Alberta
REPORT: Alberta municipalities hit with $37 million carbon tax tab in 2023

Grande Prairie. Getty Images photo
From the Canadian Energy Centre
Federal cash grab driving costs for local governments, driving up property taxes
New data shows the painful economic impact of the federal carbon tax on municipalities.
Municipalities in Alberta paid out more than $37 million in federal carbon taxes in 2023, based on a recent survey commissioned by Alberta Municipal Affairs, with data provided to the Canadian Energy Centre.
About $760,000 of that came from the City of Grande Prairie. In a statement, Mayor Jackie Clayton said “if the carbon tax were removed, City property taxes could be reduced by 0.6 per cent, providing direct financial relief to residents and businesses in Grande Prairie.”
Conducted in October, the survey asked municipal districts, towns and cities in Alberta to disclose the amount of carbon tax paid out for the heating and electrifying of municipal assets and fuel for fleet vehicles.
With these funds, Alberta municipalities could have hired 7,789 high school students at $15 per hour last year with the amount paid to Ottawa.
The cost on municipalities includes:
Lloydminster: $422,248
Calgary: $1,230,300 (estimate)
Medicine Hat: $876,237
Lethbridge: $1,398,000 (estimate)
Grande Prairie: $757,562
Crowsnest Pass: $71,100
Red Deer: $1,495,945
Bonnyville: $19,484
Hinton: $66,829
Several municipalities also noted substantial indirect costs from the carbon tax, including higher rates from vendors that serve the municipality – like gravel truck drivers and road repair providers – passing increased fuel prices onto local governments.
The rising price for materials and goods like traffic lights, steel, lumber and cement, due to higher transportation costs are also hitting the bottom line for local governments.
The City of Grande Prairie paid out $89 million in goods and services in 2023, and the indirect costs of the carbon tax “have had an inflationary impact on those expenses” in addition to the direct costs of the tax.
In her press conference announcing Alberta’s challenge to the federal carbon tax on Oct. 29, 2024, Premier Danielle Smith addressed the pressures the carbon tax places on municipal bottom lines.
“In 2023 alone, the City of Calgary could have hired an additional 112 police officers or firefighters for the amount they sent to Ottawa for the carbon tax,” she said.
In a statement issued on Oct. 7, 2024, Ontario Conservative MP Ryan Williams, shadow minister for international trade, said this issue is nationwide.
“In Belleville, Ontario, the impact of the carbon tax is particularly notable. The city faces an extra $410,000 annually in costs – a burden that directly translates to an increase of 0.37 per cent on residents’ property tax bills.”
There is no rebate yet provided on retail carbon pricing for towns, cities and counties.
In October, the council in Belleville passed a motion asking the federal government to return in full all carbon taxes paid by municipalities in Canada.
The unaltered reproduction of this content is free of charge with attribution to the Canadian Energy Centre.
Alberta
Alberta takes big step towards shorter wait times and higher quality health care

From the Fraser Institute
On Monday, the Smith government announced that beginning next year it will change the way it funds surgeries in Alberta. This is a big step towards unlocking the ability of Alberta’s health-care system to provide more, better and faster services for the same or possibly fewer dollars.
To understand the significance of this change, you must understand the consequences of the current (and outdated) approach.
Currently, the Alberta government pays a lump sum of money to hospitals each year. Consequently, hospitals perceive patients as a drain on their budgets. From the hospital’s perspective, there’s little financial incentive to serve more patients, operate more efficiently and provide superior quality services.
Consider what would happen if your local grocery store received a giant bag of money each year to feed people. The number of items would quickly decline to whatever was most convenient for the store to provide. (Have a favourite cereal? Too bad.) Store hours would become less convenient for customers, alongside a general decline in overall service. This type of grocery store, like an Alberta hospital, is actually financially better off (that is, it saves money) if you go elsewhere.
The Smith government plans to flip this entire system on its head, to the benefit of patients and taxpayers. Instead of handing out bags of money each year to providers, the new system—known as “activity-based funding”—will pay health-care providers for each patient they treat, based on the patient’s particular condition and important factors that may add complexity or cost to their care.
This turns patients from a drain on budgets into a source of additional revenue. The result, as has been demonstrated in other universal health-care systems worldwide, is more services delivered using existing health-care infrastructure, lower wait times, improved quality of care, improved access to medical technologies, and less waste.
In other words, Albertans will receive far better value from their health-care system, which is currently among the most expensive in the world. And relief can’t come soon enough—for example, last year in Alberta the median wait time for orthopedic surgeries including hip and knee replacements was 66.8 weeks.
The naysayers argue this approach will undermine the province’s universal system and hurt patients. But by allowing a spectrum of providers to compete for the delivery of quality care, Alberta will follow the lead of other more successful universal health-care systems in countries such as Australia, Germany, the Netherlands and Switzerland and create greater accountability for hospitals and other health-care providers. Taxpayers will get a much better picture of what they’re paying for and how much they pay.
Again, Alberta is not exploring an untested policy. Almost every other developed country with universal health care uses some form of “activity-based funding” for hospital and surgical care. And remember, we already spend more on health care than our counterparts in nearly all of these countries yet endure longer wait times and poorer access to services generally, in part because of how we pay for surgical care.
While the devil is always in the details, and while it’s still possible for the Alberta government to get this wrong, Monday’s announcement is a big step in the right direction. A funding model that puts patients first will get Albertans more of the high-quality health care they already pay for in a timelier fashion. And provide to other provinces an example of bold health-care reform.
Alberta
Alberta’s embrace of activity-based funding is great news for patients

 From the Montreal Economic Institute
From the Montreal Economic Institute
Alberta’s move to fund acute care services through activity-based funding follows best practices internationally, points out an MEI researcher following an announcement made by Premier Danielle Smith earlier today.
“For too long, the way hospitals were funded in Alberta incentivized treating fewer patients, contributing to our long wait times,” explains Krystle Wittevrongel, director of research at the MEI. “International experience has shown that, with the proper funding models in place, health systems become more efficient to the benefit of patients.”
Currently, Alberta’s hospitals are financed under a system called “global budgeting.” This involves allocating a pre-set amount of funding to pay for a specific number of services based on previous years’ budgets.
Under the government’s newly proposed funding system, hospitals receive a fixed payment for each treatment delivered.
An Economic Note published by the MEI last year showed that Quebec’s gradual adoption of activity-based funding led to higher productivity and lower costs in the province’s health system.
Notably, the province observed that the per-procedure cost of MRIs fell by four per cent as the number of procedures performed increased by 22 per cent.
In the radiology and oncology sector, it observed productivity increases of 26 per cent while procedure costs decreased by seven per cent.
“Being able to perform more surgeries, at lower costs, and within shorter timelines is exactly what Alberta’s patients need, and Premier Smith understands that,” continued Mrs. Wittevrongel. “Today’s announcement is a good first step, and we look forward to seeing a successful roll-out once appropriate funding levels per procedure are set.”
The governments expects to roll-out this new funding model for select procedures starting in 2026.
* * *
The MEI is an independent public policy think tank with offices in Montreal, Ottawa, and Calgary. Through its publications, media appearances, and advisory services to policymakers, the MEI stimulates public policy debate and reforms based on sound economics and entrepreneurship.
-
 2025 Federal Election2 days ago
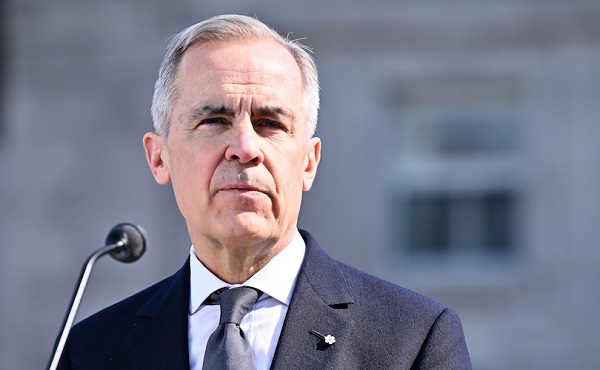
2025 Federal Election2 days agoCommunist China helped boost Mark Carney’s image on social media, election watchdog reports
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoRCMP memo warns of Chinese interference on Canadian university campuses to affect election
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoFifty Shades of Mark Carney
-

 2025 Federal Election21 hours ago
2025 Federal Election21 hours agoResearchers Link China’s Intelligence and Elite Influence Arms to B.C. Government, Liberal Party, and Trudeau-Appointed Senator
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoConservative Party urges investigation into Carney plan to spend $1 billion on heat pumps
-

 MAiD2 days ago
MAiD2 days agoDisability rights panel calls out Canada, US states pushing euthanasia on sick patients
-

 Justice2 days ago
Justice2 days agoCanadian government sued for forcing women to share spaces with ‘transgender’ male prisoners
-

 Alberta2 days ago
Alberta2 days agoAlberta takes big step towards shorter wait times and higher quality health care