Opinion
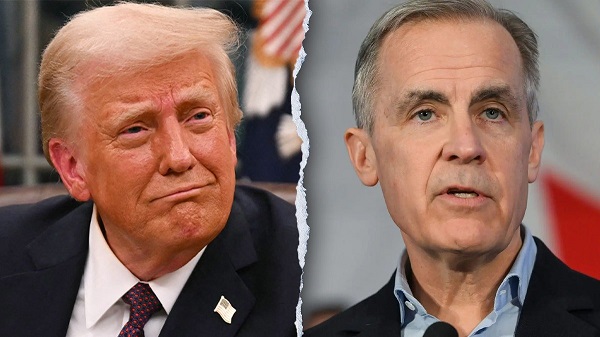
Federal Government appears led by Mr. Dressup, but acts like “The Partridge Family” when we need the “A-Team”.

For quite sometime I was smugly believing that in Federal politics after 10 years of Angry Bird running the country we turned to Mr. Dressup to give it a go. The latest trip to India, with extreme costume changes could support that line of reasoning.
But another show kept creeping into my consciousness; “The Partridge Family”. A show about a family having misadventure after misadventure before ending up on stage.
The India fiasco involved a family, children, costume changes, dancing on stage. Misadventure after misadventure sure sounds like the Partridge Family to me.
Every episode had a theme, had a misadventure just like this government of ours. You would think that the business of government was managed by the fictional manager Rueben Kincaid and choreographed by the fictional brother Danny Partridge.
The show ran from 1970-1974, I believe, which is the same as a single term in government. So will we reprogram after 4 years and go for another show, Gilligan’s Island perhaps? Perhaps with island theme in mind, let us go with Fantasy Island and then we might see “da plane” our military desperately needs.
I would really hope that this government could change channels and be more like; “The National”. We might end up with Mr. Rogers as Prime Minister and that would not be the “A-Team” we hoping for.
2025 Federal Election
MEI-Ipsos poll: 56 per cent of Canadians support increasing access to non-governmental healthcare providers

-
Most believe private providers can deliver services faster than government-run hospitals
-
77 per cent of Canadians say their provincial healthcare system is too bureaucratic
Canadians are increasingly in favour of breaking the government monopoly over health care by opening the door to independent providers and cross-border treatments, an MEI-Ipsos poll has revealed.
“Canadians from coast to coast are signalling they want to see more involvement from independent health providers in our health system,” explains Emmanuelle B. Faubert, economist at the MEI. “They understand that universal access doesn’t mean government-run, and that consistent failures to deliver timely care in government hospitals are a feature of the current system.”
Support for independent health care is on the rise, with 56 per cent of respondents in favour of allowing patients to access services provided by independent health entrepreneurs. Only 25 per cent oppose this.
In Quebec, support is especially strong, with 68 per cent endorsing this change.
Favourable views of accessing care through a mixed system are widespread, with three quarters of respondents stating that private entrepreneurs can deliver healthcare services faster than hospitals managed by the government. This is up four percentage points from last year.
Countries like Sweden and France combine universal coverage with independent providers and deliver faster, more accessible care. When informed about how these health systems run, nearly two in three Canadians favour adopting such models.
The poll also finds that 73 per cent of Canadians support allowing patients to receive treatment abroad with provincial coverage, which could help reduce long wait times at home.
Common in the European Union, this “cross-border directive” enabled 450,000 patients to access elective surgeries in 2022, with costs reimbursed as if they had been treated in their home country.
There’s a growing consensus that provincial healthcare systems are overly bureaucratic, with the strongest agreement in Alberta, B.C., and Quebec. The proportion of Canadians holding this view has risen by 16 percentage points since 2020.
Nor do Canadians see more spending as being a solution: over half say the current pace of healthcare spending in their province is unsustainable.
“Governments shouldn’t keep doubling down on what isn’t working. Instead, they should look at what works abroad,” says Ms. Faubert. “Canadians have made it clear they want to shift gears; now it’s up to policymakers to show they’re listening.”
A sample of 1,164 Canadians aged 18 and older was polled between March 24th and March 28th, 2025. The margin of error is ±3.3 percentage points, 19 times out of 20.
The results of the MEI-Ipsos poll are available here.
* * *
The MEI is an independent public policy think tank with offices in Montreal, Ottawa, and Calgary. Through its publications, media appearances, and advisory services to policymakers, the MEI stimulates public policy debate and reforms based on sound economics and entrepreneurship.
Autism
Autism Rates Reach Unprecedented Highs: 1 in 12 Boys at Age 4 in California, 1 in 31 Nationally

 Popular Rationalism
Popular Rationalism
 James Lyons-Weiler
James Lyons-Weiler
The U.S. Centers for Disease Control and Prevention (CDC) has released its 2025 report from the Autism and Developmental Disabilities Monitoring (ADDM) Network, and the findings are alarming: autism spectrum disorder (ASD) now affects 1 in 31 American 8-year-olds—the highest rate ever recorded.
For boys, the numbers are even more staggering: 1 in 20 nationwide, and 1 in 12.5 in California. The report, which tracks children born in 2014, reveals a crisis growing in severity and complexity, yet broadly unacknowledged in the national discourse.
Autism has become a public health crisis of urgent concern,” the report states plainly. And yet, government agencies have offered no new national action plan, and media coverage remains anemic.
Rapidly Accelerating Trends
In just two years, autism prevalence among 8-year-olds rose 17%, from 1 in 36 to 1 in 31. This is not an anomaly. Since the CDC began tracking autism in children born in 1992, prevalence has increased nearly fivefold, defying theories that attribute the rise solely to broader diagnostic criteria or increased awareness.
The Impact of SB277 on Autism Prevalence in California
In 2015, California enacted Senate Bill 277 (SB277), which went into effect on July 1, 2016. This legislation eliminated the state’s personal belief exemption (PBE) for childhood vaccinations, making it one of only three U.S. states at the time—alongside Mississippi and West Virginia—to require full compliance with the CDC-recommended vaccine schedule for school entry, except in cases of formally approved medical exemption.
While the primary intent of SB277 was to increase vaccination rates and try to reduce outbreaks of communicable diseases like measles, its implementation has coincided with a continued—and arguably accelerated—rise in autism spectrum disorder (ASD) diagnoses in the state. Data drawn from the California Department of Developmental Services (CDDS) and CDC’s Autism and Developmental Disabilities Monitoring (ADDM) Network offer a timeline of prevalence rates before and after the law’s enactment:
Between 2014 and 2017, ASD prevalence among young children in California increased from 0.86% to 1.18%—a 37.2% increase in just three years. By 2020, according to CDC ADDM surveillance, 4.5% of 8-year-olds in California had an autism diagnosis—the highest prevalence among all U.S. monitoring sites.
Percent Increase Post-SB277 (2016 to 2020):
From 1.08% (2016) to 4.5% (2020) = 316.7% increase
This dramatic rise cannot be definitively attributed to SB277 alone, but its temporal proximity to the policy change—which effectively compelled full vaccine schedule compliance across all demographic groups—raises serious questions. Notably, this increase occurred within California’s already robust autism tracking infrastructure (CDDS), known for conservative case identification that focuses on children with moderate to severe impairment requiring lifelong services.
While correlation does not imply causation, the magnitude and timing of California’s autism surge post-SB277 should compel further independent investigation, particularly given that:
- SB277 removed opt-out options for thousands of previously unvaccinated or selectively vaccinated children;
- The increase is most visible in 4-year-old cohorts tracked soon after the law took effect;
- California’s autism rates now exceed 1 in 12 for boys.
In light of these findings, California may now serve not only as a terrible national model for vaccine compliance—but also as a bellwether for unintended consequences of compulsory public health policy.
Alarming Trends in IQ
Contrary to such assumption of ASD leading to giftedness, the ADDM data also show that the proportion of children with higher IQs is actually decreasing, while the share of children with intellectual disability (IQ ≤ 70) has risen. Nearly 2 out of 3 children (64%) diagnosed with autism in this cohort fall below the IQ 85 threshold, indicating moderate to severe impairment.
These are hard realities that many will find unacceptable. Still, nationally, nearly 40% (39.6%) of 8-year-olds with ASD had IQ ≤ 70. Another 24.2% had borderline IQ (71–85). 36.1% had IQ > 85.
Since autism has a motor neuron impairment, demonstrated IQ may be an inexact measure of actual intelligence, as Spellers The Movie has taught the world.
From a clinical viewpoint, the ADDM report’s data quietly demolish the idea that autism incidence increases are driven by mild or high-functioning cases. Since the early 2000s, the proportion of cases with average or high IQ has dropped, while those with intellectual disability have surged. This trend—now reaching nearly 64%—indicates that autism’s rise is not a matter of greater sensitivity in diagnosis. Rather, it appears we are witnessing a real increase in biologically significant, disabling neurodevelopmental injury.
Reversal of Historic Ethnodemographic Trends
The report presents data on racial disparity that now represents a reversal:
Asian/Pacific Islander (3.75%), Black (3.63%), Hispanic (3.58%), and Multiracial (3.27%) 8-year-olds are now more likely to be identified with autism than White children (2.77%)
This is a complete reversal of pre-2018 trends, where White children had the highest identification rates. Children from low-income neighborhoods had higher prevalence of ASD than those from high-income areas in several states, e.g., Utah and Wisconsin
The California Signal: A Harbinger of What’s to Come?
San Diego, California, stands out as a sentinel site—and a warning. According to Supplementary Table 8 of the report, 8.87% of 4-year-old boys in California are diagnosed with autism. Further breakdown shows even more troubling disparities:
- Black boys: ~12%
- Hispanic boys: ~10.5%
- Asian boys: ~9%
- White boys: ~5.3%
These numbers imply that 1 in 8 to 1 in 10 young boys of color in California may carry an autism diagnosis by the time they reach second grade.
Are Environmental Triggers Driving This?
One overlooked possibility is that cumulative exposures—including the full CDC childhood vaccine schedule, lockdown-era developmental disruption, and coexisting toxicants—may act in concert to dysregulate immune and neurological development. California’s 2016 vaccine mandate removed all non-medical exemptions, making full compliance unavoidable for most working families. This timing intersects directly with birth years showing the steepest autism rises. If these policy changes are contributing, even partly, to this epidemiological shift, they demand urgent investigation—not blind defense.
The demographic disparities further reinforce the environmental hypothesis. Among 4-year-olds, autism rates among children of color now exceed those of White children by 40–90%, depending on the group and region.
Public Health Policies Under Scrutiny
Importantly, California’s strict mandate—which bars children from school or daycare without full vaccination—creates a uniquely high-exposure environment for children whose families cannot afford alternatives. These children are also more likely to be Black or Hispanic, compounding the already sharp disparities now seen in ASD prevalence. In San Diego’s 2018 birth cohort, over 1 in 10 Black and Hispanic boys have an autism diagnosis at age four. The notion that this simply reflects “better identification” strains all credibility.
Additionally, pandemic-era lockdowns, prolonged school closures, and extended masking requirements in California may have played a compounding role in disrupting normal developmental pathways for toddlers and young children during formative years.
The Cost of Inaction
The fiscal and societal burden of autism is already astronomical. A 2020 economic model projected U.S. autism-related costs could exceed $5.5 trillion per year by 2060 if trends continue unmitigated. That estimate did not anticipate the rapid acceleration seen in this latest data.
Your tax dollars have funded years of futile autism genetics research that has not led to any prevention, mitation or treatment, and any given individual genes from genome-wide association studies (GWAS) still explain only a sliver of ASD heritability. Meanwhile, evidence continues to build around plausible environmental and iatrogenic mechanisms—oxidative stress, mitochondrial dysfunction, and aluminum adjuvants, among others—without serious investment in confirming or ruling them out. If the CDC were tracking causation with the same rigor it tracks prevalence, we might already have answers.
A Turning Point?
Public health leadership now faces a choice: double down on statistical obfuscation, or finally confront the rising tide of childhood neurological injury. The tools exist—retrospective cohort comparisons, machine learning to detect risk patterns, causal inference modeling of environmental exposures, and most critically, honest, open-ended research. The CDC and NIH must stop chasing only genetic ghosts and start investigating the real, tangible environmental shifts that mirror this crisis in time.
For decades, the CDC, NIH, and IOM have promoted the idea that the rise in autism is primarily diagnostic, while excluding or downplaying environmental and iatrogenic hypotheses. But the current data—showing accelerating prevalence, worsening severity, and growing racial disparities—make this position untenable. It is now clear that narrative closure, not causal closure, has been guiding public messaging. The refusal to explore vaccine adjuvants, prenatal toxic exposures, chronic immune activation, and regulatory policy failures reflects a broken system more committed to preserving public confidence than discovering the truth.
In a striking statement during an April 2025 Cabinet meeting, Secretary of Health and Human Services Robert F. Kennedy Jr. declared,
“By September, we will know what has caused the autism epidemic and we’ll be able to eliminate those exposures.”
The promise represents a historic shift in federal tone—marking the first time in decades that a sitting health official has committed to openly investigating all plausible causes of autism, including environmental and iatrogenic exposures.
Popular Rationalism is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoNo Matter The Winner – My Canada Is Gone
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCSIS Warned Beijing Would Brand Conservatives as Trumpian. Now Carney’s Campaign Is Doing It.
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoInside Buttongate: How the Liberal Swamp Tried to Smear the Conservative Movement — and Got Exposed
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoASK YOURSELF! – Can Canada Endure, or Afford the Economic Stagnation of Carney’s Costly Climate Vision?
-

 Alberta2 days ago
Alberta2 days agoMade in Alberta! Province makes it easier to support local products with Buy Local program
-

 Alberta2 days ago
Alberta2 days agoProvince to expand services provided by Alberta Sheriffs: New policing option for municipalities
-

 International2 days ago
International2 days agoTulsi Gabbard tells Trump she has ‘evidence’ voting machines are ‘vulnerable to hackers’
-
 COVID-191 day ago
COVID-191 day agoCOVID virus, vaccines are driving explosion in cancer, billionaire scientist tells Tucker Carlson