Health
Canadian provinces push back after Trudeau’s health minister says MAiD will eventually be expanded

Liberal Health Minister Mark Holland
From LifeSiteNews
Holland has told Canadians that the government, is still seeking to expand MAiD (Medical Assistance in Dying) to those suffering from mental health issues; it just needs more time to prepare the ‘system.’
The Trudeau government still intends to provide euthanasia to mentally ill Canadians, but provincial health ministers are asking for the measure to be “indefinitely” postponed.
On January 30, health ministers from Ontario, Alberta, New Brunswick, Nova Scotia, Saskatchewan, Prince Edward Island, British Columbia, Yukon, Northwest Territories, and Nunavut appealed to Liberal Health Minister Mark Holland to “indefinitely pause” expanding MAiD eligibility to the mentally ill.
Health ministers from ON, AB, NB, NS, SK, PEI, BC, Yukon, NWT, and Nunavut are calling on Ottawa to "indefinitely pause" expanding MAID eligibility to mental illness.
Concerns about a consistent and safe approach, time for training, and an expected jump in patients#CdnPoli pic.twitter.com/1Hh4oJfsER
— Colton Praill (@ColtonPraill) January 30, 2024
On January 29, Holland told Canadians that the Liberal government, under the leadership of Prime Minister Justin Trudeau, is still seeking to expand MAiD (Medical Assistance in Dying) to those suffering from mental health issues; it just needs more time to prepare the “system.”
“We agree with the conclusion that the committee has come to that the system is not ready, and more time is required,” Holland told reporters, referring to a report that “fundamental issues” regarding the expansion have yet to be resolved.
Trudeau's health minister says "the system is at this time not ready and more time is required" to expand MAiD to those for whom mental illness is "the sole underlying condition" pic.twitter.com/Z4hYcduaWh
— The Post Millennial (@TPostMillennial) January 29, 2024
The new provision, which was to take effect in March, would have relaxed legislation around so-called MAiD to include those suffering solely from mental illness. This is a result of the 2021 passage of Bill C-7, which also allowed the chronically ill – not just the terminally ill – to qualify for so-called doctor-assisted death.
On Monday, following pushback from Canadians, Holland announced that Canada is not ready for the expansion and has determined to delay it. However, Holland stressed that this is not an abandonment of the new policy but merely a postponement.
“There are people who have, for decades, been trapped in mental torture, being in a horrific situation where they have tried everything and exhausted all avenues and under their own recognisance are saying that they want access to MAiD,” he claimed.
“What we’re saying is that … someone in that intractable situation … should have that right, but the system needs to be ready, and the system needs to get it right,” he added, not explaining how being killed would help their situation.
Holland did not reveal when the expansion is expected to take effect but disclosed that “those individuals are gonna have to wait a little longer” to end their lives by lethal injection.
Reporter: "Is your intention to still move ahead with MAiD for mental illness, just within a longer timeframe?"
Trudeau's health minister: "That's correct." pic.twitter.com/XzGs7QoexU
— The Post Millennial (@TPostMillennial) January 29, 2024
The Liberal government’s desire to expand MAiD to those suffering with mental health issues comes despite several experts, and provincial health ministers, warning against the move.
RELATED: Canada’s top pro-life group urges Trudeau gov’t to drop euthanasia expansion entirely
The provincial health ministers’ appeal echoes that of leading Canadian psychiatrist Dr. K. Sonu Gaind, who testified that the expansion of MAiD “is not so much a slippery slope as a runaway train.”
Similarly, in November, several Canadian psychiatrists warned that the country is “not ready” for the coming expansion of euthanasia to those who are mentally ill. They said that further liberalizing the procedure is not something that “society should be doing” as it could lead to deaths under a “false pretence.”
The expansion of euthanasia to those with mental illness even has the far-left New Democratic Party (NDP) concerned. Dismissing these concerns, a Trudeau Foundation fellow actually said Trudeau’s current euthanasia regime is marked by “privilege,” assuring the Canadian people that most of those being put to death are “white,” “well off,” and “highly educated.”
The most recent reports show that MAiD is the sixth highest cause of death. However, it was not listed as such in Statistics Canada’stop 10 leading causes of death from 2019 to 2022. When asked why MAiD was left off the list, the agency explained that it records the illnesses that led Canadians to choose to end their lives via euthanasia, not the actual cause of death, as the primary cause of death.
According to Health Canada, in 2022, 13,241 Canadians died by MAiD lethal injections. This accounts for 4.1 percent of all deaths in the country for that year,a 31.2 percent increase from 2021.
While the numbers for 2023 have yet to be released, all indications point to a situation even more grim than 2022.
Meanwhile, the pro-life Euthanasia Prevention Coalition (EPC)has launched a campaign to have the expansion thrown out. The campaign includes a rally and media conference on Parliament Hill on February 6 at 11 a.m. local time.
The movement also features a parliamentary postcard campaign, encouraging Canadians to send letters stating: “I demand that the government reverse its decision to permit ‘MAiD’ for mental illness alone.”
EPC also launched a petition to urge the Justice Minister to offer real care to those suffering from mental illness and not death by lethal injection.
armed forces
Yet another struggling soldier says Veteran Affairs Canada offered him euthanasia

From LifeSiteNews
‘It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself.’
Yet another Canadian combat veteran has come forward to reveal that when he sought help, he was instead offered euthanasia.
David Baltzer, who served two tours in Afghanistan with the Princess Patricia’s Canadian Light Infantry, revealed to the Toronto Sun that he was offered euthanasia on December 23, 2019—making him, as the Sun noted, “among the first Canadian soldiers offered therapeutic suicide by the federal government.”
Baltzer had been having a disagreement with his existing caseworker, when assisted suicide was brought up in in call with a different agent from Veteran Affairs Canada.
“It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself,” Baltzer told the Sun.“I was in my lowest down point, it was just before Christmas. He says to me, ‘I would like to make a suggestion for you. Keep an open mind, think about it, you’ve tried all this and nothing seems to be working, but have you thought about medical-assisted suicide?’”
Baltzer was stunned. “It just seems to me that they just want us to be like ‘f–k this, I give up, this sucks, I’d rather just take my own life,’” he said. “That’s how I honestly felt.”
Baltzer, who is from St. Catharines, Ontario, joined up at age 17, and moved to Manitoba to join the Princess Patricia’s Canadian Light Infantry, one of Canada’s elite units. He headed to Afghanistan in 2006. The Sun noted that he “was among Canada’s first troops deployed to Afghanistan as part Operation Athena, where he served two tours and saw plenty of combat.”
“We went out on long-range patrols trying to find the Taliban, and that’s exactly what we did,” Baltzer said. “The best way I can describe it, it was like Black Hawk Down — all of the sudden the s–t hit the fan and I was like ‘wow, we’re fighting, who would have thought? Canada hasn’t fought like this since the Korean War.”
After returning from Afghanistan, Baltzer says he was offered counselling by Veteran Affairs Canada, but it “was of little help,” and he began to self-medicate for his trauma through substance abuse (he noted that he is, thankfully, doing well today). Baltzer’s story is part of a growing scandal. As the Sun reported:
A key figure shedding light on the VAC MAID scandal was CAF veteran Mark Meincke, whose trauma-recovery podcast Operation Tango Romeo broke the story. ‘Veterans, especially combat veterans, usually don’t reach out for help until like a year longer than they should’ve,’ Meincke said, telling the Sun he waited over two decades before seeking help.
‘We’re desperate by the time we put our hands up for help. Offering MAID is like throwing a cinderblock instead of a life preserver.’ Meincke said Baltzer’s story shoots down VAC’s assertions blaming one caseworker for offering MAID to veterans, and suggests the problem is far more serious than some rogue public servant.
‘It had to have been policy. because it’s just too many people in too many provinces,” Meincke told the Sun. “Every province has service agents from that province.’
Veterans Affairs Canada claimed in 2022 that between four and 20 veterans had been offered assisted suicide; Meincke “personally knows of five, and said the actual number’s likely close to 20.” In a previous investigation, VAC claimed that only one caseworker was responsible—at least for the four confirmed cases—and that the person “was lo longer employed with VAC.” Baltzer says VAC should have military vets as caseworkers, rather than civilians who can’t understand what vets have been through.
To date, no federal party leader has referenced Canada’s ongoing euthanasia scandals during the 2025 election campaign.
2025 Federal Election
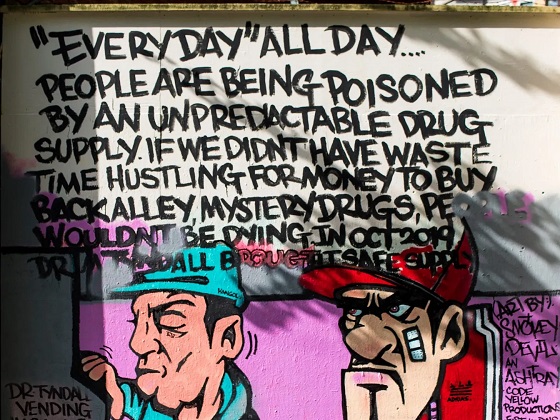
Study links B.C.’s drug policies to more overdoses, but researchers urge caution
By Alexandra Keeler
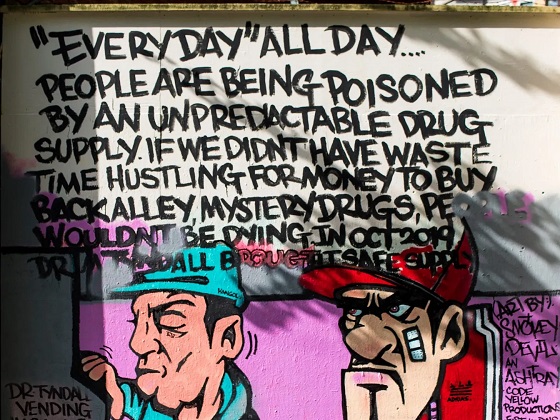
A study links B.C.’s safer supply and decriminalization to more opioid hospitalizations, but experts note its limitations
A new study says B.C.’s safer supply and decriminalization policies may have failed to reduce overdoses. Furthermore, the very policies designed to help drug users may have actually increased hospitalizations.
“Neither the safer opioid supply policy nor the decriminalization of drug possession appeared to mitigate the opioid crisis, and both were associated with an increase in opioid overdose hospitalizations,” the study says.
The study has sparked debate, with some pointing to it as proof that B.C.’s drug policies failed. Others have questioned the study’s methodology and conclusions.
“The question we want to know the answer to [but cannot] is how many opioid hospitalizations would have occurred had the policy not have been implemented,” said Michael Wallace, a biostatistician and associate professor at the University of Waterloo.
“We can never come up with truly definitive conclusions in cases such as this, no matter what data we have, short of being able to magically duplicate B.C.”
Jumping to conclusions
B.C.’s controversial safer supply policies provide drug users with prescription opioids as an alternative to toxic street drugs. Its decriminalization policy permitted drug users to possess otherwise illegal substances for personal use.
The peer-reviewed study was led by health economist Hai Nguyen and conducted by researchers from Memorial University in Newfoundland, the University of Manitoba and Weill Cornell Medicine, a medical school in New York City. It was published in the medical journal JAMA Health Forum on March 21.
The researchers used a statistical method to create a “synthetic” comparison group, since there is no ideal control group. The researchers then compared B.C. to other provinces to assess the impact of certain drug policies.
Examining data from 2016 to 2023, the study links B.C.’s safer supply policies to a 33 per cent rise in opioid hospitalizations.
The study says the province’s decriminalization policies further drove up hospitalizations by 58 per cent.
“Neither the safer supply policy nor the subsequent decriminalization of drug possession appeared to alleviate the opioid crisis,” the study concludes. “Instead, both were associated with an increase in opioid overdose hospitalizations.”
The B.C. government rolled back decriminalization in April 2024 in response to widespread concerns over public drug use. This February, the province also officially acknowledged that diversion of safer supply drugs does occur.
The study did not conclusively determine whether the increase in hospital visits was due to diverted safer supply opioids, the toxic illicit supply, or other factors.
“There was insufficient evidence to conclusively attribute an increase in opioid overdose deaths to these policy changes,” the study says.
Nguyen’s team had published an earlier, 2024 study in JAMA Internal Medicine that also linked safer supply to increased hospitalizations. However, it failed to control for key confounders such as employment rates and naloxone access. Their 2025 study better accounts for these variables using the synthetic comparison group method.
The study’s authors did not respond to Canadian Affairs’ requests for comment.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Correlation vs. causation
Chris Perlman, a health data and addiction expert at the University of Waterloo, says more studies are needed.
He believes the findings are weak, as they show correlation but not causation.
“The study provides a small signal that the rates of hospitalization have changed, but I wouldn’t conclude that it can be solely attributed to the safer supply and decrim[inalization] policy decisions,” said Perlman.
He also noted the rise in hospitalizations doesn’t necessarily mean more overdoses. Rather, more people may be reaching hospitals in time for treatment.
“Given that the [overdose] rate may have gone down, I wonder if we’re simply seeing an effect where more persons survive an overdose and actually receive treatment in hospital where they would have died in the pre-policy time period,” he said.
The Nguyen study acknowledges this possibility.
“The observed increase in opioid hospitalizations, without a corresponding increase in opioid deaths, may reflect greater willingness to seek medical assistance because decriminalization could reduce the stigma associated with drug use,” it says.
“However, it is also possible that reduced stigma and removal of criminal penalties facilitated the diversion of safer opioids, contributing to increased hospitalizations.”
Karen Urbanoski, an associate professor in the Public Health and Social Policy department at the University of Victoria, is more critical.
“The [study’s] findings do not warrant the conclusion that these policies are causally associated with increased hospitalization or overdose,” said Urbanoski, who also holds the Canada Research Chair in Substance Use, Addictions and Health Services.
Her team published a study in November 2023 that measured safer supply’s impact on mortality and acute care visits. It found safer supply opioids did reduce overdose deaths.
Critics, however, raised concerns that her study misrepresented its underlying data and showed no statistically significant reduction in deaths after accounting for confounding factors.
The Nguyen study differs from Urbanoski’s. While Urbanoski’s team focused on individual-level outcomes, the Nguyen study analyzed broader, population-level effects, including diversion.
Wallace, the biostatistician, agrees more individual-level data could strengthen analysis, but does not believe it undermines the study’s conclusions. Wallace thinks the researchers did their best with the available data they had.
“We do not have a ‘copy’ of B.C. where the policies weren’t implemented to compare with,” said Wallace.
B.C.’s overdose rate of 775 per 100,000 is well above the national average of 533.
Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, has been a vocal critic of B.C.’s decriminalization and safer supply policies.
“If the government doesn’t want to believe this study, well then I invite them to do a similar study,” she told reporters on March 27.
“Show us the evidence that they have failed to show us since 2020,” she added, referring to the year B.C. implemented safer supply.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Our content is always free – but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
-

 Business2 days ago
Business2 days agoIs Government Inflation Reporting Accurate?
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoWhen it comes to pipelines, Carney’s words flow both ways
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoStudy links B.C.’s drug policies to more overdoses, but researchers urge caution
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPolls say Canadians will give Trump what he wants, a Carney victory.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPoilievre’s Conservatives promise to repeal policy allowing male criminals in female jails
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCarney Liberals pledge to follow ‘gender-based goals analysis’ in all government policy
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoTrump Has Driven Canadians Crazy. This Is How Crazy.
-

 Entertainment1 day ago
Entertainment1 day agoPedro Pascal launches attack on J.K. Rowling over biological sex views