Addictions
Leading addiction doctor warns of Canada’s ‘safer supply’ disaster

A man considers using a prescription opioid. Credit: Dreamstime
By Liam Hunt
Addiction physician Dr. Sharon Koivu has seen the effects of safer supply programs in her clinical practice and personal life — and is sounding the alarm
Dr. Sharon Koivu, an addiction physician and parent, believes her son might not have survived to adulthood if Canada’s “safer supply” programs had been in effect during his adolescence.
Having worked on the front lines of Ontario’s opioid crisis, she views these programs as a catastrophic failure.
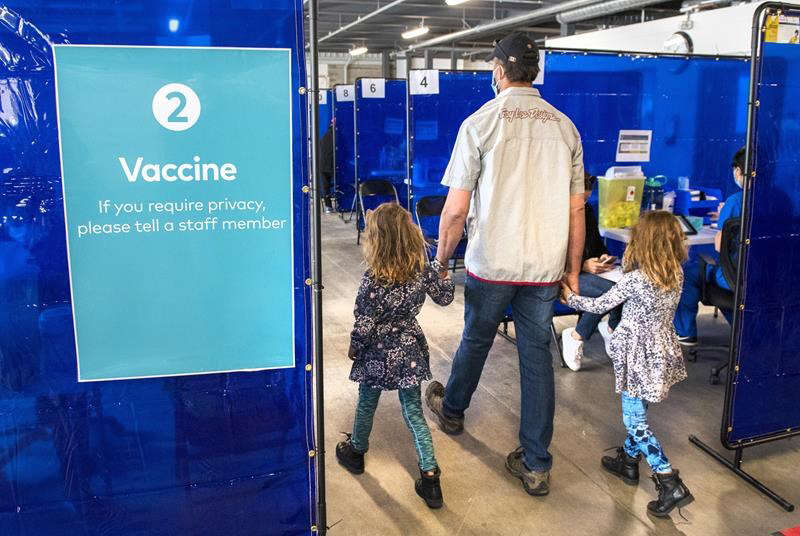
In an extended interview, Koivu explained the unintended consequences of these programs, which offer free tablets of hydromorphone — an opioid about as strong as heroin – to vulnerable patients with a history of addiction. While advocates of safer supply claim it mitigates the use of more dangerous illicit substances, there is evidence that most users divert — that is, sell or trade — their hydromorphone to acquire stronger substances.
Safer supply was first piloted in London, Ont., in 2016, before being widely expanded across Canada in 2020 with the help of generous federal grants. While the program looked good on paper, Koivu, who provides comprehensive addiction consultation services at a London-based hospital, saw a different reality: her patients were destabilizing, relapsing and fatally overdosing because of safer supply.
Koivu says that “one hundred percent” of her colleagues working in addiction medicine have noticed safer supply diversion. Some patients have told her they have been threatened with violence if they do not procure and divert these drugs. She estimates that, because of safer supply, tens of thousands of diverted hydromorphone pills — also known as “Dilaudid,” “dillies” or “D8s” — are flooding into Canadian streets every day.
For context, just two or three of these pills, if snorted, are enough to induce an overdose in a new user.
This influx has caused the drug’s street price to crash by as much as 95 per cent. While 8-milligram hydromorphone pills used to sell for $20 each several years ago, they can now be bought for as little as a dollar or two. These rock-bottom prices have ignited a new wave of addictions and relapses, and lured opioid-naive individuals into experimenting with what is essentially pharmaceutical heroin.
Koivu estimates that 80 per cent of her opioid-using patients now take diverted hydromorphone.
“The biggest harm is that we’ve turned on the tap and we’ve made everything cheap, which is leading to a large increase in the number of people becoming addicted and suffering,” she said.
“It is the most serious issue that I’ve seen in my lifetime.”
Safer supply programs seem to regularly overprescribe opioids without considering patients’ actual needs, Koivu says. Patients have come into her hospital with prescriptions that provide 40 eight-milligram hydromorphone pills a day, even though they can only tolerate 10 pills.
Subscribe to our newsletter to get our latest news and analysis – or donate to our investigative journalism fund.
‘That attraction is horrific’
Throughout the first few decades of Koivu’s career, almost “everyone” in her patient pool developed addictions due to childhood traumas or from mishandling opioids prescribed for chronic pain.
Since the advent of safer supply, the origins of new opioid addictions have shifted toward social or recreational exposure. Concerningly, this exposure often occurs in patients’ adolescent years.
“I’m seeing an increase in youth becoming addicted,” said Koivu, who has had patients as young as 15 tell her their addictions began through diverted hydromorphone.
“Almost everyone I see who’s started since 2018 started recreationally. It started as something that was at a party. It’s now a recreational drug at the youth level.”
Parents often seem completely unaware of the problem. Some have told Koivu they overheard their children discussing the availability of “D8s” at their highschools, only to later realize — when it was too late — they were referring to opioids.
“You can’t walk into your house with a six-pack of beer. If you’re smoking weed, people can smell it. But you can walk into your house with a lot of [tablets] in your pocket. So, it’s cheap, really easy to hide, and is even called ‘safe’ by the government. I think that attraction is horrific.”
“Our youth are dying at a higher rate … and we have a lot more hydromorphone found in [their bodies] at the time of death.”
While safer supply programs claim to make communities safer, Koivu’s lived experiences suggest the opposite. She used to reside in London’s Old East Village, where the city’s first safer supply program opened in 2016, but moved away after watching her neighbourhood deteriorate from widespread crime, overdoses and drug trafficking.
“I moved there to support a supervised injection site,” said Koivu. “Then I watched that community drastically change when safer supply was implemented. … I would go for walks and directly see diversion taking place. Homelessness is very complicated, but this has absolutely fueled it in ways that are unconscionable.”
Koivu characterizes the evidentiary standards used by advocates of safer supply as “deeply problematic.” She says many of the studies supporting safer supply are qualitative — meaning they rely on interviews — and use anecdotal data from patients who have a vested interest in perpetuating the program.
While Koivu has been blowing the whistle on safer supply programs for years, her concerns largely went unnoticed until recently. She has faced years of harassment and denigration for her views.
“When I came to say I’m concerned about what I’m seeing: the infections, the suffering, the encampments … I was literally told that I was lying,” she said.
Last month, the London Police Service provided the National Post with data showing that annual hydromorphone seizures increased by 3,000 per cent after access to safer supply was significantly expanded in 2020. The newspaper has since raised questions about why this data was not released earlier and whether the police stonewalled attempts to investigate the issue.
Koivu considers herself a lifelong progressive and has historically supported the New Democratic Party. But she is concerned many left-leaning politicians have ignored criticism of safer supply. Many seemingly believe that opposition to it is inherently conservative.
“I went to a hearing in Ottawa of a standing committee to talk about addiction,” she said. “We had five minutes to give a talk, and then two hours to answer questions, [but] I didn’t receive any questions from the NDP or the Liberals.”
Although Koivu believes safe supply can play a role in the continuum of care for opioid addiction, she says it must be executed in a meticulous manner that prevents diversion and emphasizes pathways to recovery.
“It needs to be part of a comprehensive strategy to help people get their lives back. And right now, it’s not.”
Above all, it is Koivu’s experience as a mother that drives her to criticize safer supply. One of her sons struggled with opioid addiction as a young adult. Although he eventually recovered, the experience could have killed him.
“Had this program been around … my family could have been another statistic from an opioid death. That drives me. Because it’s very real, and it’s very personal.”
|
|
A guest post by
|
Subscribe to Break The Needle. Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
Addictions
Coffee, Nicotine, and the Politics of Acceptable Addiction

From the Brownstone Institute
By
Every morning, hundreds of millions of people perform a socially approved ritual. They line up for coffee. They joke about not being functional without caffeine. They openly acknowledge dependence and even celebrate it. No one calls this addiction degenerate. It is framed as productivity, taste, wellness—sometimes even virtue.
Now imagine the same professional discreetly using a nicotine pouch before a meeting. The reaction is very different. This is treated as a vice, something vaguely shameful, associated with weakness, poor judgment, or public health risk.
From a scientific perspective, this distinction makes little sense.
Caffeine and nicotine are both mild psychoactive stimulants. Both are plant-derived alkaloids. Both increase alertness and concentration. Both produce dependence. Neither is a carcinogen. Neither causes the diseases historically associated with smoking. Yet one has become the world’s most acceptable addiction, while the other remains morally polluted even in its safest, non-combustible forms.
This divergence has almost nothing to do with biology. It has everything to do with history, class, marketing, and a failure of modern public health to distinguish molecules from mechanisms.
Two Stimulants, One Misunderstanding
Nicotine acts on nicotinic acetylcholine receptors, mimicking a neurotransmitter the brain already uses to regulate attention and learning. At low doses, it improves focus and mood. At higher doses, it causes nausea and dizziness—self-limiting effects that discourage excess. Nicotine is not carcinogenic and does not cause lung disease.
Caffeine works differently, blocking adenosine receptors that signal fatigue. The result is wakefulness and alertness. Like nicotine, caffeine indirectly affects dopamine, which is why people rely on it daily. Like nicotine, it produces tolerance and withdrawal. Headaches, fatigue, and irritability are routine among regular users who skip their morning dose.
Pharmacologically, these substances are peers.
The major difference in health outcomes does not come from the molecules themselves but from how they have been delivered.
Combustion Was the Killer
Smoking kills because burning organic material produces thousands of toxic compounds—tar, carbon monoxide, polycyclic aromatic hydrocarbons, and other carcinogens. Nicotine is present in cigarette smoke, but it is not what causes cancer or emphysema. Combustion is.
When nicotine is delivered without combustion—through patches, gum, snus, pouches, or vaping—the toxic burden drops dramatically. This is one of the most robust findings in modern tobacco research.
And yet nicotine continues to be treated as if it were the source of smoking’s harm.
This confusion has shaped decades of policy.
How Nicotine Lost Its Reputation
For centuries, nicotine was not stigmatized. Indigenous cultures across the Americas used tobacco in religious, medicinal, and diplomatic rituals. In early modern Europe, physicians prescribed it. Pipes, cigars, and snuff were associated with contemplation and leisure.
The collapse came with industrialization.
The cigarette-rolling machine of the late 19th century transformed nicotine into a mass-market product optimized for rapid pulmonary delivery. Addiction intensified, exposure multiplied, and combustion damage accumulated invisibly for decades. When epidemiology finally linked smoking to lung cancer and heart disease in the mid-20th century, the backlash was inevitable.
But the blame was assigned crudely. Nicotine—the named psychoactive component—became the symbol of the harm, even though the damage came from smoke.
Once that association formed, it hardened into dogma.
How Caffeine Escaped
Caffeine followed a very different cultural path. Coffee and tea entered global life through institutions of respectability. Coffeehouses in the Ottoman Empire and Europe became centers of commerce and debate. Tea was woven into domestic ritual, empire, and gentility.
Crucially, caffeine was never bound to a lethal delivery system. No one inhaled burning coffee leaves. There was no delayed epidemic waiting to be discovered.
As industrial capitalism expanded, caffeine became a productivity tool. Coffee breaks were institutionalized. Tea fueled factory schedules and office routines. By the 20th century, caffeine was no longer seen as a drug at all but as a necessity of modern life.
Its downsides—dependence, sleep disruption, anxiety—were normalized or joked about. In recent decades, branding completed the transformation. Coffee became lifestyle. The stimulant disappeared behind aesthetics and identity.
The Class Divide in Addiction
The difference between caffeine and nicotine is not just historical. It is social.
Caffeine use is public, aesthetic, and professionally coded. Carrying a coffee cup signals busyness, productivity, and belonging in the middle class. Nicotine use—even in clean, low-risk forms—is discreet. It is not aestheticized. It is associated with coping rather than ambition.
Addictions favored by elites are rebranded as habits or wellness tools. Addictions associated with stress, manual labor, or marginal populations are framed as moral failings. This is why caffeine is indulgence and nicotine is degeneracy, even when the physiological effects are similar.
Where Public Health Went Wrong
Public health messaging relies on simplification. “Smoking kills” was effective and true. But over time, simplification hardened into distortion.
“Smoking kills” became “Nicotine is addictive,” which slid into “Nicotine is harmful,” and eventually into claims that there is “No safe level.” Dose, delivery, and comparative risk disappeared from the conversation.
Institutions now struggle to reverse course. Admitting that nicotine is not the primary harm agent would require acknowledging decades of misleading communication. It would require distinguishing adult use from youth use. It would require nuance.
Bureaucracies are bad at nuance.
So nicotine remains frozen at its worst historical moment: the age of the cigarette.
Why This Matters
This is not an academic debate. Millions of smokers could dramatically reduce their health risks by switching to non-combustion nicotine products. Countries that have allowed this—most notably Sweden—have seen smoking rates and tobacco-related mortality collapse. Countries that stigmatize or ban these alternatives preserve cigarette dominance.
At the same time, caffeine consumption continues to rise, including among adolescents, with little moral panic. Energy drinks are aggressively marketed. Sleep disruption and anxiety are treated as lifestyle issues, not public health emergencies.
The asymmetry is revealing.
Coffee as the Model Addiction
Caffeine succeeded culturally because it aligned with power. It supported work, not resistance. It fit office life. It could be branded as refinement. It never challenged institutional authority.
Nicotine, especially when used by working-class populations, became associated with stress relief, nonconformity, and failure to comply. That symbolism persisted long after the smoke could be removed.
Addictions are not judged by chemistry. They are judged by who uses them and whether they fit prevailing moral narratives.
Coffee passed the test. Nicotine did not.
The Core Error
The central mistake is confusing a molecule with a method. Nicotine did not cause the smoking epidemic. Combustion did. Once that distinction is restored, much of modern tobacco policy looks incoherent. Low-risk behaviors are treated as moral threats, while higher-risk behaviors are tolerated because they are culturally embedded.
This is not science. It is politics dressed up as health.
A Final Thought
If we applied the standards used against nicotine to caffeine, coffee would be regulated like a controlled substance. If we applied the standards used for caffeine to nicotine, pouches and vaping would be treated as unremarkable adult choices.
The rational approach is obvious: evaluate substances based on dose, delivery, and actual harm. Stop moralizing chemistry. Stop pretending that all addictions are equal. Nicotine is not harmless. Neither is caffeine. But both are far safer than the stories told about them.
This essay only scratches the surface. The strange moral history of nicotine, caffeine, and acceptable addiction exposes a much larger problem: modern institutions have forgotten how to reason about risk.
Addictions
Manitoba Is Doubling Down On A Failed Drug Policy

From the Frontier Centre for Public Policy
Manitoba is choosing to expand the same drug policy model that other provinces are abandoning, policies that normalize addiction while sidelining treatment, recovery, and public safety.
The New Democrat premier of British Columbia, David Eby, stood before reporters last spring and called his government’s decision to permit public drug use in certain spaces a failure.
The policy was part of the broader “harm reduction” strategy meant to address overdose deaths. Instead, it had stirred public anger, increased street disorder and had helped neither users nor the communities that host them. “We do not accept street disorder that makes communities feel unsafe,” Eby said. The province scrapped the plan.
In Alberta, the Conservative government began shutting down safer-supply prescribing due to concerns about drug diversion and misuse. The belief that more opioids can resolve the opioid crisis is losing credibility.
Ontario Progressive Conservatives are moving away from harm reduction by shutting down supervised consumption sites near schools and limiting safer-supply prescribing. Federal funding for programs is decreasing, and the province is shifting its focus to treatment models, even though not all sites are yet closed.
Yet amid these non-partisan reversals, Manitoba’s government has announced its intention to open a supervised drug-use site in Winnipeg. Premier Wab Kinew said, “We have too many Manitobans dying from overdose.” True. But it does not follow that repeating failed approaches will yield different results.
Reversing these failed policies is not a rejection of compassion. It is a recognition that good intentions do not produce good outcomes. Vancouver and Toronto have hosted supervised drug-use sites for years. The death toll keeps rising. Drug deaths in British Columbia topped 2,500 in 2023, even with the most expansive harm reduction infrastructure in the country. A peer-reviewed study published this year found that hospitalizations from opioid poisoning rose after B.C.’s safer-supply policy was implemented. Emergency department visits increased by more than three cases per 100,000 population, with no corresponding drop in fatal overdoses.
And the problem persists day to day. Paramedics in B.C. responded to nearly 4,000 overdose calls in July 2024 alone. The monthly call volume has exceeded 3,000 almost every month this year. These are signs of crisis management without a path to recovery.
There are consequences beyond public health. These policies change the character of neighbourhoods. Businesses suffer. Residents feel unsafe. And most tragically, the person using drugs is offered little more than a cot, a nurse and a quiet signal to continue. Real help, like treatment, housing and purpose, remains out of reach.
Somewhere along the way, bureaucracies stopped asking what recovery looks like. They have settled for managing human decline. They call it compassion. But it is really surrender, wrapped in medical language.
Harm reduction had its time. It made sense when it first emerged, during the AIDS crisis, when dirty needles spread HIV. Back then, the goal was to stop a deadly virus. Today, that purpose has been lost.
When policy drifts into ideology, reality becomes an afterthought. Underneath today’s approach is the belief that drug use is inevitable, that people cannot change, that liberty means letting others fade away quietly. These ideas do not reflect science. They do not reflect hope. They reflect despair. They reflect a politics that prioritizes the appearance of compassion over effectiveness.
What Manitoba needs is treatment access that meets the scale of the problem. That means detox beds, recovery homes and long-term care focused on restoring lives. These may not generate the desired headlines, but they work. They are demanding. They are slow. And they offer respect to the person behind the addiction.
There are no shortcuts. No policy will undo decades of pain overnight. But a policy that keeps people stuck using is not mercy. It is maintenance with no way out.
A government that believes in its people should not copy failure.
Marco Navarro-Genie is vice-president of research at the Frontier Centre for Public Policy and co-author, with Barry Cooper, of Canada’s COVID: The Story of a Pandemic Moral Panic (2023).
-

 Frontier Centre for Public Policy15 hours ago
Frontier Centre for Public Policy15 hours agoIs Canada still worth the sacrifice for immigrants?
-

 Business15 hours ago
Business15 hours agoPolicy uncertainty continues to damage Canada’s mining potential
-

 Bruce Dowbiggin15 hours ago
Bruce Dowbiggin15 hours agoThe Olympic Shutout: No Quebec Players Invited For Canada
-

 Canadian Energy Centre15 hours ago
Canadian Energy Centre15 hours agoFive reasons why 2026 could mark a turning point for major export expansions
-

 International13 hours ago
International13 hours agoNetwork of Nonprofits with Marxist and CCP Ties, and Elected Socialists Race to Counter Washington’s Narrative of the Maduro Raid
-

 Opinion2 days ago
Opinion2 days agoHell freezes over, CTV’s fabrication of fake news and our 2026 forecast is still searching for sunshine
-
 COVID-191 day ago
COVID-191 day agoA new study proves, yet again, that the mRNA Covid jabs should NEVER have been approved for young people.
-

 Alberta12 hours ago
Alberta12 hours agoTrump’s Venezuela Geopolitical Earthquake Shakes up Canada’s Plans as a “Net Zero” Energy Superpower






