Health
21 states threaten top medical group with legal action for claiming puberty blockers are ‘reversible’

Idaho Attorney General Raul Labrador
From LifeSiteNews
Idaho Attorney General Raul Labrador is leading a group of 21 states in warning the American Academy of Pediatrics that its ‘evidence-free’ endorsement of ‘transitioning’ minors violates most states’ consumer protection laws.
More than 20 state attorneys general are banding together to warn the American Academy of Pediatrics (AAP) that it could face legal action if it continues to promote surgical and chemical “transitioning” of gender-confused minors, Idaho’s top law enforcement official Raul Labrador announced Tuesday.
As previously covered by LifeSiteNews, the AAP sides firmly with LGBT activists on how to approach children suffering from gender dysphoria, endorsing the use of puberty blockers, cross-sex hormones, and surgical transformation of developing bodies, going so far as to accuse states that deny minors so-called “gender-affirming care” of “state-sanctioned medical neglect and emotional abuse.”
AAP’s position is based on “evidence free standards,” the Idaho Attorney General’s Office contends, the “most concerning” of which is its claim that the “use of puberty blockers on children is safe and reversible. This assertion is not grounded in evidence and therefore may run afoul of consumer protection laws in most states.”
“When used to suppress hormones below normal ranges during or before puberty, puberty blockers: (1) may interfere with neurocognitive development; (2) compromise bone density and may negatively affect metabolic health and weight; and (3) block normal pubertal experience and experimentation,” reads the coalition’s letter to outgoing AAP president Benjamin Hoffman and his incoming successor Susan Kressley. “And when puberty blocker use is followed directly by cross-sex hormone use, which is often the case, infertility and sterility is a known consequence, at least for those who began puberty blockers in early puberty.”
“Telling parents and children that puberty blockers are ‘reversible’ at the very least conveys assurance that no permanent harm or change will occur. But that claim cannot be made in the face of the unstudied and ‘novel’ use of puberty blockers” for gender dysphoria, it continues. “It is even less defensible now that the World Professional Association for Transgender Health and its standards of care—the AAP’s apparent cornerstone source—have been exposed as unreliable and influenced by improper pressures,” referring to revelations earlier this year that Biden administration officials pressured WPATH to remove age limits.
The attorneys general of Alabama, Arkansas, Florida, Georgia, Idaho, Iowa, Kansas, Louisiana, Mississippi, Missouri, Montana, Nebraska, North Dakota, Ohio, South Carolina, South Dakota, Texas, Utah, Virginia, and West Virginia, as well as the Arizona Legislature, went on to threaten legal consequences for AAP if it does not reverse course.
“Idaho law, for example, prohibits ‘[e]ngaging in any act or practice that is otherwise misleading, false, or deceptive to the consumer,’” the letter says. “Most other states likewise prohibit making statements to consumers that are false, misleading, or deceptive. Each of us takes our responsibility to protect consumers in our states very seriously.”
The AAP has until October 18 to answer a series of information requests about its decision-making process on the subject.
“It is shameful the most basic tenet of medicine – do no harm – has been abandoned by professional associations when politically pressured,” Labrador said. “These organizations are sacrificing the health and well-being of children with medically unproven [procedures] that leave a wake of permanent damage […] Parents should be able to trust that a doctor’s medical guidance isn’t just the latest talking point from a dangerous and discredited activist agenda.”
A significant body of evidence shows that “affirming” gender confusion carries serious harms, especially when done with impressionable children who lack the mental development, emotional maturity, and life experience to consider the long-term ramifications of the decisions being pushed on them, or full knowledge about the long-term effects of life-altering, physically-transformative, and often-irreversible surgical and chemical procedures.
Studies find that more than 80% of children suffering gender dysphoria outgrow it on their own by late adolescence and that “transition” procedures, including “reassignment” surgery, fail to resolve gender-confused individuals’ heightened tendency to engage in self-harm and suicide – and even exacerbate it, including by reinforcing their confusion and neglecting the actual root causes of their mental strife.
Many oft-ignored “detransitioners,” individuals who attempted to live under a different “gender identity” before embracing their sex, attest to the physical and mental harm of reinforcing gender confusion, as well as to the bias and negligence of the medical establishment on the subject, many of whom take an activist approach to their profession and begin cases with a predetermined conclusion in favor of “transitioning.”
“Gender-affirming” physicians have also been caught on video admitting to more old-fashioned motives for such procedures, as with an 2022 exposé about Vanderbilt University Medical Center’s Clinic for Transgender Health, where Dr. Shayne Sebold Taylor said outright that “these surgeries make a lot of money.”
Addictions
Addiction experts demand witnessed dosing guidelines after pharmacy scam exposed

By Alexandra Keeler
The move follows explosive revelations that more than 60 B.C. pharmacies were allegedly participating in a scheme to overbill the government under its safer supply program. The scheme involved pharmacies incentivizing clients to fill prescriptions they did not require by offering them cash or rewards. Some of those clients then sold the drugs on the black market.
An addiction medicine advocacy group is urging B.C. to promptly issue new guidelines for witnessed dosing of drugs dispensed under the province’s controversial safer supply program.
In a March 24 letter to B.C.’s health minister, Addiction Medicine Canada criticized the BC Centre on Substance Use for dragging its feet on delivering the guidelines and downplaying the harms of prescription opioids.
The centre, a government-funded research hub, was tasked by the B.C. government with developing the guidelines after B.C. pledged in February to return to witnessed dosing. The government’s promise followed revelations that many B.C. pharmacies were exploiting rules permitting patients to take safer supply opioids home with them, leading to abuse of the program.
“I think this is just a delay,” said Dr. Jenny Melamed, a Surrey-based family physician and addiction specialist who signed the Addiction Medicine Canada letter. But she urged the centre to act promptly to release new guidelines.
“We’re doing harm and we cannot just leave people where they are.”
Addiction Medicine Canada’s letter also includes recommendations for moving clients off addictive opioids altogether.
“We should go back to evidence-based medicine, where we have medications that work for people in addiction,” said Melamed.
‘Best for patients’
On Feb. 19, the B.C. government said it would return to a witnessed dosing model. This model — which had been in place prior to the pandemic — will require safer supply participants to take prescribed opioids under the supervision of health-care professionals.
The move follows explosive revelations that more than 60 B.C. pharmacies were allegedly participating in a scheme to overbill the government under its safer supply program. The scheme involved pharmacies incentivizing clients to fill prescriptions they did not require by offering them cash or rewards. Some of those clients then sold the drugs on the black market.
In its Feb. 19 announcement, the province said new participants in the safer supply program would immediately be subject to the witnessed dosing requirement. For existing clients of the program, new guidelines would be forthcoming.
“The Ministry will work with the BC Centre on Substance Use to rapidly develop clinical guidelines to support prescribers that also takes into account what’s best for patients and their safety,” Kendra Wong, a spokesperson for B.C.’s health ministry, told Canadian Affairs in an emailed statement on Feb. 27.
More than a month later, addiction specialists are still waiting.
According to Addiction Medicine Canada’s letter, the BC Centre on Substance Use posed “fundamental questions” to the B.C. government, potentially causing the delay.
“We’re stuck in a place where the government publicly has said it’s told BCCSU to make guidance, and BCCSU has said it’s waiting for government to tell them what to do,” Melamed told Canadian Affairs.
This lag has frustrated addiction specialists, who argue the lack of clear guidance is impeding the transition to witnessed dosing and jeopardizing patient care. They warn that permitting take-home drugs leads to more diversion onto the streets, putting individuals at greater risk.
“Diversion of prescribed alternatives expands the number of people using opioids, and dying from hydromorphone and fentanyl use,” reads the letter, which was also co-signed by Dr. Robert Cooper and Dr. Michael Lester. The doctors are founding board members of Addiction Medicine Canada, a nonprofit that advises on addiction medicine and advocates for research-based treatment options.
“We have had people come in [to our clinic] and say they’ve accessed hydromorphone on the street and now they would like us to continue [prescribing] it,” Melamed told Canadian Affairs.
A spokesperson for the BC Centre on Substance Use declined to comment, referring Canadian Affairs to the Ministry of Health. The ministry was unable to provide comment by the publication deadline.
Big challenges
Under the witnessed dosing model, doctors, nurses and pharmacists will oversee consumption of opioids such as hydromorphone, methadone and morphine in clinics or pharmacies.
The shift back to witnessed dosing will place significant demands on pharmacists and patients. In April 2024, an estimated 4,400 people participated in B.C.’s safer supply program.
Chris Chiew, vice president of pharmacy and health-care innovation at the pharmacy chain London Drugs, told Canadian Affairs that the chain’s pharmacists will supervise consumption in semi-private booths.
Nathan Wong, a B.C.-based pharmacist who left the profession in 2024, fears witnessed dosing will overwhelm already overburdened pharmacists, creating new barriers to care.
“One of the biggest challenges of the retail pharmacy model is that there is a tension between making commercial profit, and being able to spend the necessary time with the patient to do a good and thorough job,” he said.
“Pharmacists often feel rushed to check prescriptions, and may not have the time to perform detailed patient counselling.”
Others say the return to witnessed dosing could create serious challenges for individuals who do not live close to health-care providers.
Shelley Singer, a resident of Cowichan Bay, B.C., on Vancouver Island, says it was difficult to make multiple, daily visits to a pharmacy each day when her daughter was placed on witnessed dosing years ago.
“It was ridiculous,” said Singer, whose local pharmacy is a 15-minute drive from her home. As a retiree, she was able to drive her daughter to the pharmacy twice a day for her doses. But she worries about patients who do not have that kind of support.
“I don’t believe witnessed supply is the way to go,” said Singer, who credits safer supply with saving her daughter’s life.
Melamed notes that not all safer supply medications require witnessed dosing.
“Methadone is under witness dosing because you start low and go slow, and then it’s based on a contingency management program,” she said. “When the urine shows evidence of no other drug, when the person is stable, [they can] take it at home.”
She also noted that Suboxone, a daily medication that prevents opioid highs, reduces cravings and alleviates withdrawal, does not require strict supervision.
Kendra Wong, of the B.C. health ministry, told Canadian Affairs that long-acting medications such as methadone and buprenorphine could be reintroduced to help reduce the strain on health-care professionals and patients.
“There are medications available through the [safer supply] program that have to be taken less often than others — some as far apart as every two to three days,” said Wong.
“Clinicians may choose to transition patients to those medications so that they have to come in less regularly.”
Such an approach would align with Addiction Medicine Canada’s recommendations to the ministry.
The group says it supports supervised dosing of hydromorphone as a short-term solution to prevent diversion. But Melamed said the long-term goal of any addiction treatment program should be to reduce users’ reliance on opioids.
The group recommends combining safer supply hydromorphone with opioid agonist therapies. These therapies use controlled medications to reduce withdrawal symptoms, cravings and some of the risks associated with addiction.
They also recommend limiting unsupervised hydromorphone to a maximum of five 8 mg tablets a day — down from the 30 tablets currently permitted with take-home supplies. And they recommend that doses be tapered over time.
“This protocol is being used with success by clinicians in B.C. and elsewhere,” the letter says.
“Please ensure that the administrative delay of the implementation of your new policy is not used to continue to harm the public.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
Autism
RFK Jr. Completely Shatters the Media’s Favorite Lie About Autism

 The Vigilant Fox
The Vigilant Fox
They say autism is rising because of “better diagnosis”—but RFK Jr. just blew that narrative wide open. He brought the hard data and dropped one undeniable truth the denialists can’t explain.
HHS Secretary Robert Kennedy Jr. appeared on Hannity Thursday evening and unloaded on the predominant autism narrative. It started with a bombshell reveal from Kennedy’s own childhood.
Hannity asked: “What was the number when you were a kid—and what do you think is going on?”
Kennedy replied: “There’s really good data on that.”
He pointed to one of the largest studies ever conducted—900,000 children in Wisconsin, published in a top-tier medical journal.
“It looked at 900,000 kids. It was published in a high-gravitas journal, peer-reviewed study, and they found the rate to be 0.7 out of 10,000.”
That’s less than 1 in 10,000. Today? It’s around 1 in 31.
Let that sink in.
Join 110K+ Substack readers and 1.6 million 𝕏 users who follow the work of Vigilant Fox.
Subscribe for top-tier news aggregation and exclusive stories you won’t find anywhere else.
That’s when Kennedy sounded the alarm on what’s happening now—and why it’s so catastrophic. He said the rise isn’t just in frequency—it’s in severity.
“Two years ago, it was 1 in 36. The CDC data we released this week shows 1 in 31,” Kennedy said.
“The worst state is California,” Kennedy continued, “which actually has the best collection methodologies. So they actually, probably reflect what we’re seeing nationwide.”
“In California, it’s 1 in every 20 kids, and 1 in every 12.5 boys,” he explained.
Even worse, he said the numbers are likely underreported in minority communities. And for many kids, the symptoms are devastating:
“About 25% of the population of those kids with autism, about 25% of them are nonverbal, nontoilet trained,” Kennedy explained.
“They have all of these stereotypical behaviors, the head banging, biting, toe walking, stimming, and that population is growing higher and higher.”
“It’s becoming a larger percentage, so we’re seeing many more cases that are now linked to severe intellectual disability.”
He says it’s a glaring red warning sign—and it’s past time to start acting on it.
And this was the moment that Kennedy took a flamethrower to the media narrative about autism. He shattered the core excuse we’ve all been fed—that this epidemic isn’t real, that it’s just a change in how we count it.
He’s not buying it.
“The media has bought into this industry canard, this mythology, that we’re just seeing more autism because we’re noticing it more. We’re better at recognizing it or there’s been changing diagnostic criteria.”
But the scientific literature, Kennedy said, says otherwise.
“There is study after study in the scientific literature going back, and they decided that the literature going back says decades that says that’s not true.”
He then cited a major investigation by California’s own lawmakers.
“In fact, the California legislature… asked the Mind Institute at UC Davis to look exactly at that topic. They [asked], is it real or are we just noticing it more? The Mind Institute came back and said, ‘Absolutely this is a real epidemic. This is something we’ve never seen before.’”
And he made it painfully clear:
“Anybody with common sense, Sean, would notice that, because the autism—this epidemic is only happening in our children. It’s not happening in people who are our age. And if it was better recognition, you’d see it in 70-year-old men.”
But we don’t.
And after laying out the data, dismantling the media narrative, and exposing the severity of the crisis, Kennedy concluded with a clarion call to get to the bottom of this epidemic.
That’s why he says it’s time to dig deeper—leave no stone unturned, and we may have answers sooner than you think.
“President Trump asked me to find out what’s causing it,” he told Hannity.
“And I am approaching that agnostically. We are looking at everything, we are going to do, we’re going to be very transparent in how we design the studies.”
To get real answers, he’s farming the research out to top institutions across the country—with full transparency from day one.
“We’re going to farm the studies out to 15 premier research groups from all over the country. And we’re going to be transparent about our protocols, about the data sets, and then every study will have to be replicated.”
The list of possible factors is long—and nothing is being ruled out, Kennedy explained.
“We’re going to look at mold. We’re going to look at the age of parents. We’re going to look at food and food additives. We’re going to look at pesticides and toxic exposures. We’re going to look at medicines. We’re going to look at vaccines. We’re going to look at everything.”
When asked how long it would take, Kennedy didn’t miss a beat.
“I think we’ll have some preliminary answers in six months. It will take us probably a year from then before we can have definitive answers because a lot of the studies will not go out until the end of the summer.”
For the first time in decades, someone is asking the hard questions—and demanding real answers.
This time, nothing is off-limits.
Thanks for reading. If you value the work being published here, upgrading your subscription is the most powerful way to support it. The more this Substack earns, the more I can do to improve quality and create the best reader experience possible.
Thank you for your support.
-

 International2 days ago
International2 days agoPope Francis has died aged 88
-

 International1 day ago
International1 day agoJD Vance was one of the last people to meet Pope Francis
-

 International1 day ago
International1 day agoPope Francis Dies on Day after Easter
-

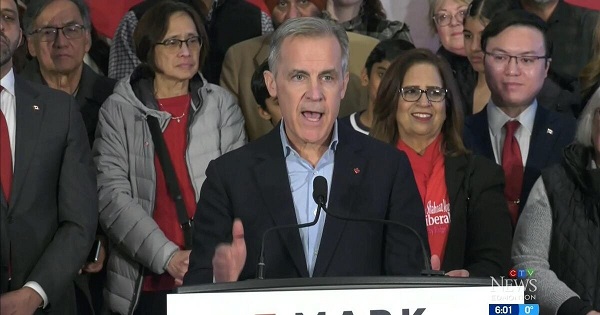
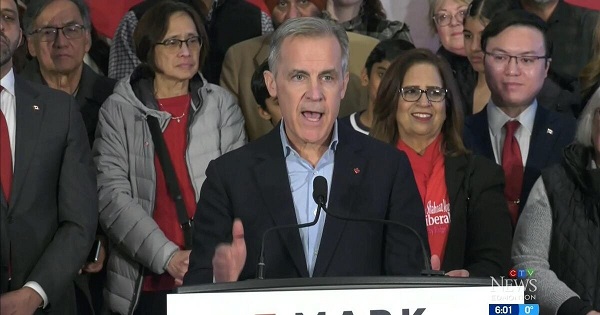
 2025 Federal Election20 hours ago
2025 Federal Election20 hours agoOttawa Confirms China interfering with 2025 federal election: Beijing Seeks to Block Joe Tay’s Election
-
 2025 Federal Election19 hours ago
2025 Federal Election19 hours agoHow Canada’s Mainstream Media Lost the Public Trust
-

 Business2 days ago
Business2 days agoCanada Urgently Needs A Watchdog For Government Waste
-
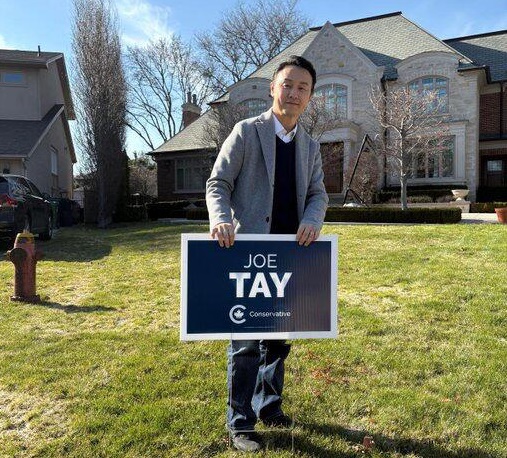
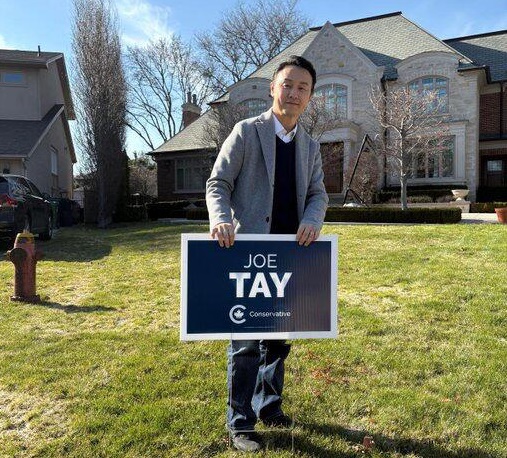 2025 Federal Election10 hours ago
2025 Federal Election10 hours agoCHINESE ELECTION THREAT WARNING: Conservative Candidate Joe Tay Paused Public Campaign
-

 Energy1 day ago
Energy1 day agoIndigenous-led Projects Hold Key To Canada’s Energy Future












