Business
BREAKING ALERT: Trump Threatens 25% Tariff on All Goods From Canada and Mexico, Cites Flood of Fentanyl and Illegal Migrants

In a stunning announcement Monday, President-Elect Donald Trump vowed swift action to combat what he described as a surge in fentanyl trafficking and illegal migration at the U.S. borders with Mexico and Canada.
Trump pledged to impose a 25% tariff on all imports from both countries, citing their alleged failure to address the crises. He announced the policy would be enacted through an Executive Order on January 20, the day he officially takes office.
“Thousands of people are pouring through Mexico and Canada, bringing Crime and Drugs at levels never seen before,” Trump said in a statement. He singled out an incoming “unstoppable” caravan from Mexico as emblematic of what he described as the failures of both neighboring countries to address the crisis.
“This Tariff will remain in effect until such time as Drugs, in particular Fentanyl, and all Illegal Aliens stop this Invasion of our Country!” Trump posted on his Truth Social platform.
The backdrop to Trump’s shocking policy against Canada—long perceived as a strong ally of the U.S.—includes a recent high-profile case against TD Bank in the United States, resulting in a multi-billion-dollar fine. Months prior to Trump’s announcement, David Asher, a former Trump administration official and consultant on DEA investigations related to the TD probe, told The Bureau that U.S. investigators believe the “command and control” for the fentanyl money-laundering networks allegedly cited in the TD case leads directly to Toronto and Vancouver.
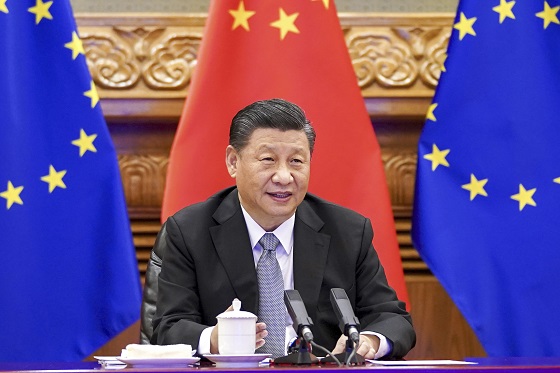
These networks—according to Asher—involve transnational Triads laundering cash from fentanyl distributed in America by Mexican cartels, who source their precursors from China.
In an exclusive interview with The Bureau, Asher criticized the Canadian government for inadequate cooperation in broader fentanyl-trafficking and Triad money laundering investigations, pointing to gang leaders in Canada with alleged ties to Beijing. Asher suggested that possible political and financial influences are hampering effective law enforcement in Canada.
“The key thing is the Canadian connection, and in almost all the investigations as far as money laundering, we saw the command control seemed to go back to our network analysis. When we seized their phones, we’d see Canada light up like a Christmas tree, especially Toronto, and also British Columbia,” Asher said.
Regarding allegations that Triads in Toronto and Vancouver are running fentanyl money-laundering networks for Mexican cartels, Asher added: “The question is, what does the Canadian government know, and why haven’t they tried to judicially prosecute?”
Asher emphasized that the failure to disrupt these networks is contributing to the ongoing fentanyl crisis, which claims tens of thousands of lives annually in the U.S. and Canada.
Furthermore, Asher disclosed that U.S. Congressional investigators allege the People’s Republic of China is not only incentivizing fentanyl precursor exports but also methamphetamine sales.
The tariff, Trump emphasized, will remain until Mexico and Canada take what he called their “absolute right and power” to stop the flow of illegal drugs and migrants.
“We hereby demand that they use this power, and until such time that they do, it is time for them to pay a very big price,” Trump declared.
The announcement has already sparked sharp reactions from political leaders and trade experts. Critics warn that such sweeping tariffs could disrupt North American trade agreements and exacerbate economic tensions with key allies.
This is a developing story. Stay tuned to The Bureau for updates.
The Bureau is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Business
Is Government Inflation Reporting Accurate?


 David Clinton
David Clinton
Who ya gonna believe: official CPI figures or your lyin’ eyes?
Great news! We’ve brought inflation back under control and stuff is now only costing you 2.4 percent more than it did last year!
That’s more or less the message we’ve been hearing from governments over the past couple of years. And in fact, the official Statistics Canada consumer price index (CPI) numbers do show us that the “all-items” index in 2024 was only 2.4 percent higher than in 2023. Fantastic.
So why doesn’t it feel fantastic?
Well statistics are funny that way. When you’ve got lots of numbers, there are all kinds of ways to dress ‘em up before presenting them as an index (or chart). And there really is no one combination of adjustments and corrections that’s definitively “right”. So I’m sure Statistics Canada isn’t trying to misrepresent things.
But I’m also curious to test whether the CPI is truly representative of Canadians’ real financial experiences. My first attempt to create my own alternative “consumer price index”, involved Statistics Canada’s “Detailed household final consumption expenditure”. That table contains actual dollar figures for nation-wide spending on a wide range of consumer items. To represent the costs Canadian’s face when shopping for basics, I selected these nine categories:
- Food and non-alcoholic beverages
- Clothing and footwear
- Housing, water, electricity, gas and other fuels
- Major household appliances
- Pharmaceutical products and other medical products (except cannabis)
- Transport
- Communications
- University education
- Property insurance
I then took the fourth quarter (Q4) numbers for each of those categories for all the years between 2013 and 2024 and divided them by the total population of the country for each year. That gave me an accurate picture of per capita spending on core cost-of-living items.
Overall, living and breathing through Q4 2013 would have cost the average Canadian $4,356.38 (or $17,425.52 for a full year). Spending for those same categories in Q4 2024, however, cost us $6,266.48 – a 43.85 percent increase.
By contrast, the official CPI over those years rose only 31.03 percent. That’s quite the difference. Here’s how the year-over-year changes in CPI inflation vs actual spending inflation compare:
As you can see, with the exception of 2020 (when COVID left us with nothing to buy), the official inflation number was consistently and significantly lower than actual spending. And, in the case of 2021, it was more than double.
Since 2023, the items with the largest price growth were university education (57.46 percent), major household appliances (52.67 percent), and housing, water, electricity, gas, and other fuels (50.79).
Having said all that, you could justifiably argue that the true cost of living hasn’t really gone up that much, but that at least part of the increase in spending is due to a growing taste for luxury items and high volume consumption. I can’t put a precise number on that influence, but I suspect it’s not trivial.
Since data on spending doesn’t seem to be the best measure of inflation, perhaps I could build my own basket of costs and compare those numbers to the official CPI. To do that, I collected average monthly costs for gasoline, home rentals, a selection of 14 core grocery items, and taxes paid by the average Canadian homeowner.¹ I calculated the tax burden (federal, provincial, property, and consumption) using the average of the estimates of two AI models.
How did the inflation represented by my custom basket compare with the official CPI? Well between 2017 and 2024, the Statistics Canada’s CPI grew by 23.39 percent. Over that same time, the monthly cost of my basket grew from $4,514.74 to $5,665.18; a difference of 25.48 percent. That’s not nearly as dramatic a difference as we saw when we measured spending, but it’s not negligible either.
The very fact that the government makes all this data freely available to us is evidence that they’re not out to hide the truth. But it can’t hurt to keep an active and independent eye on them, too.
Subscribe to The Audit.
For the full experience, upgrade your subscription.
2025 Federal Election
Carney’s Hidden Climate Finance Agenda

From Energy Now
By Tammy Nemeth and Ron Wallace
It is high time that Canadians discuss and understand Mark Carney’s avowed plan to re-align capital with global Net Zero goals.
Mark Carney’s economic vision for Canada, one that spans energy, housing and defence, rests on an unspoken, largely undisclosed, linchpin: Climate Finance – one that promises a Net Zero future for Canada but which masks a radical economic overhaul.
Regrettably, Carney’s potential approach to a Net Zero future remains largely unexamined in this election. As the former chair of the Glasgow Financial Alliance for Net Zero (GFANZ), Carney has proposed new policies, offices, agencies, and bureaus required to achieve these goals.. Pieced together from his presentations, discussions, testimonies and book, Carney’s approach to climate finance appears to have four pillars: mandatory climate disclosures, mandatory transition plans, centralized data sharing via the United Nations’ Net Zero Data Public Utility (NZDPU) and compliance with voluntary carbon markets (VCMs). There are serious issues for Canada’s economy if these principles were to form the core values for policies under a potential Liberal government.
About the first pillar Carney has been unequivocal: “Achieving net zero requires a whole economy transition.” This would require a restructuring energy and financial systems to shift away from fossil fuels to renewable energy with Carney insisting repeatedly in his book that “every financial [and business] decision takes climate change into account.” Climate finance, unlike broader sustainable finance with its Environmental, Social, and Governance (ESG) focus would channel capital into sectors aligned with a 2050 Net Zero trajectory. Carney states: “Companies, and those who invest in them…who are part of the solution, will be rewarded. Those lagging behind…will be punished.” In other words, capital would flow to compliant firms but be withheld from so-called “high emitters”.
How will investors, banks and insurers distinguish solution from problem? Mandatory climate disclosures, aligned with the International Sustainability Standards Board (ISSB), would compel firms to report emissions and outline their Net Zero strategies. Canada’s Sustainability Standards Board has adopted these methodologies, despite concerns they would disadvantage Canadian businesses. Here, Carney repeatedly emphasizes disclosures as the cornerstone to track emissions data required to shift capital away from “high emitters”. Without this, he claims, large institutional investors lack the data on supply chains to make informed decisions to shift capital to businesses that are Net Zero compliant.
The second pillar, Mandatory Transition Plans would require companies to map a 2050 Net Zero trajectory for emission reduction targets. Failure to meet those targets would invite pressure from investors, banks, or activists, who may pursue litigation for non-compliance. The UK’s Transition Plan Task Force, now part of ISSB, provides this standardized framework. Carney, while at GFANZ, advocated using transition plans for a “managed phase-out” of high-emitting assets like coal, oil and gas, not just through divestment but by financing emissions reductions. “As part of their transition planning, [GFANZ] members should establish and apply financing policies to phase out and align carbon-intensive sectors and activities, such as thermal coal, oil and gas and deforestation, not only through asset divestment but also through transition finance that reduces real world emissions. To assist with these efforts GFANZ will continue to develop and implement a framework for the Managed Phase-out of high-emitting assets.” Clearly, the purpose of this is to ensure companies either decarbonize or face capital withdrawal.
The third pillar is the United Nations’ Net Zero Data Public Utility (NZDPU), a centralized platform for emissions and transition data. Carney insists these data be freely accessible, enabling investors, banks and insurers to judge companies’ progress to Net Zero. As Carney noted in 2021: “Private finance is judging…banks, pension funds and asset managers have to show where they are in the transition to Net Zero.” Hence, compliant firms would receive investment; laggards would face divestment.
Finally, voluntary carbon markets (VCMs) allow companies to offset emissions by purchasing credits from projects like reforestation. Carney, who launched the Taskforce on Scaling VCMs in 2020, has insisted on monitoring, verification and lifecycle tracking. At a 2024 Beijing conference, he suggested major jurisdictions could establish VCMs by COP 30 (planned for 2025 in Brazil) to create a global market. If Canada mandates VCMs, businesses especially small and medium enterprises (SMEs) would face much higher compliance costs with credits available only to those that demonstrate progress with transition plans.
These potential mandatory disclosures and transition plans would burden Canadian businesses with material costs and legal risks that constitute an economic gamble which few may recognize but all should weigh. Do Canadians truly want a government that has an undisclosed climate finance agenda that would be subservient to an opaque globalized Net Zero agenda?
Tammy Nemeth is a U.K.-based strategic energy analyst. Ron Wallace is an executive fellow of the Canadian Global Affairs Institute and the Canada West Foundation.
-
 2025 Federal Election15 hours ago
2025 Federal Election15 hours agoStudy links B.C.’s drug policies to more overdoses, but researchers urge caution
-

 conflict1 day ago
conflict1 day agoMarco Rubio says US could soon ‘move on’ from Ukraine conflict: ‘This is not our war’
-

 Business1 day ago
Business1 day agoChinese firm unveils palm-based biometric ID payments, sparking fresh privacy concerns
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoMark Carney Wants You to Forget He Clearly Opposes the Development and Export of Canada’s Natural Resources
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPolice Associations Endorse Conservatives. Poilievre Will Shut Down Tent Cities
-

 Alberta2 days ago
Alberta2 days agoRed Deer Justice Centre Grand Opening: Building access to justice for Albertans
-
 Business2 days ago
Business2 days agoTrump: China’s tariffs to “come down substantially” after negotiations with Xi
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoFormer WEF insider accuses Mark Carney of using fear tactics to usher globalism into Canada