAPS.
- The next step will be to further engage with health care partners, including Indigenous communities, to implement these immediate priorities and the broader MAPS recommendations.
Related information
Alberta
Alberta project would be “the biggest carbon capture and storage project in the world”

Pathways Alliance CEO Kendall Dilling is interviewed at the World Petroleum Congress in Calgary, Monday, Sept. 18, 2023.THE CANADIAN PRESS/Jeff McIntosh
From Resource Works
Carbon capture gives biggest bang for carbon tax buck CCS much cheaper than fuel switching: report
Canada’s climate change strategy is now joined at the hip to a pipeline. Two pipelines, actually — one for oil, one for carbon dioxide.
The MOU signed between Ottawa and Alberta two weeks ago ties a new oil pipeline to the Pathways Alliance, which includes what has been billed as the largest carbon capture proposal in the world.
One cannot proceed without the other. It’s quite possible neither will proceed.
The timing for multi-billion dollar carbon capture projects in general may be off, given the retreat we are now seeing from industry and government on decarbonization, especially in the U.S., our biggest energy customer and competitor.
But if the public, industry and our governments still think getting Canada’s GHG emissions down is a priority, decarbonizing Alberta oil, gas and heavy industry through CCS promises to be the most cost-effective technology approach.
New modelling by Clean Prosperity, a climate policy organization, finds large-scale carbon capture gets the biggest bang for the carbon tax buck.
Which makes sense. If oil and gas production in Alberta is Canada’s single largest emitter of CO2 and methane, it stands to reason that methane abatement and sequestering CO2 from oil and gas production is where the biggest gains are to be had.
A number of CCS projects are already in operation in Alberta, including Shell’s Quest project, which captures about 1 million tonnes of CO2 annually from the Scotford upgrader.
What is CO2 worth?
Clean Prosperity estimates industrial carbon pricing of $130 to $150 per tonne in Alberta and CCS could result in $90 billion in investment and 70 megatons (MT) annually of GHG abatement or sequestration. The lion’s share of that would come from CCS.
To put that in perspective, 70 MT is 10% of Canada’s total GHG emissions (694 MT).
The report cautions that these estimates are “hypothetical” and gives no timelines.
All of the main policy tools recommended by Clean Prosperity to achieve these GHG reductions are contained in the Ottawa-Alberta MOU.
One important policy in the MOU includes enhanced oil recovery (EOR), in which CO2 is injected into older conventional oil wells to increase output. While this increases oil production, it also sequesters large amounts of CO2.
Under Trudeau era policies, EOR was excluded from federal CCS tax credits. The MOU extends credits and other incentives to EOR, which improves the value proposition for carbon capture.
Under the MOU, Alberta agrees to raise its industrial carbon pricing from the current $95 per tonne to a minimum of $130 per tonne under its TIER system (Technology Innovation and Emission Reduction).
The biggest bang for the buck
Using a price of $130 to $150 per tonne, Clean Prosperity looked at two main pathways to GHG reductions: fuel switching in the power sector and CCS.
Fuel switching would involve replacing natural gas power generation with renewables, nuclear power, renewable natural gas or hydrogen.
“We calculated that fuel switching is more expensive,” Brendan Frank, director of policy and strategy for Clean Prosperity, told me.
Achieving the same GHG reductions through fuel switching would require industrial carbon prices of $300 to $1,000 per tonne, Frank said.
Clean Prosperity looked at five big sectoral emitters: oil and gas extraction, chemical manufacturing, pipeline transportation, petroleum refining, and cement manufacturing.
“We find that CCUS represents the largest opportunity for meaningful, cost-effective emissions reductions across five sectors,” the report states.

Fuel switching requires higher carbon prices than CCUS.
Measures like energy efficiency and methane abatement are included in Clean Prosperity’s calculations, but again CCS takes the biggest bite out of Alberta’s GHGs.
“Efficiency and (methane) abatement are a portion of it, but it’s a fairly small slice,” Frank said. “The overwhelming majority of it is in carbon capture.”

From left, Alberta Minister of Energy Marg McCuaig-Boyd, Shell Canada President Lorraine Mitchelmore, CEO of Royal Dutch Shell Ben van Beurden, Marathon Oil Executive Brian Maynard, Shell ER Manager, Stephen Velthuizen, and British High Commissioner to Canada Howard Drake open the valve to the Quest carbon capture and storage facility in Fort Saskatchewan Alta, on Friday November 6, 2015. Quest is designed to capture and safely store more than one million tonnes of CO2 each year an equivalent to the emissions from about 250,000 cars. THE CANADIAN PRESS/Jason Franson
Credit where credit is due
Setting an industrial carbon price is one thing. Putting it into effect through a workable carbon credit market is another.
“A high headline price is meaningless without higher credit prices,” the report states.
“TIER credit prices have declined steadily since 2023 and traded below $20 per tonne as of November 2025. With credit prices this low, the $95 per tonne headline price has a negligible effect on investment decisions and carbon markets will not drive CCUS deployment or fuel switching.”
Clean Prosperity recommends a kind of government-backstopped insurance mechanism guaranteeing carbon credit prices, which could otherwise be vulnerable to political and market vagaries.
Specifically, it recommends carbon contracts for difference (CCfD).
“A straight-forward way to think about it is insurance,” Frank explains.
Carbon credit prices are vulnerable to risks, including “stroke-of-pen risks,” in which governments change or cancel price schedules. There are also market risks.
CCfDs are contractual agreements between the private sector and government that guarantees a specific credit value over a specified time period.
“The private actor basically has insurance that the credits they’ll generate, as a result of making whatever low-carbon investment they’re after, will get a certain amount of revenue,” Frank said. “That certainty is enough to, in our view, unlock a lot of these projects.”
From the perspective of Canadian CCS equipment manufacturers like Vancouver’s Svante, there is one policy piece still missing from the MOU: eligibility for the Clean Technology Manufacturing (CTM) Investment tax credit.
“Carbon capture was left out of that,” said Svante co-founder Brett Henkel said.
Svante recently built a major manufacturing plant in Burnaby for its carbon capture filters and machines, with many of its prospective customers expected to be in the U.S.
The $20 billion Pathways project could be a huge boon for Canadian companies like Svante and Calgary’s Entropy. But there is fear Canadian CCS equipment manufacturers could be shut out of the project.
“If the oil sands companies put out for a bid all this equipment that’s needed, it is highly likely that a lot of that equipment is sourced outside of Canada, because the support for Canadian manufacturing is not there,” Henkel said.
Henkel hopes to see CCS manufacturing added to the eligibility for the CTM investment tax credit.
“To really build this eco-system in Canada and to support the Pathways Alliance project, we need that amendment to happen.”
Resource Works News
Alberta
The Canadian Energy Centre’s biggest stories of 2025

From the Canadian Energy Centre
Canada’s energy landscape changed significantly in 2025, with mounting U.S. economic pressures reinforcing the central role oil and gas can play in safeguarding the country’s independence.
Here are the Canadian Energy Centre’s top five most-viewed stories of the year.
5. Alberta’s massive oil and gas reserves keep growing – here’s why

The Northern Lights, aurora borealis, make an appearance over pumpjacks near Cremona, Alta., Thursday, Oct. 10, 2024. CP Images photo
Analysis commissioned this spring by the Alberta Energy Regulator increased the province’s natural gas reserves by more than 400 per cent, bumping Canada into the global top 10.
Even with record production, Alberta’s oil reserves – already fourth in the world – also increased by seven billion barrels.
According to McDaniel & Associates, which conducted the report, these reserves are likely to become increasingly important as global demand continues to rise and there is limited production growth from other sources, including the United States.
4. Canada’s pipeline builders ready to get to work
Canada could be on the cusp of a “golden age” for building major energy projects, said Kevin O’Donnell, executive director of the Mississauga, Ont.-based Pipe Line Contractors Association of Canada.
That eagerness is shared by the Edmonton-based Progressive Contractors Association of Canada (PCA), which launched a “Let’s Get Building” advocacy campaign urging all Canadian politicians to focus on getting major projects built.
“The sooner these nation-building projects get underway, the sooner Canadians reap the rewards through new trading partnerships, good jobs and a more stable economy,” said PCA chief executive Paul de Jong.
3. New Canadian oil and gas pipelines a $38 billion missed opportunity, says Montreal Economic Institute

Steel pipe in storage for the Trans Mountain Pipeline expansion in 2022. Photo courtesy Trans Mountain Corporation
In March, a report by the Montreal Economic Institute (MEI) underscored the economic opportunity of Canada building new pipeline export capacity.
MEI found that if the proposed Energy East and Gazoduq/GNL Quebec projects had been built, Canada would have been able to export $38 billion worth of oil and gas to non-U.S. destinations in 2024.
“We would be able to have more prosperity for Canada, more revenue for governments because they collect royalties that go to government programs,” said MEI senior policy analyst Gabriel Giguère.
“I believe everybody’s winning with these kinds of infrastructure projects.”
2. Keyera ‘Canadianizes’ natural gas liquids with $5.15 billion acquisition

Keyera Corp.’s natural gas liquids facilities in Fort Saskatchewan, Alta. Photo courtesy Keyera Corp.
In June, Keyera Corp. announced a $5.15 billion deal to acquire the majority of Plains American Pipelines LLP’s Canadian natural gas liquids (NGL) business, creating a cross-Canada NGL corridor that includes a storage hub in Sarnia, Ontario.
The acquisition will connect NGLs from the growing Montney and Duvernay plays in Alberta and B.C. to markets in central Canada and the eastern U.S. seaboard.
“Having a Canadian source for natural gas would be our preference,” said Sarnia mayor Mike Bradley.
“We see Keyera’s acquisition as strengthening our region as an energy hub.”
1. Explained: Why Canadian oil is so important to the United States

Enbridge’s Cheecham Terminal near Fort McMurray, Alberta is a key oil storage hub that moves light and heavy crude along the Enbridge network. Photo courtesy Enbridge
The United States has become the world’s largest oil producer, but its reliance on oil imports from Canada has never been higher.
Many refineries in the United States are specifically designed to process heavy oil, primarily in the U.S. Midwest and U.S. Gulf Coast.
According to the Alberta Petroleum Marketing Commission, the top five U.S. refineries running the most Alberta crude are:
- Marathon Petroleum, Robinson, Illinois (100% Alberta crude)
- Exxon Mobil, Joliet, Illinois (96% Alberta crude)
- CHS Inc., Laurel, Montana (95% Alberta crude)
- Phillips 66, Billings, Montana (92% Alberta crude)
- Citgo, Lemont, Illinois (78% Alberta crude)
-

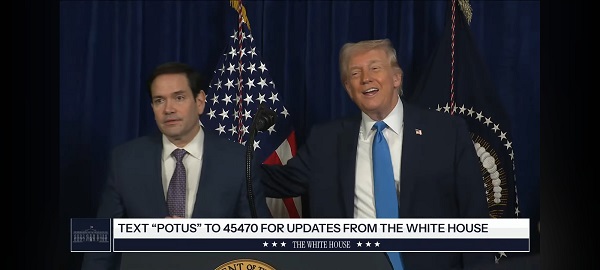
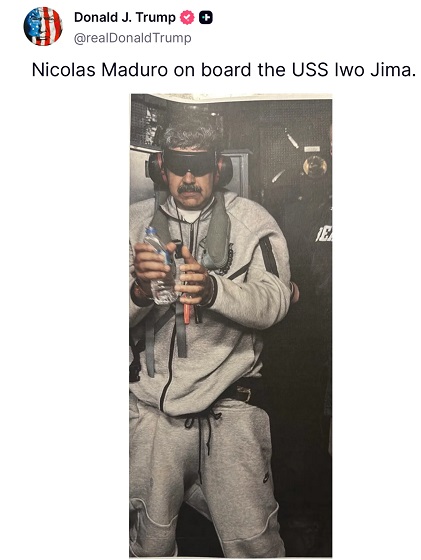
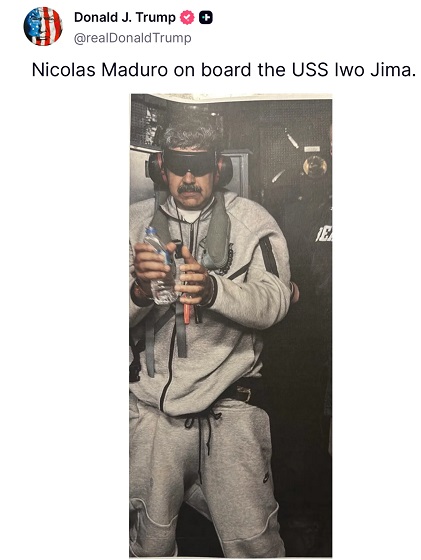
 International2 days ago
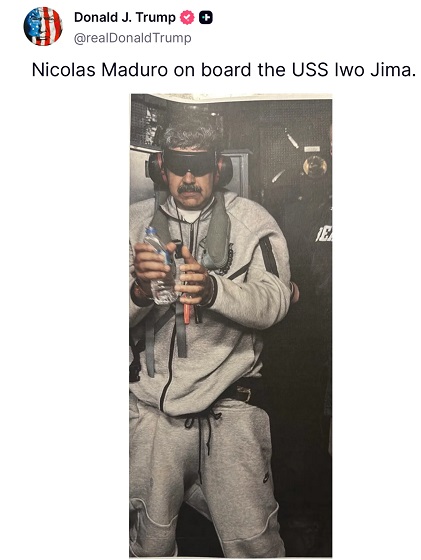
International2 days ago“Captured and flown out”: Trump announces dramatic capture of Maduro
-

 International2 days ago
International2 days agoTrump Says U.S. Strike Captured Nicolás Maduro and Wife Cilia Flores; Bondi Says Couple Possessed Machine Guns
-

 Energy1 day ago
Energy1 day agoThe U.S. Just Removed a Dictator and Canada is Collateral Damage
-
 International1 day ago
International1 day agoUS Justice Department Accusing Maduro’s Inner Circle of a Narco-State Conspiracy
-

 Haultain Research1 day ago
Haultain Research1 day agoTrying to Defend Maduro’s Legitimacy
-

 Business2 days ago
Business2 days agoVacant Somali Daycares In Viral Videos Are Also Linked To $300 Million ‘Feeding Our Future’ Fraud
-
 Daily Caller22 hours ago
Daily Caller22 hours agoTrump Says US Going To Run Venezuela After Nabbing Maduro
-
 International1 day ago
International1 day agoU.S. Claims Western Hemispheric Domination, Denies Russia Security Interests On Its Own Border




