MAiD
MAiD advocate speaks out against expansion of euthanasia to the mentally ill
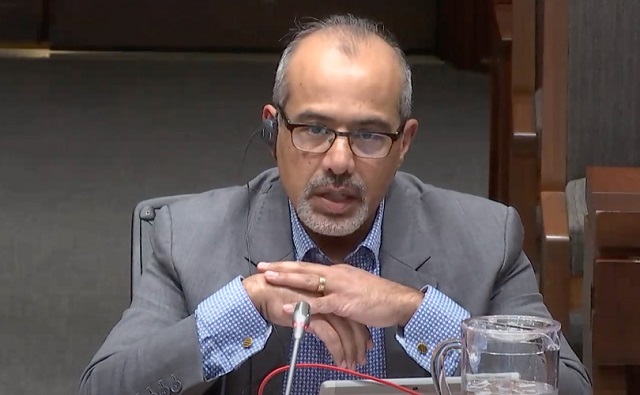
Professor Sonu Gaind
From LifeSiteNews
By and
‘not so much a slippery slope as a runaway train.’
A leading Canadian psychiatrist has testified that Canada is “not ready” to offer euthanasia to the mentally ill.
Doctor K. Sonu Gaind, who supports euthanasia under certain circumstances, testified on November 28 before the Special Joint Committee on Medical Assistance in Dying (MAiD) in Ottawa against expanding the practice.
“This expansion is not so much a slippery slope as a runaway train,” he declared.
Gaind underscored that he is not a “conscientious objector” to euthanasia and that he was the chair of his prior hospital’s MAiD team. His principal concern is to protect those with mental illness.
“MAiD is for irremediable medical conditions, ones that we can predict won’t improve,” he said.
“Worldwide evidence shows we cannot predict irremediability in cases of mental illness, meaning the primary safeguard underpinning MAiD is already bypassed,” he continued.
The leading psychiatrist added, “Scientific evidence shows we cannot distinguish suicidality caused by mental illness from motivations leading to psychiatric MAiD requests … .[There are] overlapping characteristics suggesting there may be no distinction to make.”
RELATED: Top Canadian psychiatrists urge gov’t to halt expansion of euthanasia to the mentally ill
Gaind directly addressed the claims of “discrimination” made by those in support of the expansion of MAiD, including Senator Stanley Kutcher and Dr. Mona Gupta.
“MAiD assessors will be wrong over half the time when predicting irremediability, will wrongly believe they are filtering out suicidality, and will instead provide death to marginalized suicidal Canadians who could have improved,” he said.
“That is the ultimate discrimination.”
Gaind also took issue with statements made by Dr. Jocelyn Downie, a leading euthanasia activist and Trudeau Foundation Fellow.
“Professor Downie claimed, ‘Irremediability is a legal term rather than a clinical concept.’ Try those mental gymnastics on your constituents,” Gaind said dryly.
“Convince them it was okay their loved ones with mental illness got MAiD, not because of a clinical assessment based in medicine or science, but on the ethics of the particular assessor.”
Gaind criticized the euthanasia curriculum used by the Canadian Association of MAiD Assessors and Providers (CAMAP) for not teaching users how to differentiate between “suicidality” and “psychiatric MAiD requests.”
“A key problem with psychiatric MAiD assessments [is] the hubris of the assessor thinking they can determine irremediability and distinguish suicidality from psychiatric MAiD requests, when evidence shows they can do neither,” he said.
Based on all the evidence, Gaind is convinced that direct euthanasia should not be offered to the mentally ill.
“I’ve reviewed our legislation, the Health Canada practice standard, and the CAMAP training for MAiD for mental illness,” he said. “As someone who supports MAiD in general, I assure you: we are not ready.”
Gaind included in his fast-paced, passionate speech an admonishment of those who support expansion of MAiD.
“An echo chamber has driven expansion with reassurances but no safeguards,” he asserted. “It’s reassurance theatre.”
Gaind is a University of Toronto governor and professor of psychiatric medicine. In addition, he is Chief of the Department of Psychiatry at Toronto’s Sunnybrook Health Sciences Centre and past president of Canadian Psychiatric Association.
Former Bill C-7, which allows for euthanasia on the grounds of mental illness, was passed into law in early 2021. However, the eligibility of the mentally ill to be killed was delayed for two years. The exclusion was extended in February 2023 and then extended again in March to last until March 17, 2024.
In October this year, Conservative MP Ed Fast introduced Bill C-314, an effort to “amend the Criminal Code to provide that a mental disorder is not a grievous and irremediable medical condition for which a person could receive medical assistance in dying.”
When put to a vote, the Bill was defeated 167 to 150.
MAiD
Disability rights panel calls out Canada, US states pushing euthanasia on sick patients

From LifeSiteNews
Physician-assisted suicide programs in the US and Canada are discriminating against patients with serious medical conditions according to a panel discussion at the Religion News Association.
Physician-assisted suicide programs in the United States and Canada are discriminating against patients with serious medical conditions even when their cases are not terminal, in many cases pushing to end their lives for financial reasons rather than medical.
Catholic News Agency reported that a panel of disability-rights advocates recently examined the landscape of the issue during the Religion News Association’s 2025 annual conference. During the panel, Patients Rights Action Fund (PRAF) executive director Matt Vallière accused state euthanasia programs of discriminating against patients with life-threatening conditions in violation of the Americans with Disabilities Act, noting that when a state will “will pay for every instance of assisted suicide” but not palliative care, “I don’t call that autonomy, I call that eugenics.”
Inclusion Canada CEO Krista Carr, meanwhile, discussed her organization’s lawsuit against the expansion of Canada’s medical assistance in dying (MAID) program to “people with an incurable disease or disability who are not dying, so they’re not at end of life and their death is not reasonably foreseeable.”
More astonishingly, she added, this “funded right” to lethal injection is slated to be expanded to mental illness in 2027.
“By setting out a timeline of three years, it’s an indication that the systems need to move towards readiness in two years. There’s the opportunity to do another review, and to assess the readiness of the system through a parliamentary process,” Health Minister Mark Holland said in February of the move, which Dying with Dignity Canada presents as a matter of “equality” for “those whose sole underlying condition is a mental illness.”
“It’s being called a choice,” but “it’s not a choice,” Carr said. Rather, these programs are pushing the “choice” on patients in “a desperate situation where they can’t get the support they need.”
As LifeSiteNews recently covered, the “most recent reports show that (medical assistance in dying) is the sixth highest cause of death in Canada. However, it was not listed as such in Statistics Canada’s top 10 leading causes of death from 2019 to 2022.”
In America, nine states plus the District of Columbia currently allow assisted suicide.
Support is available to talk those struggling with suicidal thoughts out of ending their lives. The American Suicide & Crisis Lifeline and the Canadian Suicide Crisis Helpline can both be reached by calling or texting 988.
MacDonald Laurier Institute
Rushing to death in Canada’s MAiD regime

 By Ramona Coelho for Inside Policy
By Ramona Coelho for Inside Policy
Canada legalized Medical Assistance in Dying (MAiD) in 2016, encompassing both euthanasia and assisted suicide. Initially limited to those nearing their natural death, eligibility expanded in 2021 to individuals with physical disabilities, with eligibility for individuals with mental illness in 2027. Parliamentary recommendations include MAiD for children. A recent federal consultation explored extending MAiD to those who lack capacity via advance directives, an approach Quebec has already adopted, despite its criminal status under federal law.
Despite its compassionate framing, investigative journalists and government reports reveal troubling patterns where inadequate exploration of reversible suffering – such as lack of access to medical treatments, poverty, loneliness, and feelings of being a burden – have driven Canadians to choose death. As described by our former Disability Inclusion Minister, Canada’s system at times makes it easier to access MAiD than to receive basic care like a wheelchair. With over 60,000 MAiD cases by the end of 2023, the evidence raises grave concerns about Canada’s MAiD regime.
I am a member of Ontario’s MAiD Death Review Committee (MDRC). Last year, the Chief Coroner released MDRC reports, and a new set of reports has just been published. The first report released by the Office of the Chief Coroner, Waivers of Final Consent, examines how individuals in Track 1 (reasonably foreseeable natural death) can sign waivers to have their lives ended even if they lose the capacity to consent by the scheduled date of MAiD. The second, Navigating Complex Issues within Same Day and Next Day MAiD Provisions, includes cases where MAiD was provided on the same day or the day after it was requested. These reports raise questions about whether proper assessments, thorough exploration of suffering, and informed consent were consistently practised by MAiD clinicians. While MDRC members hold diverse views, here is my take.
Rushing to death, Ignoring Reversible Causes of Suffering
In the same-day or next-day MAiD report, Mrs. B, in her 80s, after complications from surgery, opted for palliative care, leading to discharge home. She later requested a MAiD assessment, but her assessor noted she preferred palliative care based on personal and religious values. The next day, her spouse, struggling with caregiver burnout, took her to the emergency department, but she was discharged home. When a request for hospice palliative care was denied, her spouse contacted the provincial MAiD coordination service for an urgent assessment. A new assessor deemed her eligible for MAiD, despite concerns from the first practitioner, who questioned the new assessor on the urgency, the sudden shift in patient perspective, and the influence of caregiver burnout. The initial assessor requested an opportunity for re-evaluation, but this was denied, with the second assessor deeming it urgent. That evening, a third MAiD practitioner was brought in, and Mrs. B underwent MAiD that night.
The focus should have been on ensuring adequate palliative care and support for Mrs. B and her spouse. Hospice and palliative care teams should have been urgently re-engaged, given the severity of the situation. Additionally, the MAiD provider expedited the process despite the first assessor’s and Mrs. B’s concerns without fully considering the impact of her spouse’s burnout.
The report also has worrying trends suggesting that local medical cultures—rather than patient choice—could be influencing rushed MAiD. Geographic clustering, particularly in Western Ontario, where same-day and next-day MAiD deaths occur most frequently, raises concerns that some MAiD providers may be predisposed to rapidly approve patients for quick death rather than ensuring patients have access to adequate care or exploring if suffering is remediable. This highlights a worrying trend where the speed of the MAiD provision is prioritized over patient-centered care and ethical safeguards.
MAiD without Free and Informed Choice
Consent has been central to Canadians’ acceptance of the legalization of euthanasia and assisted suicide. However, some cases in these reports point to concerns already raised by clinicians: the lack of thorough capacity assessments and concerns that individuals may not have freely chosen MAiD.
In the waiver of final consent report, Mr. B, a man with Alzheimer’s, had been approved for MAiD with such a waiver. However, by the scheduled provision date, his spouse reported increased confusion. Upon arrival, the MAiD provider noted that Mr. B no longer recognized them and so chose not to engage him in discussion at all. Without any verbal interaction to determine his current wishes or understanding, Mr. B’s life was ended.
In the same-day or next-day MAiD report, Mr. C, diagnosed with metastatic cancer, initially expressed interest in MAiD but then experienced cognitive decline and became delirious. He was sedated for pain management. Despite the treating team confirming that capacity was no longer present, a MAiD practitioner arrived and withheld sedation, attempting to rouse him. It was documented that the patient mouthed “yes” and nodded and blinked in response to questions. Based on this interaction, the MAiD provider deemed the patient to have capacity. The MAiD practitioner then facilitated a virtual second assessment, and MAiD was administered.
These individuals were not given genuine opportunities to confirm whether they wished to die. Instead, their past wishes or inquiries were prioritized, raising concerns about ensuring free and informed consent for MAiD. As early as 2020, the Chief Coroner of Ontario identified cases where patients received MAiD without well-documented capacity assessments, even though their medical records suggested they lacked capacity. Further, when Dr. Leonie Herx, past president of the Canadian Society of Palliative Medicine, testified before Parliament about MAiD frequently occurring without capacity, an MP dismissed her, advising Parliament to be cautious about considering seriously evidence under parliamentary immunities that amounted to malpractice allegations, which should be handled by the appropriate regulatory bodies or police. These dismissive comments stand in stark contrast with the gravity of assessing financial capacity, and yet the magnitude is greater when ending life. By way of comparison, for my father, an Ontario-approved capacity expert conducted a rigorous evaluation before declaring him incapable of managing his finances. This included a lengthy interview, collateral history, and review of financial documents—yet no such rigorous capacity assessment is mandated for MAiD.
What is Compassion?
While the federal government has finished its consultation on advance directives for MAiD, experts warn against overlooking the complexities of choosing death based on hypothetical suffering and no lived experience to inform those choices. A substitute decision-maker has to interpret prior wishes, leading to guesswork and ethical dilemmas. These cases highlight how vulnerable individuals, having lost the capacity to consent, may be coerced or unduly influenced to die—whether through financial abuse, caregiver burnout, or other pressures—reminding us that the stakes are high – life and death, no less.
The fundamental expectation of health care should be to rush to care for the patient, providing support through a system that embraces them—not rush them toward death without efforts to mitigate suffering or ensure free and informed consent. If we truly value dignity, we must invest in comprehensive care to prevent patients from being administered speedy death in their most vulnerable moment, turning their worst day into potentially their last.
Dr. Ramona Coelho is a family physician whose practice largely serves marginalised persons in London, Ontario. She is a senior fellow at the Macdonald-Laurier Institute and co-editor of the new book “Unravelling MAiD in Canada” from McGill University Press.
-

 Also Interesting2 days ago
Also Interesting2 days agoMortgage Mayhem: How Rising Interest Rates Are Squeezing Alberta Homeowners
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoConservative Party urges investigation into Carney plan to spend $1 billion on heat pumps
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoCommunist China helped boost Mark Carney’s image on social media, election watchdog reports
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoFifty Shades of Mark Carney
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoCorporate Media Isn’t Reporting on Foreign Interference—It’s Covering for It
-

 Business1 day ago
Business1 day agoStocks soar after Trump suspends tariffs
-

 Justice2 days ago
Justice2 days agoCanadian government sued for forcing women to share spaces with ‘transgender’ male prisoners
-

 Alberta2 days ago
Alberta2 days agoAlberta takes big step towards shorter wait times and higher quality health care




