Alberta
Healthcare Overhaul – Services to be provided by nurses in their own clinics

Strengthening primary care with nurse practitioners
Alberta’s government is expanding opportunities for nurse practitioners to give Albertans greater access to a regular primary care provider when and where they need one.
Too many Albertans cannot find a regular family doctor or have trouble getting an appointment with the one they have. Alberta’s government continues to support and stabilize primary health care across the province by enabling nurse practitioners to open their own clinics, take on patients and offer services based on their scope of practice, training and expertise. Typically nurse practitioners can provide about 80 per cent of the medical services a family physician provides, and this will be reflected in the compensation model when it’s finalized.
Nurse practitioners have completed graduate studies and are regulated by the College of Registered Nurses of Alberta. Like other regulated professions, all nurse practitioners must meet minimum requirements to practise and follow standards set by their regulatory college.
“Nurse practitioners are highly trained and valued medical professionals. By enabling them to open their own clinics, we are ensuring Albertans can more easily access the care they need. This is a significant improvement in our primary health care system that will benefit patients and help improve the overall health and health outcomes of Alberta families.”
As the province enables nurse practitioners to do more of the work they are trained to do, a new compensation model will be created to encourage them to operate independently, adding much-needed capacity to Alberta’s primary care system. Nurse practitioners are extensively trained in their graduate studies to assess, diagnose, treat, order and interpret diagnostic tests, prescribe medications, make referrals to a specialist and manage a person’s overall care.
In addition, through a $2-million grant over the next three years, the Nurse Practitioner Association of Alberta will help to implement a compensation model, recruit other nurse practitioners to participate and provide supports as they work to set up their own clinics.
“There is no doubt about it, we need more health professionals providing primary health care to Albertans. Nurse practitioners are skilled health care professionals who play vital roles in modern health care. This model has the potential to add capacity in communities across the province and help so many Albertans gain access to a regular primary care provider.”
The new compensation model will be phased in and is expected to launch in early 2024 when nurse practitioners who want to go into independent practice will be asked to submit expressions of interest. The model is expected to include payment for a specified number of clinical hours and other commitments, such as caring for a certain number of patients.
“The Nurse Practitioner Association of Alberta is thrilled for the opportunity to support Albertans across the province in accessing a care provider in all health care environments, not just primary care. With this announcement and this grant, the association will be perfectly positioned to ensure that our members will be fully prepared to meet the needs of Albertans in both urban and rural communities. Until now, accessing a nurse practitioner has been challenging. This announcement ends those challenges. The NPAA looks forward to working with Alberta Health to get clinics open and to support NPs in being able to do the work that they are trained to do.”
Nurse practitioners who opt into the compensation model will also qualify for caseload supports once their patient caseloads are established, as announced on Oct. 18. The three-year $57-million support program will help primary health care providers manage an increasing number of patients. Each provider has the potential to receive up to $10,000 annually.
“The shortage of health care professionals in rural communities has always been a challenge that required innovative solutions. The new nurse practitioner model actively addresses this need by enhancing and expanding rural health care deliveries. This new initiative will enable rural Albertans to have better access to primary health care close to home.”
Alberta’s government will continue working with the Nurse Practitioner Association of Alberta and the College of Registered Nurses of Alberta as the compensation model is implemented.
Related information
Related news
- Strengthening health care: Improving access for all (Oct 18, 2023)
Alberta
Red Deer Justice Centre Grand Opening: Building access to justice for Albertans

The new Red Deer Justice Centre will help Albertans resolve their legal matters faster.
Albertans deserve to have access to a fair, accessible and transparent justice system. Modernizing Alberta’s courthouse infrastructure will help make sure Alberta’s justice system runs efficiently and meets the needs of the province’s growing population.
Alberta’s government has invested $191 million to build the new Red Deer Justice Centre, increasing the number of courtrooms from eight to 12, allowing more cases to be heard at one time.
“Modern, accessible courthouses and streamlined services not only strengthen our justice
system – they build safer, stronger communities across the province. Investing in the new Red Deer Justice Centre is vital to helping our justice system operate more efficiently, and will give people in Red Deer and across central Alberta better access to justice.”

Government of Alberta and Judiciary representatives with special guests at the Red Deer Justice Centre plaque unveiling event April 22, 2025.
On March 3, all court services in Red Deer began operating out of the new justice centre. The new justice centre has 12 courtrooms fully built and equipped with video-conference equipment to allow witnesses to attend remotely if they cannot travel, and vulnerable witnesses to testify from outside the courtroom.
The new justice centre also has spaces for people taking alternative approaches to the traditional courtroom trial process, with the three new suites for judicial dispute resolution services, a specific suite for other dispute resolution services, such as family mediation and civil mediation, and a new Indigenous courtroom with dedicated venting for smudging purposes.
“We are very excited about this new courthouse for central Alberta. Investing in the places where people seek justice shows respect for the rights of all Albertans. The Red Deer Justice Centre fills a significant infrastructure need for this rapidly growing part of the province. It is also an important symbol of the rule of law, meaning that none of us are above the law, and there is an independent judiciary to decide disputes. This is essential for a healthy functioning democracy.”
“Public safety and access to justice go hand in hand. With this investment in the new Red Deer Justice Centre, Alberta’s government is ensuring that communities are safer, legal matters are resolved more efficiently and all Albertans get the support they need.”
“This state-of-the-art facility will serve the people of Red Deer and surrounding communities for generations. Our team at Infrastructure is incredibly proud of the work done to plan, design and build this project. I want to thank everyone, at all levels, who helped make this project a reality.”
Budget 2025 is meeting the challenge faced by Alberta with continued investments in education and health, lower taxes for families and a focus on the economy.

Quick facts
- The new Red Deer Justice Centre is 312,000 sq ft (29,000 m2). (The old courthouse is 98,780 sq ft (9,177 m2)).
- The approved project funding for the Red Deer Justice Centre is about $191 million.
Alberta
Made in Alberta! Province makes it easier to support local products with Buy Local program

Show your Alberta side. Buy Local. |
When the going gets tough, Albertans stick together. That’s why Alberta’s government is launching a new campaign to benefit hard-working Albertans.
Global uncertainty is threatening the livelihoods of hard-working Alberta farmers, ranchers, processors and their families. The ‘Buy Local’ campaign, recently launched by Alberta’s government, encourages consumers to eat, drink and buy local to show our unified support for the province’s agriculture and food industry.
The government’s ‘Buy Local’ campaign encourages consumers to buy products from Alberta’s hard-working farmers, ranchers and food processors that produce safe, nutritious food for Albertans, Canadians and the world.
“It’s time to let these hard-working Albertans know we have their back. Now, more than ever, we need to shop local and buy made-in-Alberta products. The next time you are grocery shopping or go out for dinner or a drink with your friends or family, support local to demonstrate your Alberta pride. We are pleased tariffs don’t impact the ag industry right now and will keep advocating for our ag industry.”
Alberta’s government supports consumer choice. We are providing tools to help folks easily identify Alberta- and Canadian-made foods and products. Choosing local products keeps Albertans’ hard-earned dollars in our province. Whether it is farm-fresh vegetables, potatoes, honey, craft beer, frozen food or our world-renowned beef, Alberta has an abundance of fresh foods produced right on our doorstep.
Quick facts
- This summer, Albertans can support local at more than 150 farmers’ markets across the province and meet the folks who make, bake and grow our food.
- In March 2023, the Alberta government launched the ‘Made in Alberta’ voluntary food and beverage labelling program to support local agriculture and food sectors.
- Through direct connections with processors, the program has created the momentum to continue expanding consumer awareness about the ‘Made in Alberta’ label to help shoppers quickly identify foods and beverages produced in our province.
- Made in Alberta product catalogue website
Related information
-

 Business2 days ago
Business2 days agoIs Government Inflation Reporting Accurate?
-

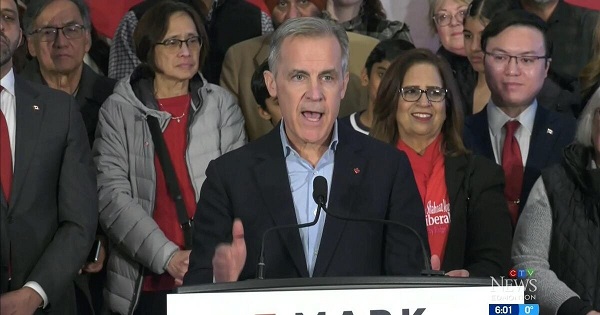
 2025 Federal Election2 days ago
2025 Federal Election2 days agoCarney’s Hidden Climate Finance Agenda
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoWhen it comes to pipelines, Carney’s words flow both ways
-
 2025 Federal Election2 days ago
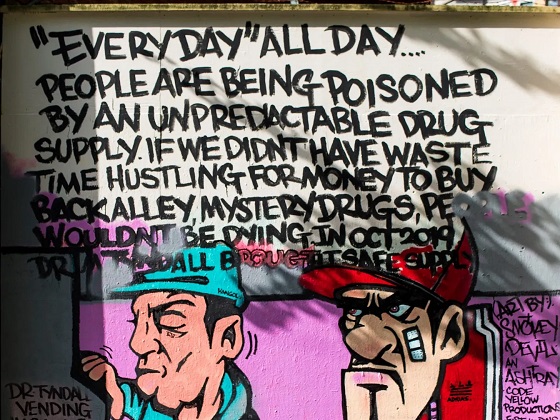
2025 Federal Election2 days agoStudy links B.C.’s drug policies to more overdoses, but researchers urge caution
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPolls say Canadians will give Trump what he wants, a Carney victory.
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoCarney Liberals pledge to follow ‘gender-based goals analysis’ in all government policy
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoPoilievre’s Conservatives promise to repeal policy allowing male criminals in female jails
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoTrump Has Driven Canadians Crazy. This Is How Crazy.