Addictions
The new drug agency tasked with improving Canada’s medication practices

By Alexandra Keeler
A recent report calls on the newly-created Canada’s Drug Agency to implement a strategy to improve prescription medication practices
As Canada moves toward establishing a national drug agency, a new report has outlined recommendations for a prescription medications strategy that the agency should be tasked with implementing.
The report, released July 26 by the Canadian Drug Agency Transition Office, calls on the newly established Canada’s Drug Agency to implement a nation-wide strategy for the appropriate use of prescription medications. The transition office is a temporary government initiative responsible for developing the drug agency’s mandate and plan.
“Part of the opioid crisis has been linked to prescribing particular medications, and the dependency that people can develop with respect to certain medications,” said Stephen Samis, chair of the Appropriate Use Advisory Committee, which helped guide the development of the medications strategy outlined in the report.
“If there’s a way to help get people off of those medications in a safe and effective way, and by the use of alternatives to the medication, that’s really important,” said Samis, who formerly served as deputy health minister in the Yukon.
Canada’s Drug Agency, which was first announced by Health Minister Mark Holland in December 2023, is tasked with managing and coordinating Canada’s pharmaceutical system across the provinces and territories. It has begun establishing advisory bodies, building partnerships and conducting research.
Under Canada’s proposed pharmacare legislation, the drug agency will also be responsible for identifying the essential prescription drugs to which Canadians should have access under pharmacare.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Primary care crisis
The report proposes six guiding principles for improving Canada’s prescription and medication use practices. These include providing more personalized primary care to patients, ensuring careful oversight of prescription medications and improving coordination between health-care providers.
Currently, more than one in five Canadian adults — about 6.5 million people — lack access to primary care, according to a May 2024 study in the Canadian Medical Association Journal. Primary care refers to health care that is regular and ongoing, such as doctor check-ups or management of chronic conditions.
“The crisis in primary care right now is really one of those potential barriers to people receiving appropriate medication with a provider that they have a relationship with,” said Samis.
The lack of access to primary care can lead to problems such as inconsistent prescribing, inadequate follow-up and insufficient patient education on prescription medications, the report says.
About 1.9 million Canadian seniors use at least one prescription medication inappropriately. This costs them and the health-care system an estimated $1.4 billion in direct and indirect costs, the report says.
“Benzodiazepines, sleeping pills … even things like medications that control heartburn. If people are on them for too long, [it] can have other kinds of side effects,” said Samis.
“Same thing with opioid related medications. It’s really important that people have medications they need so that they don’t develop dependencies.”
The report also notes that fragmented information systems and poor coordination between service providers complicate medication management — resulting in duplicate prescriptions, contradictory treatment plans and gaps in care.
“What happens often is that somebody is in primary care, and their data is over here,” said Samis. “They go into long-term care, and that information doesn’t follow them. They get prescribed new things in long-term care, they go into the hospital, then the long-term care information system might not be speaking to the hospital information system.”
‘Neutral space’
Samis says he is optimistic that Canada’s Drug Agency will be able to address some of the problematic medication practices identified in the report.
Samis will co-chair a new committee responsible for assisting with the implementation of the report’s recommendations.
“We have a diverse and knowledgeable group joining our newly established Appropriate Use Advisory Committee, with the inaugural meeting to take place on September 13,” a media relations spokesperson for Canada’s Drug Agency’s told Canadian Affairs in a written statement.
Samis envisions the agency as a “neutral space” to address health-care issues and resolve conflicts between governments and health-care providers.
“This approach avoids the conflicts that often arise between jurisdictions, levels of government, or between government and [health-care] providers,” he said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Break The Needle. Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
Addictions
Why B.C.’s new witnessed dosing guidelines are built to fail

Photo by Acceptable at English Wikipedia, ‘Two 1 mg pills of Hydromorphone, prescribed to me after surgery.’ [Licensed under CC BY-SA 3.0, via Wikimedia Commons]
By Alexandra Keeler
B.C. released new witnessed dosing guidelines for safer supply opioids. Experts say they are vague, loose and toothless
This February, B.C pledged to reintroduce witnessed dosing to its controversial safer supply program.
Safer supply programs provide prescription opioids to people who use drugs. Witnessed dosing requires patients to consume those prescribed opioids under the supervision of a health-care professional, rather than taking their drugs offsite.
The province said it was reintroducing witnessed dosing to “prevent the diversion of prescribed opioids and hold bad actors accountable.”
But experts are saying the government’s interim guidelines, released April 29, are fundamentally flawed.
“These guidelines — just as any guidelines for safer supply — do not align with addiction medicine best practices, period,” said Dr. Leonara Regenstreif, a primary care physician specializing in substance use disorders. Regenstreif is a founding member of Addiction Medicine Canada, an advocacy group that represents 23 addiction specialists.
Addiction physician Dr. Michael Lester, who is also a founding member of the group, goes further.
“Tweaking a treatment protocol that should not have been implemented in the first place without prior adequate study is not much of an advancement,” he said.
Witnessed dosing
Initially, B.C.’s safer supply program was generally administered through witnessed dosing. But in 2020, to facilitate access amidst pandemic restrictions, the province moved to “take-home dosing,” allowing patients to take their prescription opioids offsite.
After pandemic restrictions were lifted, the province did not initially return to witnessed dosing. Rather, it did so only recently, after a bombshell government report alleged more than 60 B.C. pharmacies were boosting sales by encouraging patients to fill unnecessary opioid prescriptions. This incentivized patients to sell their medications on the black market.
B.C.’s interim guidelines, developed by the BC Centre on Substance Use at the government’s request, now require all new safer supply patients to begin with witnessed dosing.
But for existing patients, the guidelines say prescribers have discretion to determine whether to require witnessed dosing. The guidelines define an existing patient as someone who was dispensed prescription opioids within the past 30 days.
The guidelines say exemptions to witnessed dosing are permitted under “extraordinary circumstances,” where witnessed dosing could destabilize the patient or where a prescriber uses “best clinical judgment” and determines diversion risk is “very low.”
Holes
Clinicians say the guidelines are deliberately vague.
Regenstreif described them as “wordy, deliberately confusing.” They enable prescribers to carry on as before, she says.
Lester agrees. Prescribers would be in compliance with these guidelines even if “none of their patients are transferred to witnessed dosing,” he said.
In his view, the guidelines will fail to meet their goal of curbing diversion.
And without witnessed dosing, diversion is nearly impossible to detect. “A patient can take one dose a day and sell seven — and this would be impossible to detect through urine testing,” Lester said.
He also says the guidelines do not remove the incentive for patients to sell their drugs to others. He cites estimates from Addiction Medicine Canada that clients can earn up to $20,000 annually by selling part of their prescribed supply.
“[Prescribed safer supply] can function as a form of basic income — except that the community is being flooded with addictive and dangerous opioids,” Lester said.
Regenstreif warns that patients who had been diverting may now receive unnecessarily high doses. “Now you’re going to give people a high dose of opioids who don’t take opioids,” she said.
She also says the guidelines leave out important details on adjusting doses for patients who do shift from take-home to witnessed dosing.
“If a doctor followed [the guidelines] to the word, and the patient followed it to the word, the patient would go into withdrawal,” she said.
The guidelines assume patients will swallow their pills under supervision, but many crush and inject them instead, Regenstreif says. Because swallowing is less potent, a higher dose may be needed.
“None of that is accounted for in this document,” she said.
Survival strategy
Some harm reduction advocates oppose a return to witnessed dosing, saying it will deter people from accessing a regulated drug supply.
Some also view diversion as a life-saving practice.
Diversion is “a harm reduction practice rooted in mutual aid,” says a 2022 document developed by the National Safer Supply Community of Practice, a group of clinicians and harm reduction advocates.
The group supports take-home dosing as part of a broader strategy to improve access to safer supply medications. In their document, they say barriers to accessing safer supply programs necessitate diversion among people who use drugs — and that the benefits of diversion outweigh the risks.
However, the risks — and harms — of diversion are mounting.
People can quickly develop a tolerance to “safer” opioids and then transition to more dangerous substances. Some B.C. teenagers have said the prescription opioid Dilaudid was a stepping stone to them using fentanyl. In some cases, diversion of these drugs has led to fatal overdoses.
More recently, a Nanaimo man was sentenced to prison for running a highly organized drug operation that trafficked diverted safer supply opioids. He exchanged fentanyl and other illicit drugs for prescription pills obtained from participants in B.C.’s safer supply program.
Recovery
Lester, of Addiction Medicine Canada, believes clinical discretion has gone too far. He says take-home dosing should be eliminated.
“Best practices in addiction medicine assume physicians prescribing is based on sound and thorough research, and ensuring that their prescribing does not cause harm to the broader community, as well as the patient,” he said.
“[Safer supply] for opioids fails in both these regards.”
He also says safer supply should only be offered as a short-term bridge to patients being started on proven treatments like buprenorphine or methadone, which help reduce drug cravings and manage withdrawal symptoms.
B.C.’s witnessed dosing guidelines say prescribers can discuss such treatment options with patients. However, the guidelines remain neutral on whether safer supply is intended as a transitional step toward longer-term treatment.
Regenstreif says this neutrality undermines care.
“[M]ost patients I’ve seen with opioid use disorder don’t want to have [this disorder],” she said. “They would rather be able to set goals and do other things.”
Oversight gaps
Currently, about 3,900 people in B.C. participate in the safer supply program — down from 5,200 in March 2023.
The B.C. government has not provided data on how many have been transitioned to witnessed dosing. Investigative journalist Rob Shaw recently reported that these data do not exist.
“The government … confirmed recently they don’t have any mechanism to track which ‘safe supply’ participants are witnessed and which [are] not,” said Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, who has been a vocal critic of safer supply.
“Without a public report and accountability there can be no confidence.”
The BC Centre on Substance Use, which developed the interim guidelines, says it does not oversee policy decisions or data tracking. It referred Canadian Affairs’ questions to B.C.’s Ministry of Health, which has yet to clarify whether it will track and publish transition data. The ministry did not respond to requests for comment by deadline.
B.C. has also not indicated when or whether it will release final guidelines.
Regenstreif says the flawed guidelines mean many people may be misinformed, discouraged or unsupported when trying to reduce their drug use and recover.
“We’re not listening to people with lived experience of recovery,” she said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
Addictions
More young men want to restrict pornography: survey

From LifeSiteNews
Nearly 64% of American men now believe online pornography should be more difficult to access, with even higher numbers of women saying the same thing.
A new survey has shown that an increasing number of young men want more restrictions on online pornography.
According to a survey by the American Enterprise Institute’s Survey Center on American Life, nearly 7 in 10 (69 percent) of Americans support the idea of making online pornography less accessible. In 2013, 65 percent expressed support for policies restricting internet pornography.
The most substantial increase in the support for restrictive measures on pornography could be observed in young men (age 18-24). In 2013, about half of young men favored restrictions, while 40 percent actively opposed such policies. In 2025, 64 percent of men believe accessing online pornography should be made more difficult.
The largest support for restriction on internet pornography overall could be measured among older men (65+), where 73 percent favored restrictions. An even larger percentage of women in each age group supported making online pornography less accessible. Seventy-two percent of young women (age 18-24) favored restriction, while 87 percent of women 55 years or older expressed support for less accessibility of internet pornography.
Viewing pornography is highly addictive and can lead to serious health problems. Studies have shown that children often have their first encounter with pornography at around 12 years old, with boys having a lower average age of about 10-11, and some encountering online pornography as young as 8. Studies have also shown that viewing pornography regularly rewires humans brains and that children, adolescents, and younger men are especially at risk for becoming addicted to online pornography.
According to Gary Wilson’s landmark book on the matter, “Your Brain on Porn,” pornography addiction frequently leads to problems like destruction of genuine intimate relationships, difficulty forming and maintaining real bonds in relationship, depression, social anxiety, as well as reduction of gray matter, leading to desensitization and diminished pleasure from everyday activities among many others.
-
 Opinion1 day ago
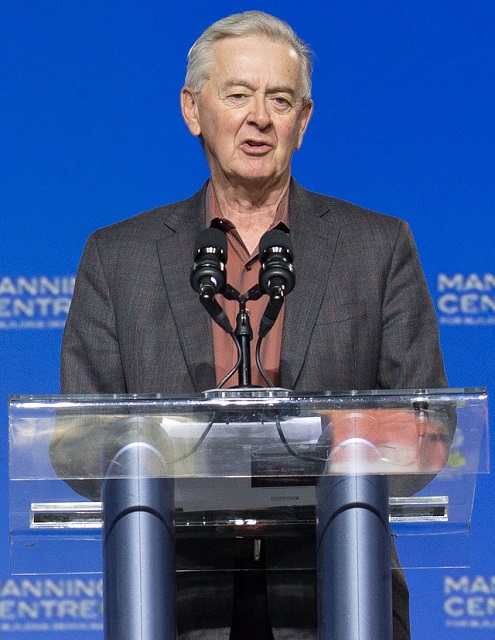
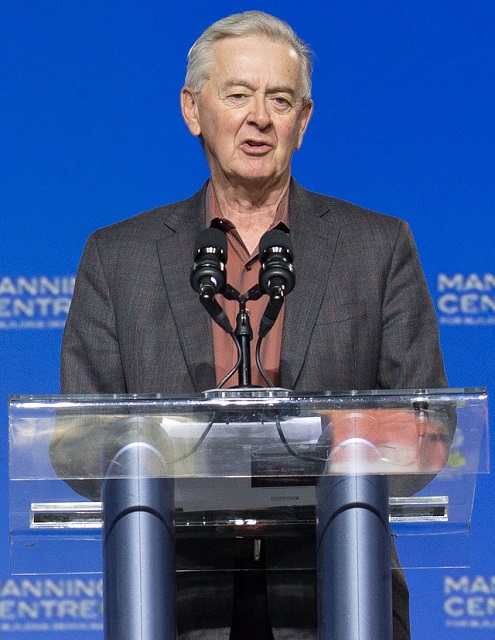
Opinion1 day agoPreston Manning: Three Wise Men from the East, Again
-

 Addictions1 day ago
Addictions1 day agoWhy B.C.’s new witnessed dosing guidelines are built to fail
-

 Business24 hours ago
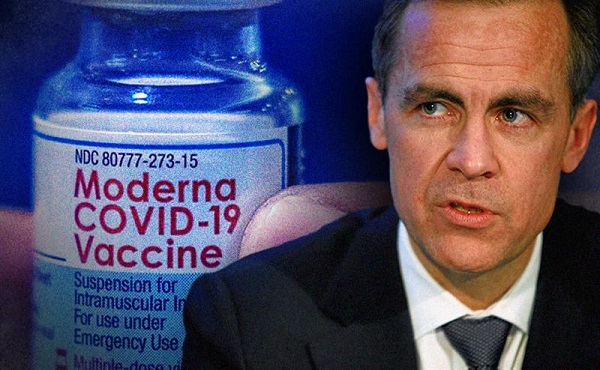
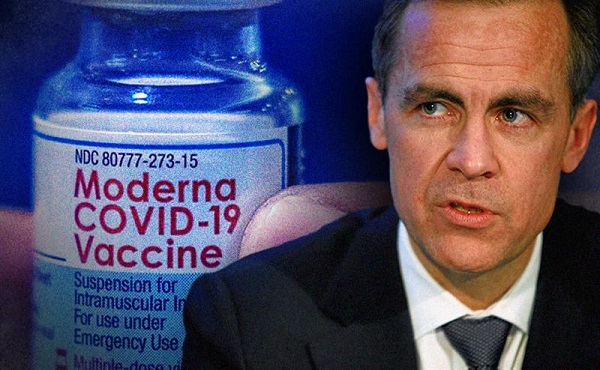
Business24 hours agoMark Carney’s Fiscal Fantasy Will Bankrupt Canada
-

 Business2 days ago
Business2 days agoCarney government should apply lessons from 1990s in spending review
-

 Uncategorized2 days ago
Uncategorized2 days agoCNN’s Shock Climate Polling Data Reinforces Trump’s Energy Agenda
-
 Business1 day ago
Business1 day agoCarney Liberals quietly award Pfizer, Moderna nearly $400 million for new COVID shot contracts
-

 COVID-1924 hours ago
COVID-1924 hours agoTrump DOJ dismisses charges against doctor who issued fake COVID passports
-

 Alberta23 hours ago
Alberta23 hours agoTemporary Alberta grid limit unlikely to dampen data centre investment, analyst says








