Alberta
Pharmacist-led clinics improve access to health care: Lessons from Alberta

News release from the Montreal Economic Institute
In Canada, 35 per cent of avoidable emergency room visits could be handled by pharmacists.
Emulating Alberta’s pharmacist-led clinic model could enhance access to primary care and help avoid unnecessary emergency room visits, according to a new study from the Montreal Economic Institute.
“Pharmacists know medication better than anyone else in our health systems,” explains Krystle Wittevrongel, senior public policy analyst and Alberta project lead at the MEI. “By unlocking their full potential in prescribing and substituting medications, Alberta’s pharmacist-led clinics have helped avoid tens of thousands of unnecessary emergency room visits.”
Pharmacists in Alberta have the largest prescribing authority in the country, including the ability to prescribe schedule one drugs with special training.
Unlike in Ontario and Manitoba, Alberta pharmacists are authorized to substitute prescribed medications, which can help address issues such as adverse reactions caused by interaction with other treatments.
The study explains that this can help reduce pressure on hospitals, as prescription-related issues account for more than 10 per cent of emergency room visits.
Alberta’s first pharmacist-led clinic, in Lethbridge, sees between 14,600 and 21,900 patients per year since opening in 2022.
It is expected that there will be 103 such clinics active in the province by the end of 2024.
The researcher also links the success of the pharmacist-led clinic model in Alberta to pharmacists’ expanded scope of practice in the province.
Among other things, Alberta pharmacists are able to order and interpret lab tests, unlike their counterparts in British Columbia, Ontario, and Newfoundland and Labrador.
A 2019 peer-reviewed study found that pharmacists could handle 35 per cent of avoidable emergency room visits in Canada.
“By enabling pharmacists to play a larger role in its health system, Alberta is redirecting minor cases from emergency rooms to more appropriate facilities,” said Wittevrongel. “Just imagine how much faster things could be if pharmacists could take care of 35 per cent of the unnecessary load placed on Canada’s emergency rooms.”
The MEI study is available here.
* * *
The MEI is an independent public policy think tank with offices in Montreal and Calgary. Through its publications, media appearances, and advisory services to policy-makers, the MEI stimulates public policy debate and reforms based on sound economics and entrepreneurship.
Alberta
Low oil prices could have big consequences for Alberta’s finances

From the Fraser Institute
By Tegan Hill
Amid the tariff war, the price of West Texas Intermediate oil—a common benchmark—recently dropped below US$60 per barrel. Given every $1 drop in oil prices is an estimated $750 million hit to provincial revenues, if oil prices remain low for long, there could be big implications for Alberta’s budget.
The Smith government already projects a $5.2 billion budget deficit in 2025/26 with continued deficits over the following two years. This year’s deficit is based on oil prices averaging US$68.00 per barrel. While the budget does include a $4 billion “contingency” for unforeseen events, given the economic and fiscal impact of Trump’s tariffs, it could quickly be eaten up.
Budget deficits come with costs for Albertans, who will already pay a projected $600 each in provincial government debt interest in 2025/26. That’s money that could have gone towards health care and education, or even tax relief.
Unfortunately, this is all part of the resource revenue rollercoaster that’s are all too familiar to Albertans.
Resource revenue (including oil and gas royalties) is inherently volatile. In the last 10 years alone, it has been as high as $25.2 billion in 2022/23 and as low as $2.8 billion in 2015/16. The provincial government typically enjoys budget surpluses—and increases government spending—when oil prices and resource revenue is relatively high, but is thrown into deficits when resource revenues inevitably fall.
Fortunately, the Smith government can mitigate this volatility.
The key is limiting the level of resource revenue included in the budget to a set stable amount. Any resource revenue above that stable amount is automatically saved in a rainy-day fund to be withdrawn to maintain that stable amount in the budget during years of relatively low resource revenue. The logic is simple: save during the good times so you can weather the storm during bad times.
Indeed, if the Smith government had created a rainy-day account in 2023, for example, it could have already built up a sizeable fund to help stabilize the budget when resource revenue declines. While the Smith government has deposited some money in the Heritage Fund in recent years, it has not created a dedicated rainy-day account or introduced a similar mechanism to help stabilize provincial finances.
Limiting the amount of resource revenue in the budget, particularly during times of relatively high resource revenue, also tempers demand for higher spending, which is only fiscally sustainable with permanently high resource revenues. In other words, if the government creates a rainy-day account, spending would become more closely align with stable ongoing levels of revenue.
And it’s not too late. To end the boom-bust cycle and finally help stabilize provincial finances, the Smith government should create a rainy-day account.
Alberta
Governments in Alberta should spur homebuilding amid population explosion

From the Fraser Institute
By Tegan Hill and Austin Thompson
In 2024, construction started on 47,827 housing units—the most since 48,336 units in 2007 when population growth was less than half of what it was in 2024.
Alberta has long been viewed as an oasis in Canada’s overheated housing market—a refuge for Canadians priced out of high-cost centres such as Vancouver and Toronto. But the oasis is starting to dry up. House prices and rents in the province have spiked by about one-third since the start of the pandemic. According to a recent Maru poll, more than 70 per cent of Calgarians and Edmontonians doubt they will ever be able to afford a home in their city. Which raises the question: how much longer can this go on?
Alberta’s housing affordability problem reflects a simple reality—not enough homes have been built to accommodate the province’s growing population. The result? More Albertans competing for the same homes and rental units, pushing prices higher.
Population growth has always been volatile in Alberta, but the recent surge, fuelled by record levels of immigration, is unprecedented. Alberta has set new population growth records every year since 2022, culminating in the largest-ever increase of 186,704 new residents in 2024—nearly 70 per cent more than the largest pre-pandemic increase in 2013.
Homebuilding has increased, but not enough to keep pace with the rise in population. In 2024, construction started on 47,827 housing units—the most since 48,336 units in 2007 when population growth was less than half of what it was in 2024.
Moreover, from 1972 to 2019, Alberta added 2.1 new residents (on average) for every housing unit started compared to 3.9 new residents for every housing unit started in 2024. Put differently, today nearly twice as many new residents are potentially competing for each new home compared to historical norms.
While Alberta attracts more Canadians from other provinces than any other province, federal immigration and residency policies drive Alberta’s population growth. So while the provincial government has little control over its population growth, provincial and municipal governments can affect the pace of homebuilding.
For example, recent provincial amendments to the city charters in Calgary and Edmonton have helped standardize building codes, which should minimize cost and complexity for builders who operate across different jurisdictions. Municipal zoning reforms in Calgary, Edmonton and Red Deer have made it easier to build higher-density housing, and Lethbridge and Medicine Hat may soon follow suit. These changes should make it easier and faster to build homes, helping Alberta maintain some of the least restrictive building rules and quickest approval timelines in Canada.
There is, however, room for improvement. Policymakers at both the provincial and municipal level should streamline rules for building, reduce regulatory uncertainty and development costs, and shorten timelines for permit approvals. Calgary, for instance, imposes fees on developers to fund a wide array of public infrastructure—including roads, sewers, libraries, even buses—while Edmonton currently only imposes fees to fund the construction of new firehalls.
It’s difficult to say how long Alberta’s housing affordability woes will endure, but the situation is unlikely to improve unless homebuilding increases, spurred by government policies that facilitate more development.
-

 2025 Federal Election7 hours ago
2025 Federal Election7 hours agoThe Federal Brief That Should Sink Carney
-
 2025 Federal Election9 hours ago
2025 Federal Election9 hours agoHow Canada’s Mainstream Media Lost the Public Trust
-

 2025 Federal Election12 hours ago
2025 Federal Election12 hours agoOttawa Confirms China interfering with 2025 federal election: Beijing Seeks to Block Joe Tay’s Election
-
 John Stossel8 hours ago
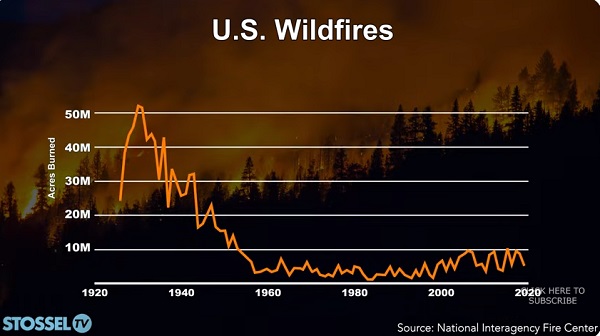
John Stossel8 hours agoClimate Change Myths Part 2: Wildfires, Drought, Rising Sea Level, and Coral Reefs
-
 2025 Federal Election11 hours ago
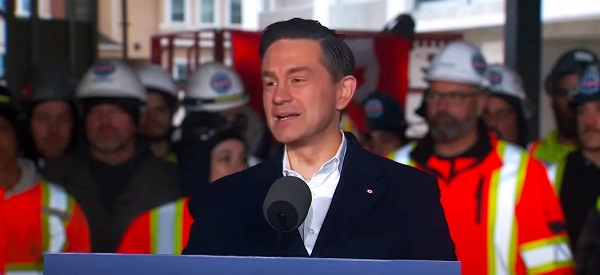
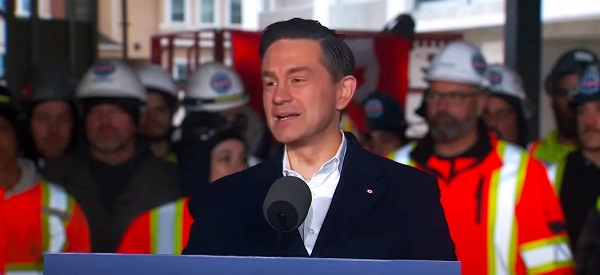
2025 Federal Election11 hours agoReal Homes vs. Modular Shoeboxes: The Housing Battle Between Poilievre and Carney
-

 COVID-1910 hours ago
COVID-1910 hours agoNearly Half of “COVID-19 Deaths” Were Not Due to COVID-19 – Scientific Reports Journal
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPoilievre’s Conservatives promise to repeal policy allowing male criminals in female jails
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCarney Liberals pledge to follow ‘gender-based goals analysis’ in all government policy



