Health
Primary Care Network offers all kinds of services for bolstering health and wellness

The Primary Care Network offers a tremendous range of programming all geared to helping folks live their healthiest lives.
Staff at the local office, located at 5120 47 St., are excited about launching into 2022 with a spectrum of workshops from Anxiety to Calm, Happiness Basics and Moving on With Persistent Pain to Relationships in Motion, Sleep and Journey Through Grief.
Others include My Way to Health (formerly Health Basics), Strong and Steady (which focuses on bolstering one’s strength and flexibility), and H.E.A.R.T.S which has been carefully designed to help families through the loss of a child during pregnancy or shortly after birth.
Of course, due to the pandemic, programming has been virtually all online. But there has been a silver lining with that approach, explained Lorna Milkovich, executive director.
“With our group workshops, we discovered that with going online, we were able to reach some people that we may not have reached otherwise. For some, being able to attend via Zoom offered new flexibility. Others were more comfortable with that format over in-person meetings.” Moving forward, group workshops will certainly continue to be offered in-person, but the PCN will also continue with online versions as well. “That’s exciting, because it opens the door to reaching a wider demographic.
“Through the online versions, we continued to evaluate things and receive feedback, and we continue to see really amazing results. For Anxiety to Calm for example, it consistently shows that people reduce their anxiety, on average, by 50 per cent,” she explained. “It’s amazing.” As for the programs, Milkovich noted that the popular workshop Health Basics has been re-launched as My Way to Health. “It’s a very core workshop that we would encourage most people to take,” she said, adding the sessions focus on healthy living habits including weight loss, bolstering activity and assisting with chronic pain and maintaining a healthy brain through the ageing process. Essentially, participants will learn a host of practical skills they can put into action, said Milkovich.
“It’s super important that people can make changes that are meaningful to them, and that work with their lifestyles.”
There is always an emphasis on designing the workshops to be primarily skills-based, interactive and experiential. “It’s really about, how do you incorporate these skills into your life?

“With each one of our workshops, you will learn new skills that you are going to practice that week to see how they work for you. By the end, you will have four or five new skills and you’ll find those that really resonate with you; ones that work for you,” she said. “That’s what we find that really works for people.”
In a move to make the workshops even more accessible, Milkovich said many are available in both four and eight- week sessions.
“We are also starting up the workshops every month,” she said. This way, there are no lengthy waiting periods should someone miss out on signing up during a given week.
Another exciting new tool this year is the introduction of a downloadable publication called My Self-Care Journey.
“It’s a journal that is available on our web site. It was designed by several health care professionals as well as patients and other members of the community. The journal is about choosing healthy habits each day, and it helps you intentionally tune into your lifestyle choices – it provides a guide for making positive changes,” she said, adding that there are sections on mindfulness and gratitude as well. Ultimately, solid lifestyle changes typically come from making smaller, more manageable goals, said Milkovich.
“it’s more about those tiny little building blocks in your lifestyle that can make a difference. It’s also about people being kinder and gentler with themselves while building healthier lifestyles.”
“My Self-Care Journey is available to anyone – they can go online and print it off. For those who would prefer a hard copy, they can ask at their doctor’s office, or they can swing by the Primary Care Network. There is no charge.”
Looking ahead, the next Health Café is slated for March 14 and is entitled ‘Gout – Disease of the Kings’. Presented by PCN staff, folks are invited to learn more about this condition and ways to help manage it. Tune in live on the Red Deer Public Library Facebook page at 5:15 p.m. Milkovich said staff are always open to preparing Health Cafes on topics of interest to the public at large. “They can let us know – we’d be happy to hear from them,” she said. Several individual programs are available as well via the PCN, from help with diabetes, blood pressure and cholesterol to pharmacy queries to assistance with everything from quitting smoking to learning more about housing or financing. Milkovich also highlighted a relatively new program called the MINT Memory Clinic which is available with a referral from a family doctor. Folks are taken through a full assessment and provided with recommendations for ongoing care and connection with specialists.

As Milkovich pointed out, the PCN is also a hub for those seeking information about health and wellness resources in the community. Besides the workshops, health cafes and personal appointments, they can help point folks in the right direction for the best kind of assistance they may need.
“We want to help empower people to live the healthiest lives that they can,” she said, adding that it’s always so amazing to see people make terrific changes in their daily lives.
“We do get stories from people, and it is so inspiring to see the differences that have been made in their lives.”
For more about the PCN, check out reddeerpcn.com or find them on Facebook for all the latest news as well. You can also call the office at 403-343-9100.
Click here to read other stories from the Red Deer Primary Care Network.
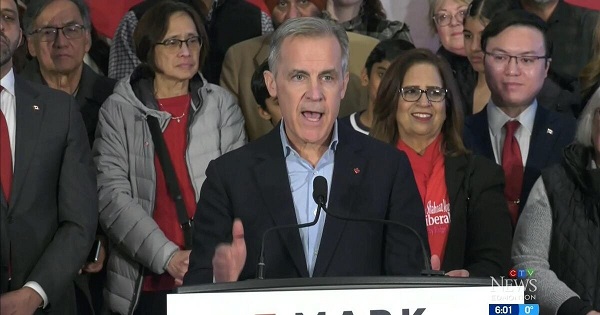
2025 Federal Election
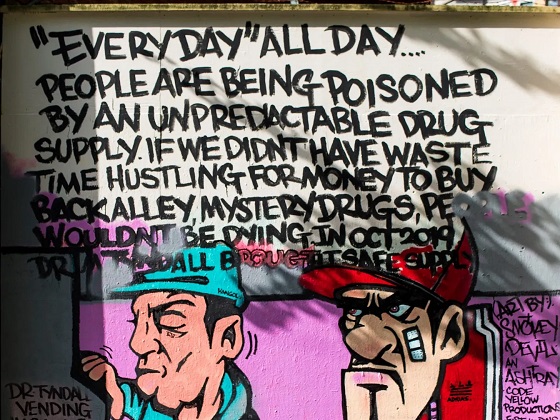
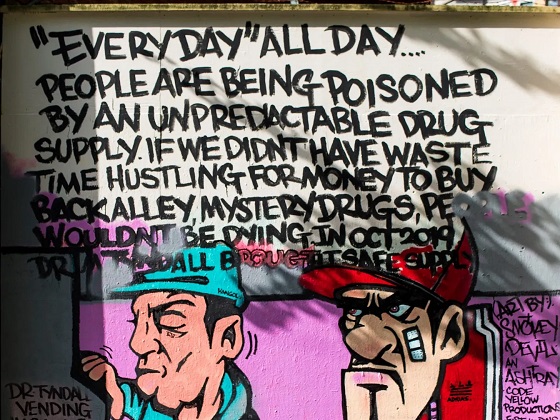
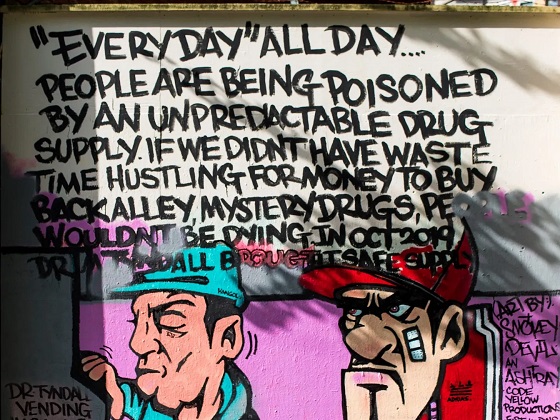
Study links B.C.’s drug policies to more overdoses, but researchers urge caution
By Alexandra Keeler
A study links B.C.’s safer supply and decriminalization to more opioid hospitalizations, but experts note its limitations
A new study says B.C.’s safer supply and decriminalization policies may have failed to reduce overdoses. Furthermore, the very policies designed to help drug users may have actually increased hospitalizations.
“Neither the safer opioid supply policy nor the decriminalization of drug possession appeared to mitigate the opioid crisis, and both were associated with an increase in opioid overdose hospitalizations,” the study says.
The study has sparked debate, with some pointing to it as proof that B.C.’s drug policies failed. Others have questioned the study’s methodology and conclusions.
“The question we want to know the answer to [but cannot] is how many opioid hospitalizations would have occurred had the policy not have been implemented,” said Michael Wallace, a biostatistician and associate professor at the University of Waterloo.
“We can never come up with truly definitive conclusions in cases such as this, no matter what data we have, short of being able to magically duplicate B.C.”
Jumping to conclusions
B.C.’s controversial safer supply policies provide drug users with prescription opioids as an alternative to toxic street drugs. Its decriminalization policy permitted drug users to possess otherwise illegal substances for personal use.
The peer-reviewed study was led by health economist Hai Nguyen and conducted by researchers from Memorial University in Newfoundland, the University of Manitoba and Weill Cornell Medicine, a medical school in New York City. It was published in the medical journal JAMA Health Forum on March 21.
The researchers used a statistical method to create a “synthetic” comparison group, since there is no ideal control group. The researchers then compared B.C. to other provinces to assess the impact of certain drug policies.
Examining data from 2016 to 2023, the study links B.C.’s safer supply policies to a 33 per cent rise in opioid hospitalizations.
The study says the province’s decriminalization policies further drove up hospitalizations by 58 per cent.
“Neither the safer supply policy nor the subsequent decriminalization of drug possession appeared to alleviate the opioid crisis,” the study concludes. “Instead, both were associated with an increase in opioid overdose hospitalizations.”
The B.C. government rolled back decriminalization in April 2024 in response to widespread concerns over public drug use. This February, the province also officially acknowledged that diversion of safer supply drugs does occur.
The study did not conclusively determine whether the increase in hospital visits was due to diverted safer supply opioids, the toxic illicit supply, or other factors.
“There was insufficient evidence to conclusively attribute an increase in opioid overdose deaths to these policy changes,” the study says.
Nguyen’s team had published an earlier, 2024 study in JAMA Internal Medicine that also linked safer supply to increased hospitalizations. However, it failed to control for key confounders such as employment rates and naloxone access. Their 2025 study better accounts for these variables using the synthetic comparison group method.
The study’s authors did not respond to Canadian Affairs’ requests for comment.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Correlation vs. causation
Chris Perlman, a health data and addiction expert at the University of Waterloo, says more studies are needed.
He believes the findings are weak, as they show correlation but not causation.
“The study provides a small signal that the rates of hospitalization have changed, but I wouldn’t conclude that it can be solely attributed to the safer supply and decrim[inalization] policy decisions,” said Perlman.
He also noted the rise in hospitalizations doesn’t necessarily mean more overdoses. Rather, more people may be reaching hospitals in time for treatment.
“Given that the [overdose] rate may have gone down, I wonder if we’re simply seeing an effect where more persons survive an overdose and actually receive treatment in hospital where they would have died in the pre-policy time period,” he said.
The Nguyen study acknowledges this possibility.
“The observed increase in opioid hospitalizations, without a corresponding increase in opioid deaths, may reflect greater willingness to seek medical assistance because decriminalization could reduce the stigma associated with drug use,” it says.
“However, it is also possible that reduced stigma and removal of criminal penalties facilitated the diversion of safer opioids, contributing to increased hospitalizations.”
Karen Urbanoski, an associate professor in the Public Health and Social Policy department at the University of Victoria, is more critical.
“The [study’s] findings do not warrant the conclusion that these policies are causally associated with increased hospitalization or overdose,” said Urbanoski, who also holds the Canada Research Chair in Substance Use, Addictions and Health Services.
Her team published a study in November 2023 that measured safer supply’s impact on mortality and acute care visits. It found safer supply opioids did reduce overdose deaths.
Critics, however, raised concerns that her study misrepresented its underlying data and showed no statistically significant reduction in deaths after accounting for confounding factors.
The Nguyen study differs from Urbanoski’s. While Urbanoski’s team focused on individual-level outcomes, the Nguyen study analyzed broader, population-level effects, including diversion.
Wallace, the biostatistician, agrees more individual-level data could strengthen analysis, but does not believe it undermines the study’s conclusions. Wallace thinks the researchers did their best with the available data they had.
“We do not have a ‘copy’ of B.C. where the policies weren’t implemented to compare with,” said Wallace.
B.C.’s overdose rate of 775 per 100,000 is well above the national average of 533.
Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, has been a vocal critic of B.C.’s decriminalization and safer supply policies.
“If the government doesn’t want to believe this study, well then I invite them to do a similar study,” she told reporters on March 27.
“Show us the evidence that they have failed to show us since 2020,” she added, referring to the year B.C. implemented safer supply.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Our content is always free – but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
Health
Horrific and Deadly Effects of Antidepressants

 The Vigilant Fox
The Vigilant Fox
Once you see what else these drugs are doing, you’ll never look at depression “treatment” the same way again.
The following information is based on a report originally published by A Midwestern Doctor. Key details have been streamlined and editorialized for clarity and impact. Read the original report here.
Did you know that SSRI antidepressants INCREASE suicidal thoughts by 255%?
A clinical trial on healthy volunteers found that 2 out of 20 became suicidal after taking Zoloft.
One was literally on her way to kill herself when a timely phone call saved her life.
But it’s not just suicidal thoughts that make antidepressants dangerous.
And once you see what else these drugs are doing, you’ll never look at depression “treatment” the same way again.
Selective serotonin reuptake inhibitors—or SSRIs—are one of the most harmful medicines prescribed today.
And that’s saying a lot because the market is FULL of harmful medicines.
What’s so bad about these antidepressants?
First of all, their use is widespread and frequently unjustifiable.
They promise to be a magical solution to depression and anxiety, but it’s quite the opposite.
In fact, they can cause side effects far worse than what they claim to treat.
SSRIs don’t just dull your emotions, and they don’t alter your brain chemistry for the better.
They literally reprogram your brain.
Between 40% and 60% of users report emotional numbness. Not just negative emotions—all emotions.
Joy, pain, motivation—all of it completely flatlined.
Some describe it as “life without color” or a “zombie-like” existence.
Sure, maybe you don’t feel depressed anymore. But you don’t feel anything at all.
That sounds… terrible.
Depression can be serious, but should we accept emotionless zombies as the alternative?
If you want to dig even deeper into the dark side of antidepressants and why they’re so harmful, check out @Midwesterndoc’s comprehensive report on the subject. And be sure to share this with anyone you know who may be considering starting an SSRI.
And it’s not just becoming an emotionless zombie you have to worry about. The emotional shutdown can lead to something that is much worse than depression and anxiety.
I don’t mean just a little anger here and there.
SSRIs are causing people to commit suicide—and yes, even horrific mass shootings.
And guess what? The FDA knew about it.
Prozac triggers hallucinations, mania, and violence, and the FDA has known all along.
Even animals become aggressive on SSRIs.
But instead of going back to the drawing board, the FDA approved it anyway.
After nine years on the market, 39,000 people reported major psychiatric events. And those are only the people who reported it…
Really makes you question FDA approval, doesn’t it?
Did you know most of the mass shooters we hear about in the news were often on SSRIs?
It’s true.
And the media even reported on it. But then, they stopped.
That’s weird.
So why are we “not allowed” to talk about SSRIs and violence anymore?
It’s pretty simple.
It would blow the lid off one of the most dangerous pharmaceutical cover-ups in modern history.
It would expose the truth that Big Pharma knowingly released drugs that could make people snap and kill other people.
And they just kept selling them anyway.

But the psychotic violence caused by SSRIs is only the tip of the iceberg.
Obviously, not everyone taking these drugs becomes a mass shooter. But that doesn’t mean the other side effects are any less terrible for those who experience them.
SSRIs truly warp your mind, body, and emotions. And sometimes it is irreversible.
The numbers are truly chilling:
→ A 255% increase in suicidal thoughts
→ 30% of SSRI users develop Bipolar disorder
→ 59% suffer long-term sexual dysfunction
With many saying their libido never came back even after stopping the drug.
The science is clear. The harm caused by SSRIs greatly outweighs any benefits they provide.
Talk about depressing…
A 2020 study involving 20 healthy volunteers with zero history of depression or other mental illnesses had shocking results.
They were each given Zoloft.
TWO of them BECAME suicidal.
One of them was even on her way to kill herself when a divinely timed phone call interrupted her plans.
These two study participants were still affected several months later. They were actually questioning the stability of their personalities.
This doesn’t sound like a magic solution. This sounds like torture.
Speaking of stopping SSRIs—good luck!
They are highly addictive.
And it’s not just physical addiction. It’s neurological.
And because of what they do to the brain, it can take years to step down the dose and wean off of them. Years!
Withdrawal symptoms include things like:
– Brain zaps
– Panic attacks
– Suicidal spirals
– Derealization
And these symptoms can last weeks, months, or even years.
It’s not uncommon to fail and continue taking them because the withdrawal is just that bad.
A 2022 review found that 56% of users who tried to stop SSRIs experience withdrawal symptoms, and 46% describe it as severe.
Psychiatrists mislabel it as a “relapse” and prescribe even more drugs.
The system is set up to trap you. There’s no exit.
And the most vulnerable groups?
Pregnant women and children.
Despite strong evidence linking SSRIs to birth defects, premature birth, and newborn death, the FDA still endorses their use during pregnancy.
One study showed a six times higher risk of pulmonary hypertension in newborns.
Another study showed that SSRI babies lost height and weight in just 19 weeks.
This isn’t good.
SSRIs are being pushed on everyone. Especially vulnerable people like foster kids, parolees, prisoners, and elderly nursing home residents.
And in many of these cases, there is no real ability for them to say no.
That’s not mental health care. That’s drugging people.
The industry tells us SSRIs are “fixing a serotonin imbalance.”
But that’s a lie.
There’s no solid evidence that depression is caused by low serotonin.
So what’s the real mechanism at play here?
SSRIs alter brain wiring. And obviously not always in good ways.
SSRI users describe feeling like their “personality changed” after starting the drug.
The reports are endless and absolutely chilling.
Some were left numb for years. Others became aggressive, impulsive, or dissociated from reality.
Many say they don’t recognize who they became after taking SSRIs.
Excuse me… what?!
And of course, patients and their families are rarely warned about these effects.
Most say they were never told about the risks. There was no informed consent.
How can you not inform depressed people that their medication might make them suicidal? How is it even possible that we can be asking that question?
They experienced these things and talked to their doctors.
They were gaslit every step of the way.
If you or someone you love is taking SSRIs or is considering taking them, I urge you to read the full report from A Midwestern Doctor
How many more people have to suffer before this ends?
How many more people who reach out to their doctor because something is off and they’re looking for help are going to be hurt, sometimes permanently?
It’s time to expose the cover-up and end Big Pharma’s abuse and gaslighting once and for all.
RFK Jr. is right—this could finally be the turning point.
For 40 years, this tragedy was hidden behind slick ads and corrupted science.
But now it’s in the light and MAHA is ready to fight.
If you know anyone considering starting an SSRI, be sure to forward them this information. Because if you wait until after, it might be too late.
Thanks for reading!
This information was based on a report originally published by A Midwestern Doctor. Key details were streamlined and editorialized for clarity and impact.
-

 Business2 days ago
Business2 days agoChinese firm unveils palm-based biometric ID payments, sparking fresh privacy concerns
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoConservatives promise to ban firing of Canadian federal workers based on COVID jab status
-

 Business1 day ago
Business1 day agoIs Government Inflation Reporting Accurate?
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoCarney’s Hidden Climate Finance Agenda
-

 Environment2 days ago
Environment2 days agoExperiments to dim sunlight will soon be approved by UK government: report
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoWhen it comes to pipelines, Carney’s words flow both ways
-
 2025 Federal Election1 day ago
2025 Federal Election1 day agoStudy links B.C.’s drug policies to more overdoses, but researchers urge caution
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoFormer WEF insider accuses Mark Carney of using fear tactics to usher globalism into Canada