Addictions
Drug-related deaths fall in Alberta after province adopts recovery-based program over ‘safe supply’

From LifeSiteNews
Data revealed that deaths by drugs in Alberta dropped to 72 in May after reaching a peak of 185 in March 2023.
Deaths related to opioid and other drug overdoses in the Canadian province of Alberta have fallen to their lowest levels in years after the Conservative government began to focus on helping addicts via a recovery-based approach instead of the Liberal-minded, so-called “safe-supply” method.
According to data released by the United Conservative Party (UCP) government via its “Alberta substance use surveillance system,” which was updated in August, there was a 55 percent decrease in opioid-related deaths in May 2024 compared with May 2023.
The data revealed that deaths by deadly drugs fell to 72 in May, which was the lowest reported since March 2020 when 71 deaths were reported.
At their peak, opioid-related deaths spiked at 185 in March 2023. Since that time, deaths have been on the decline.
Dan Williams, who serves as Alberta’s mental health and addictions minister, noted to the media in a recent statement that it is his view that a recovery-based approach to dealing and helping addicts is the right way to go as opposed to giving out free drugs, which is done in British Columbia.
He said that, in his view, he is “cautiously optimistic” that the declining deaths are due to focusing on a recovery-based model when dealing with the rampant abuse of illicit drugs.
Williams said that the UCP government believes that for people suffering from “the disease of addiction, recovery is possible.”
“We are turning words into action and giving people an opportunity to pursue recovery,” he said.
The Alberta government’s recovery-based approach specifically focuses on prevention and the treatment of addicts as well as a long-term recovery support model.
The federal government of Prime Minister Justin Trudeau claims their “safer supply” program is good because it is “providing prescribed medications as a safer alternative to the toxic illegal drug supply to people who are at high risk of overdose.”
However, studies have shown that these programs often lead to an excess of deaths from overdose in areas where they are allowed.
In British Columbia and Ontario, the so-called “safer supply” model has been in use and promoted by current and former governments. However, Ontario Premier Doug Ford, as reported by LifeSiteNews recently, said he wants to end safer “supply” in his province. He said Trudeau’s continued push for lax drug policies has effectively turned the federal government into “the biggest drug dealer in the entire country.”
Williams observed that the “safer supply” model is not something Alberta will be doing, and instead will focus on “expanding access to the treatment and recovery services we know save lives.”
While drug overdose deaths have dipped slightly in British Columbia and Ontario, they are still extremely high, with 185 deaths alone in June just in British Columbia.
The NDP provincial government of British Columbia and the Trudeau feds are proponents of legalizing some hard drugs. Alberta is opposed to such a policy.
While many of the Trudeau government’s lax drug policies continue, it has been forced to backpedal on some of its most extreme actions.
After his federal government allowed the province of British Columbia to decriminalize the possession of hard drugs, including heroin, cocaine, fentanyl, meth and MDMA beginning on January 1, 2023, reports of overdoses and chaos began skyrocketing, leading the province to request that Trudeau re-criminalize drugs in public spaces.
A week later, the Trudeau government relented and accepted British Columbia’s request.
Addictions
Addiction experts demand witnessed dosing guidelines after pharmacy scam exposed

By Alexandra Keeler
The move follows explosive revelations that more than 60 B.C. pharmacies were allegedly participating in a scheme to overbill the government under its safer supply program. The scheme involved pharmacies incentivizing clients to fill prescriptions they did not require by offering them cash or rewards. Some of those clients then sold the drugs on the black market.
An addiction medicine advocacy group is urging B.C. to promptly issue new guidelines for witnessed dosing of drugs dispensed under the province’s controversial safer supply program.
In a March 24 letter to B.C.’s health minister, Addiction Medicine Canada criticized the BC Centre on Substance Use for dragging its feet on delivering the guidelines and downplaying the harms of prescription opioids.
The centre, a government-funded research hub, was tasked by the B.C. government with developing the guidelines after B.C. pledged in February to return to witnessed dosing. The government’s promise followed revelations that many B.C. pharmacies were exploiting rules permitting patients to take safer supply opioids home with them, leading to abuse of the program.
“I think this is just a delay,” said Dr. Jenny Melamed, a Surrey-based family physician and addiction specialist who signed the Addiction Medicine Canada letter. But she urged the centre to act promptly to release new guidelines.
“We’re doing harm and we cannot just leave people where they are.”
Addiction Medicine Canada’s letter also includes recommendations for moving clients off addictive opioids altogether.
“We should go back to evidence-based medicine, where we have medications that work for people in addiction,” said Melamed.
‘Best for patients’
On Feb. 19, the B.C. government said it would return to a witnessed dosing model. This model — which had been in place prior to the pandemic — will require safer supply participants to take prescribed opioids under the supervision of health-care professionals.
The move follows explosive revelations that more than 60 B.C. pharmacies were allegedly participating in a scheme to overbill the government under its safer supply program. The scheme involved pharmacies incentivizing clients to fill prescriptions they did not require by offering them cash or rewards. Some of those clients then sold the drugs on the black market.
In its Feb. 19 announcement, the province said new participants in the safer supply program would immediately be subject to the witnessed dosing requirement. For existing clients of the program, new guidelines would be forthcoming.
“The Ministry will work with the BC Centre on Substance Use to rapidly develop clinical guidelines to support prescribers that also takes into account what’s best for patients and their safety,” Kendra Wong, a spokesperson for B.C.’s health ministry, told Canadian Affairs in an emailed statement on Feb. 27.
More than a month later, addiction specialists are still waiting.
According to Addiction Medicine Canada’s letter, the BC Centre on Substance Use posed “fundamental questions” to the B.C. government, potentially causing the delay.
“We’re stuck in a place where the government publicly has said it’s told BCCSU to make guidance, and BCCSU has said it’s waiting for government to tell them what to do,” Melamed told Canadian Affairs.
This lag has frustrated addiction specialists, who argue the lack of clear guidance is impeding the transition to witnessed dosing and jeopardizing patient care. They warn that permitting take-home drugs leads to more diversion onto the streets, putting individuals at greater risk.
“Diversion of prescribed alternatives expands the number of people using opioids, and dying from hydromorphone and fentanyl use,” reads the letter, which was also co-signed by Dr. Robert Cooper and Dr. Michael Lester. The doctors are founding board members of Addiction Medicine Canada, a nonprofit that advises on addiction medicine and advocates for research-based treatment options.
“We have had people come in [to our clinic] and say they’ve accessed hydromorphone on the street and now they would like us to continue [prescribing] it,” Melamed told Canadian Affairs.
A spokesperson for the BC Centre on Substance Use declined to comment, referring Canadian Affairs to the Ministry of Health. The ministry was unable to provide comment by the publication deadline.
Big challenges
Under the witnessed dosing model, doctors, nurses and pharmacists will oversee consumption of opioids such as hydromorphone, methadone and morphine in clinics or pharmacies.
The shift back to witnessed dosing will place significant demands on pharmacists and patients. In April 2024, an estimated 4,400 people participated in B.C.’s safer supply program.
Chris Chiew, vice president of pharmacy and health-care innovation at the pharmacy chain London Drugs, told Canadian Affairs that the chain’s pharmacists will supervise consumption in semi-private booths.
Nathan Wong, a B.C.-based pharmacist who left the profession in 2024, fears witnessed dosing will overwhelm already overburdened pharmacists, creating new barriers to care.
“One of the biggest challenges of the retail pharmacy model is that there is a tension between making commercial profit, and being able to spend the necessary time with the patient to do a good and thorough job,” he said.
“Pharmacists often feel rushed to check prescriptions, and may not have the time to perform detailed patient counselling.”
Others say the return to witnessed dosing could create serious challenges for individuals who do not live close to health-care providers.
Shelley Singer, a resident of Cowichan Bay, B.C., on Vancouver Island, says it was difficult to make multiple, daily visits to a pharmacy each day when her daughter was placed on witnessed dosing years ago.
“It was ridiculous,” said Singer, whose local pharmacy is a 15-minute drive from her home. As a retiree, she was able to drive her daughter to the pharmacy twice a day for her doses. But she worries about patients who do not have that kind of support.
“I don’t believe witnessed supply is the way to go,” said Singer, who credits safer supply with saving her daughter’s life.
Melamed notes that not all safer supply medications require witnessed dosing.
“Methadone is under witness dosing because you start low and go slow, and then it’s based on a contingency management program,” she said. “When the urine shows evidence of no other drug, when the person is stable, [they can] take it at home.”
She also noted that Suboxone, a daily medication that prevents opioid highs, reduces cravings and alleviates withdrawal, does not require strict supervision.
Kendra Wong, of the B.C. health ministry, told Canadian Affairs that long-acting medications such as methadone and buprenorphine could be reintroduced to help reduce the strain on health-care professionals and patients.
“There are medications available through the [safer supply] program that have to be taken less often than others — some as far apart as every two to three days,” said Wong.
“Clinicians may choose to transition patients to those medications so that they have to come in less regularly.”
Such an approach would align with Addiction Medicine Canada’s recommendations to the ministry.
The group says it supports supervised dosing of hydromorphone as a short-term solution to prevent diversion. But Melamed said the long-term goal of any addiction treatment program should be to reduce users’ reliance on opioids.
The group recommends combining safer supply hydromorphone with opioid agonist therapies. These therapies use controlled medications to reduce withdrawal symptoms, cravings and some of the risks associated with addiction.
They also recommend limiting unsupervised hydromorphone to a maximum of five 8 mg tablets a day — down from the 30 tablets currently permitted with take-home supplies. And they recommend that doses be tapered over time.
“This protocol is being used with success by clinicians in B.C. and elsewhere,” the letter says.
“Please ensure that the administrative delay of the implementation of your new policy is not used to continue to harm the public.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
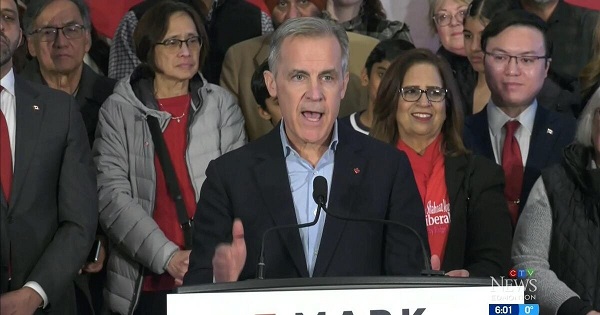
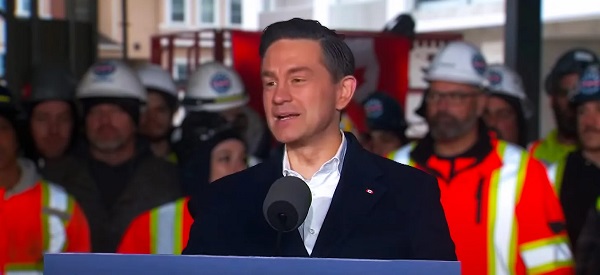
2025 Federal Election
Poilievre to invest in recovery, cut off federal funding for opioids and defund drug dens

From Conservative Party Communications
Poilievre will Make Recovery a Reality for 50,000 Canadians
Conservative Leader Pierre Poilievre pledged he will bring the hope that our vulnerable Canadians need by expanding drug recovery programs, creating 50,000 new opportunities for Canadians seeking freedom from addiction. At the same time, he will stop federal funding for opioids, defund federal drug dens, and ensure that any remaining sites do not operate within 500 meters of schools, daycares, playgrounds, parks and seniors’ homes, and comply with strict new oversight rules that focus on pathways to treatment.
More than 50,000 people have lost their lives to fentanyl since 2015—more Canadians than died in the Second World War. Poilievre pledged to open a path to recovery while cracking down on the radical Liberal experiment with free access to illegal drugs that has made the crisis worse and brought disorder to local communities.
Specifically, Poilievre will:
- Fund treatment for 50,000 Canadians. A new Conservative government will fund treatment for 50,000 Canadians in treatment centres with a proven record of success at getting people off drugs. This includes successful models like the Bruce Oake Recovery Centre, which helps people recover and reunite with their families, communities, and culture. To ensure the best outcomes, funding will follow results. Where spaces in good treatment programs exist, we will use them, and where they need to expand, these funds will allow that.
- Ban drug dens from being located within 500 metres of schools, daycares, playgrounds, parks, and seniors’ homes and impose strict new oversight rules. Poilievre also pledged to crack down on the Liberals’ reckless experiments with free access to illegal drugs that allow provinces to operate drug sites with no oversight, while pausing any new federal exemptions until evidence justifies they support recovery. Existing federal sites will be required to operate away from residential communities and places where families and children frequent and will now also have to focus on connecting users with treatment, meet stricter regulatory standards or be shut down. He will also end the exemption for fly-by-night provincially-regulated sites.
“After the Lost Liberal Decade, Canada’s addiction crisis has spiralled out of control,” said Poilievre. “Families have been torn apart while children have to witness open drug use and walk through dangerous encampments to get to school. Canadians deserve better than the endless Liberal cycle of crime, despair, and death.”
Since the Liberals were first elected in 2015, our once-safe communities have become sordid and disordered, while more and more Canadians have been lost to the dangerous drugs the Liberals have flooded into our streets. In British Columbia, where the Liberals decriminalized dangerous drugs like fentanyl and meth, drug overdose deaths increased by 200 percent.
The Liberals also pursued a radical experiment of taxpayer-funded hard drugs, which are often diverted and resold to children and other vulnerable Canadians. The Vancouver Police Department has said that roughly half of all hydromorphone seizures were diverted from this hard drugs program, while the Waterloo Regional Police Service and Niagara Regional Police Service said that hydromorphone seizures had exploded by 1,090% and 1,577%, respectively.
Despite the death and despair that is now common on our streets, bizarrely Mark Carney told a room of Liberal supporters that 50,000 fentanyl deaths in Canada is not “a crisis.” He also hand-picked a Liberal candidate who said the Liberals “would be smart to lean into drug decriminalization” and another who said “legalizing all drugs would be good for Canada.”
Carney’s star candidate Gregor Robertson, an early advocate of decriminalization and so-called safe supply, wanted drug dens imposed on communities without any consultation or public safety considerations. During his disastrous tenure as Vancouver Mayor, overdoses increased by 600%.
Alberta has pioneered an approach that offers real hope by adopting a recovery-focused model of care, leading to a nearly 40 percent reduction in drug-poisoning deaths since 2023—three times the decrease seen in British Columbia. However, we must also end the Liberal drug policies that have worsened the crisis and harmed countless lives and families.
To fund this policy, a Conservative government will stop federal funding for opioids, defund federal drug dens, and sue the opioid manufacturers and consulting companies who created this crisis in the first place.
“Canadians deserve better than the Liberal cycle of crime, despair, and death,” said Poilievre. “We will treat addiction with compassion and accountability—not with more taxpayer-funded poison. We will turn hurt into hope by shutting down drug dens, restoring order in our communities, funding real recovery, and bringing our loved ones home drug-free.”
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoOttawa Confirms China interfering with 2025 federal election: Beijing Seeks to Block Joe Tay’s Election
-

 International2 days ago
International2 days agoJD Vance was one of the last people to meet Pope Francis
-

 COVID-191 day ago
COVID-191 day agoNearly Half of “COVID-19 Deaths” Were Not Due to COVID-19 – Scientific Reports Journal
-
 2025 Federal Election1 day ago
2025 Federal Election1 day agoHow Canada’s Mainstream Media Lost the Public Trust
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoBREAKING: THE FEDERAL BRIEF THAT SHOULD SINK CARNEY
-
 2025 Federal Election1 day ago
2025 Federal Election1 day agoReal Homes vs. Modular Shoeboxes: The Housing Battle Between Poilievre and Carney
-

 International14 hours ago
International14 hours agoNew York Times publishes chilling new justification for assisted suicide
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoPOLL: Canadians want spending cuts







