Alberta
Pharmacist-led clinics improve access to health care: Lessons from Alberta

News release from the Montreal Economic Institute
In Canada, 35 per cent of avoidable emergency room visits could be handled by pharmacists.
Emulating Alberta’s pharmacist-led clinic model could enhance access to primary care and help avoid unnecessary emergency room visits, according to a new study from the Montreal Economic Institute.
“Pharmacists know medication better than anyone else in our health systems,” explains Krystle Wittevrongel, senior public policy analyst and Alberta project lead at the MEI. “By unlocking their full potential in prescribing and substituting medications, Alberta’s pharmacist-led clinics have helped avoid tens of thousands of unnecessary emergency room visits.”
Pharmacists in Alberta have the largest prescribing authority in the country, including the ability to prescribe schedule one drugs with special training.
Unlike in Ontario and Manitoba, Alberta pharmacists are authorized to substitute prescribed medications, which can help address issues such as adverse reactions caused by interaction with other treatments.
The study explains that this can help reduce pressure on hospitals, as prescription-related issues account for more than 10 per cent of emergency room visits.
Alberta’s first pharmacist-led clinic, in Lethbridge, sees between 14,600 and 21,900 patients per year since opening in 2022.
It is expected that there will be 103 such clinics active in the province by the end of 2024.
The researcher also links the success of the pharmacist-led clinic model in Alberta to pharmacists’ expanded scope of practice in the province.
Among other things, Alberta pharmacists are able to order and interpret lab tests, unlike their counterparts in British Columbia, Ontario, and Newfoundland and Labrador.
A 2019 peer-reviewed study found that pharmacists could handle 35 per cent of avoidable emergency room visits in Canada.
“By enabling pharmacists to play a larger role in its health system, Alberta is redirecting minor cases from emergency rooms to more appropriate facilities,” said Wittevrongel. “Just imagine how much faster things could be if pharmacists could take care of 35 per cent of the unnecessary load placed on Canada’s emergency rooms.”
The MEI study is available here.
* * *
The MEI is an independent public policy think tank with offices in Montreal and Calgary. Through its publications, media appearances, and advisory services to policy-makers, the MEI stimulates public policy debate and reforms based on sound economics and entrepreneurship.
Alberta
Red Deer Justice Centre Grand Opening: Building access to justice for Albertans

The new Red Deer Justice Centre will help Albertans resolve their legal matters faster.
Albertans deserve to have access to a fair, accessible and transparent justice system. Modernizing Alberta’s courthouse infrastructure will help make sure Alberta’s justice system runs efficiently and meets the needs of the province’s growing population.
Alberta’s government has invested $191 million to build the new Red Deer Justice Centre, increasing the number of courtrooms from eight to 12, allowing more cases to be heard at one time.
“Modern, accessible courthouses and streamlined services not only strengthen our justice
system – they build safer, stronger communities across the province. Investing in the new Red Deer Justice Centre is vital to helping our justice system operate more efficiently, and will give people in Red Deer and across central Alberta better access to justice.”

Government of Alberta and Judiciary representatives with special guests at the Red Deer Justice Centre plaque unveiling event April 22, 2025.
On March 3, all court services in Red Deer began operating out of the new justice centre. The new justice centre has 12 courtrooms fully built and equipped with video-conference equipment to allow witnesses to attend remotely if they cannot travel, and vulnerable witnesses to testify from outside the courtroom.
The new justice centre also has spaces for people taking alternative approaches to the traditional courtroom trial process, with the three new suites for judicial dispute resolution services, a specific suite for other dispute resolution services, such as family mediation and civil mediation, and a new Indigenous courtroom with dedicated venting for smudging purposes.
“We are very excited about this new courthouse for central Alberta. Investing in the places where people seek justice shows respect for the rights of all Albertans. The Red Deer Justice Centre fills a significant infrastructure need for this rapidly growing part of the province. It is also an important symbol of the rule of law, meaning that none of us are above the law, and there is an independent judiciary to decide disputes. This is essential for a healthy functioning democracy.”
“Public safety and access to justice go hand in hand. With this investment in the new Red Deer Justice Centre, Alberta’s government is ensuring that communities are safer, legal matters are resolved more efficiently and all Albertans get the support they need.”
“This state-of-the-art facility will serve the people of Red Deer and surrounding communities for generations. Our team at Infrastructure is incredibly proud of the work done to plan, design and build this project. I want to thank everyone, at all levels, who helped make this project a reality.”
Budget 2025 is meeting the challenge faced by Alberta with continued investments in education and health, lower taxes for families and a focus on the economy.

Quick facts
- The new Red Deer Justice Centre is 312,000 sq ft (29,000 m2). (The old courthouse is 98,780 sq ft (9,177 m2)).
- The approved project funding for the Red Deer Justice Centre is about $191 million.
Alberta
CPP another example of Albertans’ outsized contribution to Canada

From the Fraser Institute
By Tegan Hill
Amid the economic uncertainty fuelled by Trump’s trade war, its perhaps more important than ever to understand Alberta’s crucial role in the federation and its outsized contribution to programs such as the Canada Pension Plan (CPP).
From 1981 to 2022, Albertan’s net contribution to the CPP—meaning the amount Albertans paid into the program over and above what retirees in Alberta received in CPP payments—was $53.6 billion. In 2022 (the latest year of available data), Albertans’ net contribution to the CPP was $3.0 billion.
During that same period (1981 to 2022), British Columbia was the only other province where residents paid more into the CPP than retirees received in benefits—and Alberta’s contribution was six times greater than B.C.’s contribution. Put differently, residents in seven out of the nine provinces that participate in the CPP (Quebec has its own plan) receive more back in benefits than they contribute to the program.
Albertans pay an outsized contribution to federal and national programs, including the CPP because of the province’s relatively high rates of employment, higher average incomes and younger population (i.e. more workers pay into the CPP and less retirees take from it).
Put simply, Albertan workers have been helping fund the retirement of Canadians from coast to coast for decades, and without Alberta, the CPP would look much different.
How different?
If Alberta withdrew from the CPP and established its own standalone provincial pension plan, Alberta workers would receive the same retirement benefits but at a lower cost (i.e. lower CPP contribution rate deducted from our paycheques) than other Canadians, while the contribution rate—essentially the CPP tax rate—to fund the program would likely need to increase for the rest of the country to maintain the same benefits.
And given current demographic projections, immigration patterns and Alberta’s long history of leading the provinces in economic growth, Albertan workers will likely continue to pay more into the CPP than Albertan retirees get back from it.
Therefore, considering Alberta’s crucial role in national programs, the next federal government—whoever that may be—should undo and prevent policies that negatively impact the province and Albertans ability to contribute to Canada. Think of Bill C-69 (which imposes complex, uncertain and onerous review requirements on major energy projects), Bill C-48 (which bans large oil tankers off B.C.’s northern coast and limits access to Asian markets), an arbitrary cap on oil and gas emissions, numerous other “net-zero” targets, and so on.
Canada faces serious economic challenges, including a trade war with the United States. In times like this, it’s important to remember Alberta’s crucial role in the federation and the outsized contributions of Alberta workers to the wellbeing of Canadians across the country.
-
 2025 Federal Election2 days ago
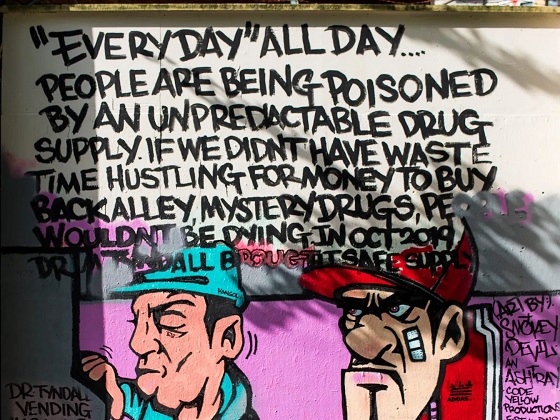
2025 Federal Election2 days agoStudy links B.C.’s drug policies to more overdoses, but researchers urge caution
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCarney’s Hidden Climate Finance Agenda
-

 Business2 days ago
Business2 days agoIs Government Inflation Reporting Accurate?
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoWhen it comes to pipelines, Carney’s words flow both ways
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPolls say Canadians will give Trump what he wants, a Carney victory.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoThe Anhui Convergence: Chinese United Front Network Surfaces in Australian and Canadian Elections
-

 2025 Federal Election23 hours ago
2025 Federal Election23 hours agoPoilievre Campaigning To Build A Canadian Economic Fortress
-

 Automotive23 hours ago
Automotive23 hours agoCanadians’ Interest in Buying an EV Falls for Third Year in a Row