Health
Canada remains poor performer among countries with universal health care

From the Fraser Institute
By Mackenzie Moir and Bacchus Barua
Canada reported far fewer physicians (ranking 28th of 30) and hospital beds (23rd of 29) per 1,000 people in 2021. And ranked low for the availability of MRI machines (25th of 29) and CT scanners (26thof 30) per million people in 2019
Earlier this year, the Trudeau government announced it will increase health-care spending to provinces and territories by $196.1 billion over the next decade. But patients hoping for improved access will likely be disappointed. In reality, Canada’s health-care system already ranks as one of the most expensive systems in the world, but only has mediocre results to show for it. In other words, the problem isn’t the amount of money we spend, it’s the poor value we get for our health-care dollars.
A new study compared the spending and performance of Canada’s system with 29 other universal health-care systems worldwide. According to the study (after adjusting for population age in each country), Canada was the highest spender on health care as a share of the economy (at 12.6 per cent) and ninth-highest on a per person basis in 2021, the latest year of available data.
And yet, compared to other universal countries, Canada reported far fewer physicians (ranking 28th of 30) and hospital beds (23rd of 29) per 1,000 people in 2021. And ranked low for the availability of MRI machines (25th of 29) and CT scanners (26thof 30) per million people in 2019 (the latest year of available data).
Unsurprisingly, scarce health-care resources are accompanied by long wait times. Using data collected in 2020 by the Commonwealth Fund, the study found that only 38 per cent of Canadians reported waiting less than four weeks for a specialist appointment—a much smaller percentage than countries such as Switzerland (68 per cent) and Germany (67 per cent). On this indicator, Canada ranked 10th out of 10 countries. Canada also ranked dead last (10th) on timely access to elective surgery—with 62 per cent of Canadians reporting waiting less than four months—compared to 99 per cent of Germans and 94 per cent of Swiss.
While these results were disappointing, Canada reported mixed results in other areas of performance. For example, although Canada performed poorly on safety indicators such as obstetric trauma during birth (23rd of 23 countries), it performed above the OECD average on other indicators including heart attack survival rates (9th of 25 countries). But while the Canadian system has in some areas performed in line with its high spending levels, overall it’s struggled to meet many of its basic obligations—especially timely access to care.
With its latest increase in health-care spending, the Trudeau government again ignores the fact that Canada already has one of the most expensive universal health-care systems in the world. And although some of this new spending is predicated on provinces tracking progress and demonstrating improvement on certain indicators, international data reveal a simple truth—Canadians do not receive commensurate value for their health-care dollars. Without fundamental reform, it’s unlikely the new spending promised by the Trudeau government will produce improved performance for Canadian patients and their families.
Authors:
Brownstone Institute
Net Zero: The Mystery of the Falling Fertility

From the Brownstone Institute
By
If you want to argue that a mysterious factor X is responsible for the drop in fertility, you will have to explain (1) why the factor affected only the vaccinated, and (2) why it started affecting them at about the time of vaccination.
In January 2022, the number of children born in the Czech Republic suddenly decreased by about 10%. By the end of 2022, it had become clear that this was a signal: All the monthly numbers of newborns were mysteriously low.
In April 2023, I wrote a piece for a Czech investigative platform InFakta and suggested that this unexpected phenomenon might be connected to the aggressive vaccination campaign that had started approximately 9 months before the drop in natality. Denik N – a Czech equivalent of the New York Times – immediately came forward with a “devastating takedown” of my article, labeled me a liar and claimed that the pattern can be explained by demographics: There were fewer women in the population and they were getting older.
To compare fertility across countries (and time), the so-called Total Fertility Rate (TFR) is used. Roughly speaking, it is the average number of children that are born to a woman over her lifetime. TFR is independent of the number of women and of their age structure. Figure 1 below shows the evolution of TFR in several European countries between 2001 and 2023. I selected countries that experienced a similar drop in TFR in 2022 as the Czech Republic.

So, by the end of 2023, the following two points were clear:
- The drop in natality in the Czech Republic in 2022 could not be explained by demographic factors. Total fertility rate – which is independent of the number of women and their age structure – dropped sharply in 2022 and has been decreasing ever since. The data for 2024 show that the Czech TFR has decreased further to 1.37.
- Many other European countries experienced the same dramatic and unexpected decrease in fertility that started at the beginning of 2022. I have selected some of them for Figure 1 but there are more: The Netherlands, Norway, Slovakia, Slovenia, and Sweden. On the other hand, there are some countries that do not show a sudden drop in TFR, but rather a steady decline over a longer period (e.g. Belgium, France, UK, Greece, or Italy). Notable exceptions are Bulgaria, Spain, and Portugal where fertility has increased (albeit from very low numbers). The Human Fertility Project database has all the numbers.
This data pattern is so amazing and unexpected that even the mainstream media in Europe cannot avoid the problem completely. From time to time, talking heads with many academic titles appear and push one of the politically correct narratives: It’s Putin! (Spoiler alert: The war started in February 2022; however, children not born in 2022 were not conceived in 2021). It’s the inflation caused by Putin! (Sorry, that was even later). It’s the demographics! (Nope, see above, TFR is independent of the demographics).
Thus, the “v” word keeps creeping back into people’s minds and the Web’s Wild West is ripe with speculation. We decided not to speculate but to wrestle some more data from the Czech government. For many months, we were trying to acquire the number of newborns in each month, broken down by age and vaccination status of the mother. The post-socialist health-care system of our country is a double-edged sword: On one hand, the state collects much more data about citizens than an American would believe. On the other hand, we have an equivalent of the FOIA, and we are not afraid to use it. After many months of fruitless correspondence with the authorities, we turned to Jitka Chalankova – a Czech Ron Johnson in skirts – who finally managed to obtain an invaluable data sheet.
To my knowledge, the datasheet (now publicly available with an English translation here) is the only officially released dataset containing a breakdown of newborns by the Covid-19 vaccination status of the mother. We requested much more detailed data, but this is all we got. The data contains the number of births per month between January 2021 and December 2023 given by women (aged 18-39) who were vaccinated, i.e., had received at least one Covid vaccine dose by the date of delivery, and by women who were unvaccinated, i.e., had not received any dose of any Covid vaccine by the date of delivery.
Furthermore, the numbers of births per month by women vaccinated by one or more doses during pregnancy were provided. This enabled us to estimate the number of women who were vaccinated before conception. Then, we used open data on the Czech population structure by age, and open data on Covid vaccination by day, sex, and age.
Combining these three datasets, we were able to estimate the rates of successful conceptions (i.e., conceptions that led to births nine months later) by preconception vaccination status of the mother. Those interested in the technical details of the procedure may read Methods in the newly released paper. It is worth mentioning that the paper had been rejected without review in six high-ranking scientific journals. In Figure 2, we reprint the main finding of our analysis.

Figure 2 reveals several interesting patterns that I list here in order of importance:
- Vaccinated women conceived about a third fewer children than would be expected from their share of the population. Unvaccinated women conceived at about the same rate as all women before the pandemic. Thus, a strong association between Covid vaccination status and successful conceptions has been established.
- In the second half of 2021, there was a peak in the rate of conceptions of the unvaccinated (and a corresponding trough in the vaccinated). This points to rather intelligent behavior of Czech women, who – contrary to the official advice – probably avoided vaccination if they wanted to get pregnant. This concentrated the pregnancies in the unvaccinated group and produced the peak.
- In the first half of 2021, there was significant uncertainty in the estimates of the conception rates. The lower estimate of the conception rate in the vaccinated was produced by assuming that all women vaccinated (by at least one dose) during pregnancy were unvaccinated before conception. This was almost certainly true in the first half of 2021 because the vaccines were not available prior to 2021. The upper estimate was produced by assuming that all women vaccinated (by at least one dose) during pregnancy also received at least one dose before conception. This was probably closer to the truth in the second part of 2021. Thus, we think that the true conception rates for the vaccinated start close to the lower bound in early 2021 and end close to the upper bound in early 2022. Once again, we would like to be much more precise, but we have to work with what we have got.
Now that the association between Covid-19 vaccination and lower rates of conception has been established, the one important question looms: Is this association causal? In other words, did the Covid-19 vaccines really prevent women from getting pregnant?
The guardians of the official narrative brush off our findings and say that the difference is easily explained by confounding: The vaccinated tend to be older, more educated, city-dwelling, more climate change aware…you name it. That all may well be true, but in early 2022, the TFR of the whole population dropped sharply and has been decreasing ever since.
So, something must have happened in the spring of 2021. Had the population of women just spontaneously separated into two groups – rednecks who wanted kids and didn’t want the jab, and city slickers who didn’t want kids and wanted the jab – the fertility rate of the unvaccinated would indeed be much higher than that of the vaccinated. In that respect, such a selection bias could explain the observed pattern. However, had this been true, the total TFR of the whole population would have remained constant.
But this is not what happened. For some reason, the TFR of the whole population jumped down in January 2022 and has been decreasing ever since. And we have just shown that, for some reason, this decrease in fertility affected only the vaccinated. So, if you want to argue that a mysterious factor X is responsible for the drop in fertility, you will have to explain (1) why the factor affected only the vaccinated, and (2) why it started affecting them at about the time of vaccination. That is a tall order. Mr. Occam and I both think that X = the vaccine is the simplest explanation.
What really puzzles me is the continuation of the trend. If the vaccines really prevented conception, shouldn’t the effect have been transient? It’s been more than three years since the mass vaccination event, but fertility rates still keep falling. If this trend continues for another five years, we may as well stop arguing about pensions, defense spending, healthcare reform, and education – because we are done.
We are in the middle of what may be the biggest fertility crisis in the history of mankind. The reason for the collapse in fertility is not known. The governments of many European countries have the data that would unlock the mystery. Yet, it seems that no one wants to know.
Author
Addictions
More young men want to restrict pornography: survey

From LifeSiteNews
Nearly 64% of American men now believe online pornography should be more difficult to access, with even higher numbers of women saying the same thing.
A new survey has shown that an increasing number of young men want more restrictions on online pornography.
According to a survey by the American Enterprise Institute’s Survey Center on American Life, nearly 7 in 10 (69 percent) of Americans support the idea of making online pornography less accessible. In 2013, 65 percent expressed support for policies restricting internet pornography.
The most substantial increase in the support for restrictive measures on pornography could be observed in young men (age 18-24). In 2013, about half of young men favored restrictions, while 40 percent actively opposed such policies. In 2025, 64 percent of men believe accessing online pornography should be made more difficult.
The largest support for restriction on internet pornography overall could be measured among older men (65+), where 73 percent favored restrictions. An even larger percentage of women in each age group supported making online pornography less accessible. Seventy-two percent of young women (age 18-24) favored restriction, while 87 percent of women 55 years or older expressed support for less accessibility of internet pornography.
Viewing pornography is highly addictive and can lead to serious health problems. Studies have shown that children often have their first encounter with pornography at around 12 years old, with boys having a lower average age of about 10-11, and some encountering online pornography as young as 8. Studies have also shown that viewing pornography regularly rewires humans brains and that children, adolescents, and younger men are especially at risk for becoming addicted to online pornography.
According to Gary Wilson’s landmark book on the matter, “Your Brain on Porn,” pornography addiction frequently leads to problems like destruction of genuine intimate relationships, difficulty forming and maintaining real bonds in relationship, depression, social anxiety, as well as reduction of gray matter, leading to desensitization and diminished pleasure from everyday activities among many others.
-

 Business2 days ago
Business2 days agoWEF-linked Linda Yaccarino to step down as CEO of X
-

 Freedom Convoy2 days ago
Freedom Convoy2 days agoCourt Orders Bank Freezing Records in Freedom Convoy Case
-
 Crime2 days ago
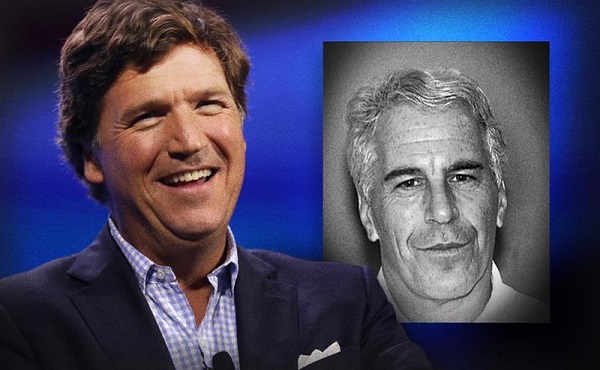
Crime2 days agoTucker Carlson: US intelligence is shielding Epstein network, not President Trump
-

 Business1 day ago
Business1 day ago‘Experts’ Warned Free Markets Would Ruin Argentina — Looks Like They Were Dead Wrong
-

 Automotive1 day ago
Automotive1 day agoAmerica’s EV Industry Must Now Compete On A Level Playing Field
-

 International1 day ago
International1 day agoSecret Service suspends six agents nearly a year after Trump assassination attempt
-

 Business1 day ago
Business1 day agoCarney government should recognize that private sector drives Canada’s economy
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoThe Covid 19 Disaster: When Do We Get The Apologies?