Health
Time for an intervention – an urgent call to end “gender-affirming” treatments for children

From the Macdonald Laurier Institute
By J. Edward Les
Despite the Cass Review’s alarming findings, trans activists and their enablers in the medical professions continue to push kids into having dangerous, life-altering surgeries and hormone-blocking treatments. It needs to stop.
If nothing else, the scathing final report of the Cass Review released this week (but commissioned four years ago to investigate the disturbing practices of the UK’s Gender Identity Service), is a reminder that doctors historically are guilty of many sins.
Take the Tuskegee syphilis study, one of the greatest stains on the medical profession, in which impoverished syphilis-infected black men were knowingly deprived of therapy so that researchers could study the natural history of untreated disease.
Or consider the repugnant New Zealand cervical cancer study in the 1960s and 1970s, which left women untreated for years so that researchers could learn how cervical cancer progressed. Or the Swedish efforts to solidify the link between sugar and dental decay by feeding copious amounts of sweets to the mentally handicapped.
The doctors behind such scandals undoubtedly felt they were advancing scientific inquiry in pursuit of the greater good; but they clearly stampeded far beyond the boundaries of ethical medical practice.
More common by far, though, are medical “sins” committed unknowingly, such as when doctors prescribe toxic treatments to patients in the mistaken belief that they are beneficial. When physicians in Europe and Canada latched onto thalidomide in the late 1950s and early 1960s, for instance, they thought it was a wonder drug for morning sickness. Only the fine work of Dr. Francis Kelsey, an astute pharmacist at the FDA, prevented the ensuing birth-defects tragedy from being visited upon American women and children.
And when Oxycontin hit the medical marketplace in the 1990s, physicians embraced it as a marvellous — and supposedly non-addictive — solution to their patients’ pain. But the drug was simply another synthetic derivative of opium, and every bit as addictive; its use triggered a massive opioid overdose crisis — still ongoing today — that has killed hundreds of thousands and ruined the lives of countless individuals and their families.
Physicians in the latter instances weren’t driven by malevolence; but rather by a deep-seated desire to help patients. That wish, compounded by extreme busy-ness, repeatedly seduces doctors into unwarranted faith in untested therapies.
And no discipline in medicine, arguably, is more frequently led astray by the siren song of shiny new things than the field of psychiatry. Which is understandable, perhaps, given the nature of psychiatric practice. Categorizations of mental disorders — and the methods used to treat them — are based almost entirely on consensus opinion, rather than on direct measurement. Contrast that with other domains of medical practice: appendicitis is diagnosed by imaging the infected organ, and then cured by surgically removing the inflamed tissue; diabetes is detected by measuring elevated blood sugar, and then corrected by the administration of insulin; elevated blood pressure is calibrated in millimetres of mercury, and then effectively reduced with antihypertensives; and so on.
But mental disturbances remain largely the stuff of conjecture — learned conjecture, mind you, but conjecture, nonetheless. The Diagnostic and Statistical Manual of Mental Disorders, the “bible” of mental health professionals, is the collective effort of groups of tall foreheads gathered around conference tables opining on the various perturbations of the human mind. Imprecise definitions abound, with heaps of overlap between conditions.
The current version (DSM-5) describes schizophrenia, for example, as occurring on a spectrum of “abnormalities in one or more of the following five domains: delusions, hallucinations, disorganized thinking (speech), grossly disorganized or abnormal motor behavior (including catatonia), and negative symptoms.” Each of these five domains is open to professional interpretation; and what’s more, the schizophrenia spectrum is further subdivided into ten sub-categories.
That theme runs through the entire manual – and imprecise definitions lead on to imprecise solutions. Given the blurred indications for starting, balancing, and stopping medications, it’s no accident that many mentally unwell patients languish on ever-changing cocktails of mind-altering drugs.
None of which is to downplay the enormous importance of psychiatry, which does much to address human suffering amidst unimaginable complexity; its practitioners are among the brightest and most capable members of the medical profession. But by its very nature the discipline is submerged in — and handicapped by — uncertainty. It’s unsurprising, then, that mental health professionals desperate for effective treatments are susceptible to being misled.
The dark history of frontal lobotomies, seized upon by psychiatrists as a miracle cure but long relegated to the trash heap of medical barbarism, is well known. The procedure (which garnered its inventor the Nobel Prize in Medicine) basically consisted of driving an ice pick through patients’ eye sockets to destroy their frontal lobes; thousands of patients were permanently maimed before saner heads prevailed and the practice was halted. Many of its victims were gay men: “conversion therapy” with a literal, brain-altering “punch.”
Similarly, the fabricated “recovered memories of sexual abuse” saga of the 1980s and early 1990s suckered mental health practitioners into believing it was legitimate. Hundreds of professional careers were built on the “therapy” before it was all exposed as a fraud, leaving many lives ruined, families torn asunder, and scores of innocent men imprisoned or dead from suicide. In a 2005 review, Harvard psychology professor Richard McNally pegged the recovered memory movement as “the worst catastrophe to befall the mental health field since the lobotomy era.”
Until now, that is. That scandal pales in comparison to the “gender transition/gender affirming care” craze that has befogged the medical profession in recent years.
Without a shred of supporting scientific evidence, many doctors — led by psychiatrists, but aided and abetted by endocrinologists, surgeons, pediatricians, and family doctors — have bought into the mystical notion of gender fluidity. What was previously recognized as “gender identity disorder” was rebranded as gender “dysphoria” and recast as part of the normal spectrum of human experience, the basic truth of binary mammalian biology simply discarded in favour of the fiction that it’s possible to convert from one sex to another.
Much suffering has ensued. The enabling of biological males’ invasion of women’s spaces, rape shelters, prisons, and sports is bad enough. But what is being done to children is the stuff of horror movies: doctors are using medications to block physiological puberty as prologue to cross-gender hormones, genital-revising surgery, and a lifetime of infertility and medical misery — and labelling the entire sordid mess as gender-affirming care.
The malignant fad began innocently enough, with a Dutch effort in the late 1980s and early 1990s to improve the lot of transgendered adults troubled by the disconnect between their physical bodies and their gender identity. Those clinicians’ motivations were defensible, perhaps; but their research was riddled with ethical lapses and methodological errors and has since been thoroughly discredited. Yet their methods “escaped the lab”, with the international medical community adopting them as a template for managing gender-confused children, and the World Professional Association for Transgender Health (WPATH) enshrining them as “standard of care.” Then, as American social psychologist Jonathan Haidt is the latest to observe, the rise of social media torqued the trend into a craze by convincing hordes of adolescents they were “trans.” Which is how we ended up where we are today, with science replaced by rabid ideology — and with condemnation heaped upon anyone who dares to challenge it.
An explanation sometimes offered for the massive spike in gender-confused kids seeking “affirmation” in the past fifteen years is that today it’s “safe” for kids to express themselves, as if this phenomenon always existed but that — as with homosexuality — it was “closeted” due to stigma. Yet are we really expected to believe that the giants of empirical research into childhood development —brilliant minds like Jean Piaget, Eric Erikson, Lev Vygotsky, and Lawrence Kohlberg — somehow missed entirely the trait of mutable “gender identity” amongst all the other childhood traits they were studying? That’s nonsense, of course. They didn’t miss it — because it isn’t real.
The fog is beginning to dissipate, thankfully. Multiple jurisdictions around the world, including the UK, Sweden, Norway, Finland, and France have begun to realize the grave harm that has been done, and are pulling back from — or halting altogether — the practice of blocking puberty. And the final Cass Report goes even further, taking square aim at the dangerous practice of social transitioning and concluding that it’s “not a neutral act” but instead presents risk of grave psychological harm.
All of which places Canada in a rather awkward position. Because in December of 2021 parliamentarians gave unanimous consent to Bill C-4, which bans conversion therapy, including “any practice, service or treatment designed to change a person’s gender identity.” It’s since been a crime in Canada, punishable by up to five years in prison, to try to help your child feel comfortable with his or her sex.
As far as I know, no one has been charged, let alone imprisoned, since the bill was passed into law. But it certainly has cast a chill on the willingness of providers to deliver appropriate counselling to gender-confused children: few dare to risk it.
A conversion therapy ban had been in the works for years, triggered by concerns about disturbing and harmful practices targeting gay children. But by the time the bill was presented in its final form to Parliament for a vote it had been hijacked by trans activists, with its content perverted to the degree that there is more language in the legislation speaking to gender identity than to homosexuality.
To be clear, likening homosexuality to pediatric “gender fluidity” is a category error, akin to comparing apples to elephants. The one is an innate sexual orientation, the acceptance of which requires simply leaving people be to live their lives and love whomever they wish; the other is wholly imaginary, the acceptance of which mandates irreversible medical (and often surgical) intervention and the transformation of children into lifelong (and usually infertile) medical patients.
And the real “elephant” in the room is that in a troubling number of cases pediatric trans care is conversion therapy for gay children because for some people, it’s more acceptable to be trans than it is to be gay.
Bill C-4 received unanimous endorsement from all parliamentarians, including from Pierre Poilievre, now the leader of the Conservative Party. No debate. No analysis. Just high-fives all around for the television cameras.
It’s possible that many of the opposition MPs hastening to support the ban did so for fear of being painted as bigots. Yet the primary responsibility of an opposition party in any healthy democracy is to oppose, even when it’s unpopular. In 2015, when NDP Opposition leader Tom Mulcair faced withering criticism for resisting anti-terror legislation tabled by Stephen Harper’s Conservative government, he cited John Diefenbaker’s comments on the role of political opposition:
“The reading of history proves that freedom always dies when criticism ends… The Opposition finds fault; it suggests amendments; it asks questions and elicits information; it arouses, educates, and moulds public opinion by voice and vote… It must scrutinize every action of the government and, in doing so, prevents the shortcuts through democratic procedure that governments like to make.”
In the case of Bill C-4 the Conservatives did none of that. And by abdicating their responsibility they helped drive a metaphorical ice pick into the futures of scores of innocent children, destroying forever their prospects for normal, healthy lives.
We’re long overdue for a “conversion”: a conversion back to the light of reason, a conversion back to evidence-based care of children.
In 1962, when the harms of thalidomide became known, it was withdrawn from the Canadian market. In 2024, now that the serious harms of “gender-affirming care” have been exposed, it remains an open question as to when Canada’s doctors and politicians will finally take the difficult step of admitting that they got it wrong and put a stop to the practice.
Dr. Edward Les is a pediatrician in Calgary who writes on politics, social issues, and other matters.
armed forces
Yet another struggling soldier says Veteran Affairs Canada offered him euthanasia

From LifeSiteNews
‘It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself.’
Yet another Canadian combat veteran has come forward to reveal that when he sought help, he was instead offered euthanasia.
David Baltzer, who served two tours in Afghanistan with the Princess Patricia’s Canadian Light Infantry, revealed to the Toronto Sun that he was offered euthanasia on December 23, 2019—making him, as the Sun noted, “among the first Canadian soldiers offered therapeutic suicide by the federal government.”
Baltzer had been having a disagreement with his existing caseworker, when assisted suicide was brought up in in call with a different agent from Veteran Affairs Canada.
“It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself,” Baltzer told the Sun.“I was in my lowest down point, it was just before Christmas. He says to me, ‘I would like to make a suggestion for you. Keep an open mind, think about it, you’ve tried all this and nothing seems to be working, but have you thought about medical-assisted suicide?’”
Baltzer was stunned. “It just seems to me that they just want us to be like ‘f–k this, I give up, this sucks, I’d rather just take my own life,’” he said. “That’s how I honestly felt.”
Baltzer, who is from St. Catharines, Ontario, joined up at age 17, and moved to Manitoba to join the Princess Patricia’s Canadian Light Infantry, one of Canada’s elite units. He headed to Afghanistan in 2006. The Sun noted that he “was among Canada’s first troops deployed to Afghanistan as part Operation Athena, where he served two tours and saw plenty of combat.”
“We went out on long-range patrols trying to find the Taliban, and that’s exactly what we did,” Baltzer said. “The best way I can describe it, it was like Black Hawk Down — all of the sudden the s–t hit the fan and I was like ‘wow, we’re fighting, who would have thought? Canada hasn’t fought like this since the Korean War.”
After returning from Afghanistan, Baltzer says he was offered counselling by Veteran Affairs Canada, but it “was of little help,” and he began to self-medicate for his trauma through substance abuse (he noted that he is, thankfully, doing well today). Baltzer’s story is part of a growing scandal. As the Sun reported:
A key figure shedding light on the VAC MAID scandal was CAF veteran Mark Meincke, whose trauma-recovery podcast Operation Tango Romeo broke the story. ‘Veterans, especially combat veterans, usually don’t reach out for help until like a year longer than they should’ve,’ Meincke said, telling the Sun he waited over two decades before seeking help.
‘We’re desperate by the time we put our hands up for help. Offering MAID is like throwing a cinderblock instead of a life preserver.’ Meincke said Baltzer’s story shoots down VAC’s assertions blaming one caseworker for offering MAID to veterans, and suggests the problem is far more serious than some rogue public servant.
‘It had to have been policy. because it’s just too many people in too many provinces,” Meincke told the Sun. “Every province has service agents from that province.’
Veterans Affairs Canada claimed in 2022 that between four and 20 veterans had been offered assisted suicide; Meincke “personally knows of five, and said the actual number’s likely close to 20.” In a previous investigation, VAC claimed that only one caseworker was responsible—at least for the four confirmed cases—and that the person “was lo longer employed with VAC.” Baltzer says VAC should have military vets as caseworkers, rather than civilians who can’t understand what vets have been through.
To date, no federal party leader has referenced Canada’s ongoing euthanasia scandals during the 2025 election campaign.
2025 Federal Election
Study links B.C.’s drug policies to more overdoses, but researchers urge caution
By Alexandra Keeler
A study links B.C.’s safer supply and decriminalization to more opioid hospitalizations, but experts note its limitations
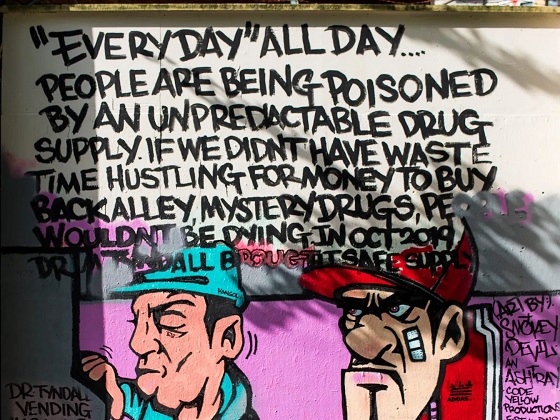
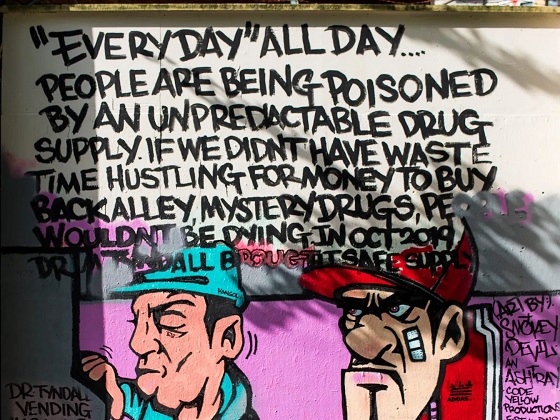
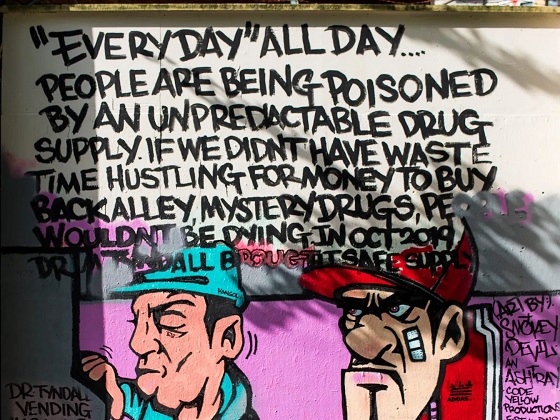
A new study says B.C.’s safer supply and decriminalization policies may have failed to reduce overdoses. Furthermore, the very policies designed to help drug users may have actually increased hospitalizations.
“Neither the safer opioid supply policy nor the decriminalization of drug possession appeared to mitigate the opioid crisis, and both were associated with an increase in opioid overdose hospitalizations,” the study says.
The study has sparked debate, with some pointing to it as proof that B.C.’s drug policies failed. Others have questioned the study’s methodology and conclusions.
“The question we want to know the answer to [but cannot] is how many opioid hospitalizations would have occurred had the policy not have been implemented,” said Michael Wallace, a biostatistician and associate professor at the University of Waterloo.
“We can never come up with truly definitive conclusions in cases such as this, no matter what data we have, short of being able to magically duplicate B.C.”
Jumping to conclusions
B.C.’s controversial safer supply policies provide drug users with prescription opioids as an alternative to toxic street drugs. Its decriminalization policy permitted drug users to possess otherwise illegal substances for personal use.
The peer-reviewed study was led by health economist Hai Nguyen and conducted by researchers from Memorial University in Newfoundland, the University of Manitoba and Weill Cornell Medicine, a medical school in New York City. It was published in the medical journal JAMA Health Forum on March 21.
The researchers used a statistical method to create a “synthetic” comparison group, since there is no ideal control group. The researchers then compared B.C. to other provinces to assess the impact of certain drug policies.
Examining data from 2016 to 2023, the study links B.C.’s safer supply policies to a 33 per cent rise in opioid hospitalizations.
The study says the province’s decriminalization policies further drove up hospitalizations by 58 per cent.
“Neither the safer supply policy nor the subsequent decriminalization of drug possession appeared to alleviate the opioid crisis,” the study concludes. “Instead, both were associated with an increase in opioid overdose hospitalizations.”
The B.C. government rolled back decriminalization in April 2024 in response to widespread concerns over public drug use. This February, the province also officially acknowledged that diversion of safer supply drugs does occur.
The study did not conclusively determine whether the increase in hospital visits was due to diverted safer supply opioids, the toxic illicit supply, or other factors.
“There was insufficient evidence to conclusively attribute an increase in opioid overdose deaths to these policy changes,” the study says.
Nguyen’s team had published an earlier, 2024 study in JAMA Internal Medicine that also linked safer supply to increased hospitalizations. However, it failed to control for key confounders such as employment rates and naloxone access. Their 2025 study better accounts for these variables using the synthetic comparison group method.
The study’s authors did not respond to Canadian Affairs’ requests for comment.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Correlation vs. causation
Chris Perlman, a health data and addiction expert at the University of Waterloo, says more studies are needed.
He believes the findings are weak, as they show correlation but not causation.
“The study provides a small signal that the rates of hospitalization have changed, but I wouldn’t conclude that it can be solely attributed to the safer supply and decrim[inalization] policy decisions,” said Perlman.
He also noted the rise in hospitalizations doesn’t necessarily mean more overdoses. Rather, more people may be reaching hospitals in time for treatment.
“Given that the [overdose] rate may have gone down, I wonder if we’re simply seeing an effect where more persons survive an overdose and actually receive treatment in hospital where they would have died in the pre-policy time period,” he said.
The Nguyen study acknowledges this possibility.
“The observed increase in opioid hospitalizations, without a corresponding increase in opioid deaths, may reflect greater willingness to seek medical assistance because decriminalization could reduce the stigma associated with drug use,” it says.
“However, it is also possible that reduced stigma and removal of criminal penalties facilitated the diversion of safer opioids, contributing to increased hospitalizations.”
Karen Urbanoski, an associate professor in the Public Health and Social Policy department at the University of Victoria, is more critical.
“The [study’s] findings do not warrant the conclusion that these policies are causally associated with increased hospitalization or overdose,” said Urbanoski, who also holds the Canada Research Chair in Substance Use, Addictions and Health Services.
Her team published a study in November 2023 that measured safer supply’s impact on mortality and acute care visits. It found safer supply opioids did reduce overdose deaths.
Critics, however, raised concerns that her study misrepresented its underlying data and showed no statistically significant reduction in deaths after accounting for confounding factors.
The Nguyen study differs from Urbanoski’s. While Urbanoski’s team focused on individual-level outcomes, the Nguyen study analyzed broader, population-level effects, including diversion.
Wallace, the biostatistician, agrees more individual-level data could strengthen analysis, but does not believe it undermines the study’s conclusions. Wallace thinks the researchers did their best with the available data they had.
“We do not have a ‘copy’ of B.C. where the policies weren’t implemented to compare with,” said Wallace.
B.C.’s overdose rate of 775 per 100,000 is well above the national average of 533.
Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, has been a vocal critic of B.C.’s decriminalization and safer supply policies.
“If the government doesn’t want to believe this study, well then I invite them to do a similar study,” she told reporters on March 27.
“Show us the evidence that they have failed to show us since 2020,” she added, referring to the year B.C. implemented safer supply.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Our content is always free – but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoStudy links B.C.’s drug policies to more overdoses, but researchers urge caution
-

 Business2 days ago
Business2 days agoIs Government Inflation Reporting Accurate?
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCarney’s Hidden Climate Finance Agenda
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoWhen it comes to pipelines, Carney’s words flow both ways
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPolls say Canadians will give Trump what he wants, a Carney victory.
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoThe Anhui Convergence: Chinese United Front Network Surfaces in Australian and Canadian Elections
-

 2025 Federal Election18 hours ago
2025 Federal Election18 hours agoPoilievre Campaigning To Build A Canadian Economic Fortress
-

 Automotive18 hours ago
Automotive18 hours agoCanadians’ Interest in Buying an EV Falls for Third Year in a Row