Health
Patient Success Story From The Brent Sutter Sports Medicine Clinic – Part 2 Of 2
By Sheldon Spackman
Since it’s inception in early 2016, the Brent Sutter Sports Medicine Clinic has served over 800 patients. A growing number are self-referring through the clinic’s website, but for now most patients are referred to the clinic as Carly Kukowski was.
Three years ago, Carly Kukowski from Eckville injured her right knee playing baseball. A few weeks later she went dirt-biking and aggravated the injury. It was time to see her family doctor. After waiting almost 9 months for an MRI it was discovered she severed her ACL and had a torn meniscus. Kukowski waited about 1 year to see a surgeon. In the meantime, she got around on her injured knee, making her injuries even worse. It got to the point that she wasn’t able to do the activities she wanted to do. Snowmobiling, dirt-biking and baseball were out of the question. Eventually her knee was fixed but the entire process took well over a year.
Then last November, Kukowski injured her other knee. This time she came to the Brent Sutter Sports Medicine Clinic. Dr. Wolstenholme diagnosed a torn ACL and a quick route to recovery was set out. Carly was able to get into surgery in just a few weeks and her recovery is nearly complete.
Health
RFK Jr’s argument for studying efficacy of various vaccines

From HHS Secretary Robert F Kennedy’s Facebook Page
Addictions
The War on Commonsense Nicotine Regulation

From the Brownstone Institute
Cigarettes kill nearly half a million Americans each year. Everyone knows it, including the Food and Drug Administration. Yet while the most lethal nicotine product remains on sale in every gas station, the FDA continues to block or delay far safer alternatives.
Nicotine pouches—small, smokeless packets tucked under the lip—deliver nicotine without burning tobacco. They eliminate the tar, carbon monoxide, and carcinogens that make cigarettes so deadly. The logic of harm reduction couldn’t be clearer: if smokers can get nicotine without smoke, millions of lives could be saved.
Sweden has already proven the point. Through widespread use of snus and nicotine pouches, the country has cut daily smoking to about 5 percent, the lowest rate in Europe. Lung-cancer deaths are less than half the continental average. This “Swedish Experience” shows that when adults are given safer options, they switch voluntarily—no prohibition required.
In the United States, however, the FDA’s tobacco division has turned this logic on its head. Since Congress gave it sweeping authority in 2009, the agency has demanded that every new product undergo a Premarket Tobacco Product Application, or PMTA, proving it is “appropriate for the protection of public health.” That sounds reasonable until you see how the process works.
Manufacturers must spend millions on speculative modeling about how their products might affect every segment of society—smokers, nonsmokers, youth, and future generations—before they can even reach the market. Unsurprisingly, almost all PMTAs have been denied or shelved. Reduced-risk products sit in limbo while Marlboros and Newports remain untouched.
Only this January did the agency relent slightly, authorizing 20 ZYN nicotine-pouch products made by Swedish Match, now owned by Philip Morris. The FDA admitted the obvious: “The data show that these specific products are appropriate for the protection of public health.” The toxic-chemical levels were far lower than in cigarettes, and adult smokers were more likely to switch than teens were to start.
The decision should have been a turning point. Instead, it exposed the double standard. Other pouch makers—especially smaller firms from Sweden and the US, such as NOAT—remain locked out of the legal market even when their products meet the same technical standards.
The FDA’s inaction has created a black market dominated by unregulated imports, many from China. According to my own research, roughly 85 percent of pouches now sold in convenience stores are technically illegal.
The agency claims that this heavy-handed approach protects kids. But youth pouch use in the US remains very low—about 1.5 percent of high-school students according to the latest National Youth Tobacco Survey—while nearly 30 million American adults still smoke. Denying safer products to millions of addicted adults because a tiny fraction of teens might experiment is the opposite of public-health logic.
There’s a better path. The FDA should base its decisions on science, not fear. If a product dramatically reduces exposure to harmful chemicals, meets strict packaging and marketing standards, and enforces Tobacco 21 age verification, it should be allowed on the market. Population-level effects can be monitored afterward through real-world data on switching and youth use. That’s how drug and vaccine regulation already works.
Sweden’s evidence shows the results of a pragmatic approach: a near-smoke-free society achieved through consumer choice, not coercion. The FDA’s own approval of ZYN proves that such products can meet its legal standard for protecting public health. The next step is consistency—apply the same rules to everyone.
Combustion, not nicotine, is the killer. Until the FDA acts on that simple truth, it will keep protecting the cigarette industry it was supposed to regulate.
-

 Business2 days ago
Business2 days agoTrans Mountain executive says it’s time to fix the system, expand access, and think like a nation builder
-
 International2 days ago
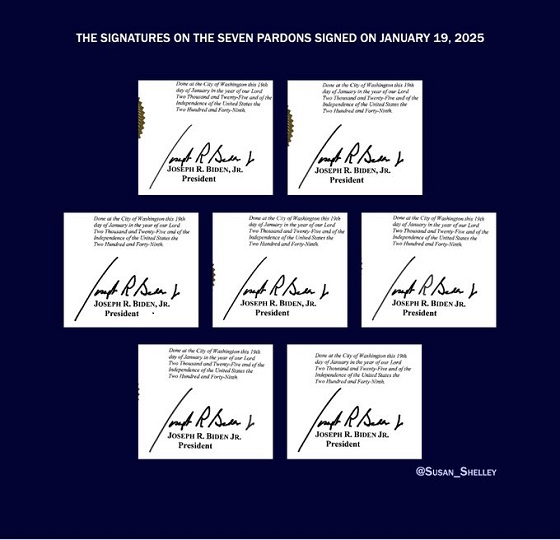
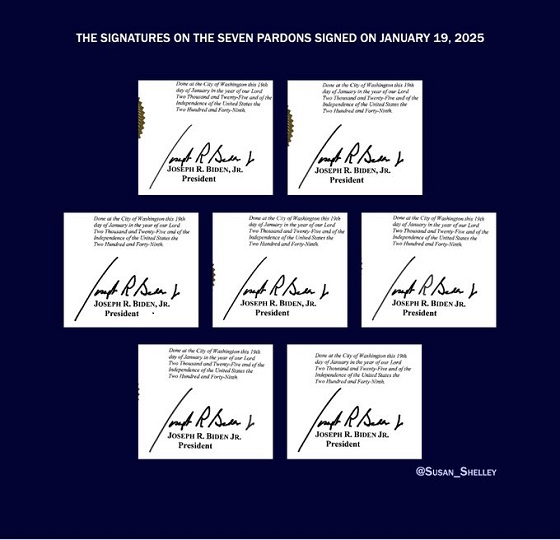
International2 days agoBiden’s Autopen Orders declared “null and void”
-

 MAiD1 day ago
MAiD1 day agoStudy promotes liver transplants from Canadian euthanasia victims
-

 Business1 day ago
Business1 day agoCanada has given $109 million to Communist China for ‘sustainable development’ since 2015
-

 Internet2 days ago
Internet2 days agoMusk launches Grokipedia to break Wikipedia’s information monopoly
-

 Business2 days ago
Business2 days agoCanada’s combative trade tactics are backfiring
-

 Business1 day ago
Business1 day agoYou Won’t Believe What Canada’s Embassy in Brazil Has Been Up To
-

 Automotive1 day ago
Automotive1 day agoCarney’s Budget Risks Another Costly EV Bet