Health
UK to ban puberty blockers for minors indefinitely

From LifeSiteNews
UK Health Secretary Wes Streeting announced Wednesday that he will indefinitely extend a ban on puberty blockers for minors under the age of 18. The only exception is for clinical trials.
Puberty blockers will be banned indefinitely in the U.K. for under 18-year-olds, except for clinical trials.
In May of this year, the then-government of Rishi Sunak used emergency legislation to temporarily ban puberty blockers for minors. Health Secretary Wes Streeting announced on Wednesday that he will indefinitely extend the ban on the supply and sale of puberty blockers.
The Department of Health cited the Commission on Human Medicines’ (CHM) expert advice that said there was “currently an unacceptable safety risk in the continued prescription of puberty blockers to children.”
The U.K.’s National Health Service (NHS) already halted the prescription of puberty blockers to children in March. In May, the then-Conservative government introduced a ban, preventing the prescription of puberty blockers by European or private prescribers and legally restricting the NHS’s use of the drugs to clinical trials.
The ban was upheld in July by the High Court after pro-LGBT activists brought a challenge to the ruling because they “were concerned for the safety and welfare of young trans people in the UK.”
The prohibition of prescribing harmful puberty blockers for children was prompted by the Cass Review, an extensive report by pediatrician Dr. Hilary Cass that pointed out the significant risks of the medication and the lack of evidence regarding the alleged benefits of puberty blockers.
Health Secretary Streeting said that he would “always put the safety of children first” and added that his approach would “continue to be informed by Dr [Hilary] Cass’s review, which found there was insufficient evidence to show puberty blockers were safe for under-18s.”
Earlier on the same day that the nationwide ban was announced, the Parliament of Northern Ireland had voted unanimously to permanently ban puberty blockers in order to prevent the province from becoming a “back door” for the distribution of the drugs in the U.K.
The co-founder of the advocacy group “Our Duty,” Keith Jordan, applauded the decision by Northern Ireland to ban the harmful drugs indefinitely.
“This marks a significant step in safeguarding children, preventing Northern Ireland from becoming a ‘back door’ for these unregulated treatments – a concern highlighted by Susie Green’s earlier attempts to circumvent mainland restrictions,” he said.
Susie Green is a transgender activist who set up a clinic in Northern Ireland in an attempt to circumvent the restrictions in mainland Britain.
“However, we must remain vigilant, as the demand for these drugs may drive young people to unregulated, dangerous sources,” Jordan stressed, urging lawmakers to prioritize safeguarding children.
Alberta
A Christmas wish list for health-care reform

From the Fraser Institute
By Nadeem Esmail and Mackenzie Moir
It’s an exciting time in Canadian health-care policy. But even the slew of new reforms in Alberta only go part of the way to using all the policy tools employed by high performing universal health-care systems.
For 2026, for the sake of Canadian patients, let’s hope Alberta stays the path on changes to how hospitals are paid and allowing some private purchases of health care, and that other provinces start to catch up.
While Alberta’s new reforms were welcome news this year, it’s clear Canada’s health-care system continued to struggle. Canadians were reminded by our annual comparison of health care systems that they pay for one of the developed world’s most expensive universal health-care systems, yet have some of the fewest physicians and hospital beds, while waiting in some of the longest queues.
And speaking of queues, wait times across Canada for non-emergency care reached the second-highest level ever measured at 28.6 weeks from general practitioner referral to actual treatment. That’s more than triple the wait of the early 1990s despite decades of government promises and spending commitments. Other work found that at least 23,746 patients died while waiting for care, and nearly 1.3 million Canadians left our overcrowded emergency rooms without being treated.
At least one province has shown a genuine willingness to do something about these problems.
The Smith government in Alberta announced early in the year that it would move towards paying hospitals per-patient treated as opposed to a fixed annual budget, a policy approach that Quebec has been working on for years. Albertans will also soon be able purchase, at least in a limited way, some diagnostic and surgical services for themselves, which is again already possible in Quebec. Alberta has also gone a step further by allowing physicians to work in both public and private settings.
While controversial in Canada, these approaches simply mirror what is being done in all of the developed world’s top-performing universal health-care systems. Australia, the Netherlands, Germany and Switzerland all pay their hospitals per patient treated, and allow patients the opportunity to purchase care privately if they wish. They all also have better and faster universally accessible health care than Canada’s provinces provide, while spending a little more (Switzerland) or less (Australia, Germany, the Netherlands) than we do.
While these reforms are clearly a step in the right direction, there’s more to be done.
Even if we include Alberta’s reforms, these countries still do some very important things differently.
Critically, all of these countries expect patients to pay a small amount for their universally accessible services. The reasoning is straightforward: we all spend our own money more carefully than we spend someone else’s, and patients will make more informed decisions about when and where it’s best to access the health-care system when they have to pay a little out of pocket.
The evidence around this policy is clear—with appropriate safeguards to protect the very ill and exemptions for lower-income and other vulnerable populations, the demand for outpatient healthcare services falls, reducing delays and freeing up resources for others.
Charging patients even small amounts for care would of course violate the Canada Health Act, but it would also emulate the approach of 100 per cent of the developed world’s top-performing health-care systems. In this case, violating outdated federal policy means better universal health care for Canadians.
These top-performing countries also see the private sector and innovative entrepreneurs as partners in delivering universal health care. A relationship that is far different from the limited individual contracts some provinces have with private clinics and surgical centres to provide care in Canada. In these other countries, even full-service hospitals are operated by private providers. Importantly, partnering with innovative private providers, even hospitals, to deliver universal health care does not violate the Canada Health Act.
So, while Alberta has made strides this past year moving towards the well-established higher performance policy approach followed elsewhere, the Smith government remains at least a couple steps short of truly adopting a more Australian or European approach for health care. And other provinces have yet to even get to where Alberta will soon be.
Let’s hope in 2026 that Alberta keeps moving towards a truly world class universal health-care experience for patients, and that the other provinces catch up.
Health
FDA warns ‘breast binder’ manufacturers to stop marketing to gender-confused girls

From LifeSiteNews
Dr. Marty Makary took aim at the transgender-medical-industrial complex that has exploded in recent years during a recent press conference.
Food and Drug Administration (FDA) commissioner Dr. Marty Makary has sternly warned companies manufacturing “breast binders” to cease marketing and supplying their product to gender-confused girls seeking to make their bodies appear masculine.
“Today the FDA is taking action,” said Makary in a press conference. “We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.”
“Breast binders are a class one medical device with legitimate medical users, such as being used by women after breast cancer surgery,” but “these binders are not benign,” he cautioned. “Long-term usage has been associated with pain, compromised lung function, and even difficulty breast feeding later in life.”
“The warning letters will formally notify the companies of their significant regulatory violations and require prompt corrective action,” said the FDA head.
.@DrMakaryFDA: “Today the FDA is taking action. We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.” pic.twitter.com/6JNAy36223
— HHS Rapid Response (@HHSResponse) December 18, 2025
The warning letter addressed to California manufacturer, GenderBender, notes that the company’s website states that “[c]hest binding is the practice of compressing breast mass into a more masculine shape, often done in the LGBTQ community for gender euphoria.”
“Your firm should take prompt action to address any violations identified in this letter. Failure to adequately address this matter may result in regulatory action being initiated by the FDA without further notice. These actions include, but are not limited to, seizure and injunction,” advised the FDA.
During his presentation, Makary took aim at the transgender-medical-industrial complex that has exploded in recent years.
“One of the most barbaric features of a society is the genital mutilation of its children,” observed Makary.
“Pushing transgender ideology in children is predatory, it’s wrong, and it needs to stop,” he declared.
“This ideology is a belief system that some teachers, some pediatricians, and others are selling to children without their parents knowing sometimes, or with a deliberate attempt to remove parents from the decision making,” Makary explained.
To witness society “putting kids on a path of chest binders, drugs, castration, mastectomies, and other procedures is a path that now many kids regret,” he lamented, as he pointed to Chloe Cole, who has reverted to her God-given femininity after undergoing so-called “gender-affirming” surgery as a teen.
Cole is a leading voice for young people who have “detransitioned” after having medically, surgically, and socially attempted to “transition” to a member of the opposite sex.
.@DrMakaryFDA: “Pushing transgender ideology in children is predatory, it's wrong, and it needs to stop.” pic.twitter.com/TXxWNEtNZk
— HHS Rapid Response (@HHSResponse) December 18, 2025
-

 International2 days ago
International2 days agoGeorgia county admits illegally certifying 315k ballots in 2020 presidential election
-

 Alberta1 day ago
Alberta1 day agoA Christmas wish list for health-care reform
-

 Business1 day ago
Business1 day agoSome Of The Wackiest Things Featured In Rand Paul’s New Report Alleging $1,639,135,969,608 In Gov’t Waste
-

 Energy1 day ago
Energy1 day ago‘The electric story is over’
-

 Business2 days ago
Business2 days agoWarning Canada: China’s Economic Miracle Was Built on Mass Displacement
-

 Agriculture2 days ago
Agriculture2 days agoThe Climate Argument Against Livestock Doesn’t Add Up
-

 International19 hours ago
International19 hours ago$2.6 million raised for man who wrestled shotgun from Bondi Beach terrorist
-
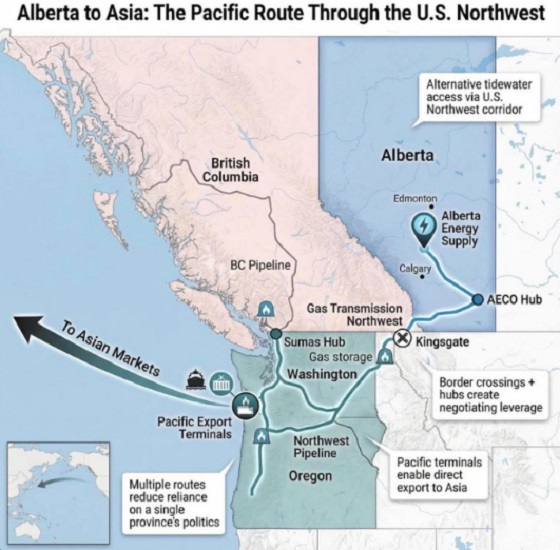
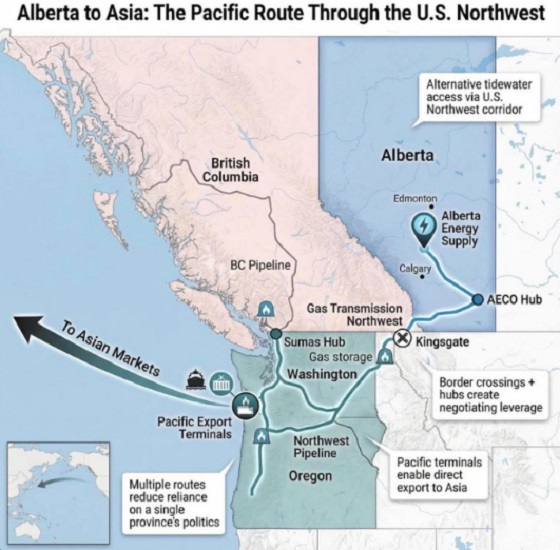 Alberta2 days ago
Alberta2 days agoWhat are the odds of a pipeline through the American Pacific Northwest