Health
Canadian patients face long waits for diagnostic imaging

From the Fraser Institute
Polling data from earlier this year is crystal clear—the majority Canadians believe their health-care system has worsened over the past decade and more money won’t fix the problem.
Who could blame them?
This year we’ve seen reports of the regular closing of emergency room services, studies finding that one in five Canadians are without access to a regular a family doctor, and that the country now boasts some of the longest waits for medically necessary surgery in 30 years.
It’s no secret that the rationing of care through long wait times has become the defining characteristic of Canadian health care. In fact, in 2023 Canadians could expect to wait a median of 27.7 weeks for treatment—nearly seven weeks longer than in 2019 and almost three times longer than the 9.3-week wait in 1993.
While bottlenecks can be found nearly everywhere throughout the system, less talked about are the increasingly lengthy waits Canadians face when trying to access timely diagnostic services.
In 2023, reported waits for an MRI were found to be a median of 12.9 weeks—two weeks longer than last year, and the longest on record in at least a decade. We see a similar thing for CT scans where the 6.6-week wait this year is a week longer than last year (and also the longest in at least a decade).
So why the lengthening delays?
One reason is that, when compared to other countries with universal coverage, Canada has some of the lowest availability of key diagnostic imaging technology in the industrialized world despite being one of the highest spenders among the same cohort.
Take CT scanners, for example. In 2019 (the latest year of available data), Canada ranked 26th (of 30 countries) for the number of scanners available. At 14.9 units per million population, this doesn’t even come close to the availability of this technology among top performers such as Japan, which reported having five-and-a-half times as many scanners. We see a similar story with MRI units, where Canada ranks 25th out of 29 countries and reports an availability of stock four times smaller than Japan’s. Canada also had middling to poor results for the volume of diagnostic examinations performed, ranking 13th of 26 for CT scans and 18th out of 26 for MRI exams per thousand population.
Ultimately, poor access to diagnostic imaging not only frustrates the timely triaging of patients, it can also potentially add onto already lengthy waits for scheduled treatment (which again are the longest in at least three decades).
Canadian patients face many challenges in seeking to access timely elective surgical care including lengthy waits for diagnostic services. Improving access to medical imaging is a first step towards improving this access.
Health
RFK Jr. Shuts Down Measles Scare in His First Network Interview as HHS Secretary

 The Vigilant Fox
The Vigilant Fox
CBS’s Jon LaPook tried to hype the measles panic, but Kennedy calmly dismantled the narrative and set the record straight.
The following is a streamlined and editorialized version of a thread that originally appeared on the American Values X page. It was edited and republished with permission. Click here to read the original thread.
HHS Secretary RFK Jr. recently set the record straight in an interview with CBS News’ chief medical correspondent, Dr. Jon LaPook. He pushed back on the claim that a second child had died from measles, exposing the narrative as not just misleading, but flat-out false.
But before that happened, Kennedy addressed the current measles outbreak and ongoing concerns about vaccine safety. He revealed that new safety trials are finally in motion.
“We don’t know the risks of many of these products,” he said. “They’re not adequately safety-tested.” He explained that “many of the vaccines are tested for only 3-4 days with NO placebo group.”
Kennedy made it clear this isn’t about banning vaccines—it’s about transparency. “I’ve always said … I’m not gonna take people’s vaccines away from them,” he said. “I’m gonna make sure that we have good science so that people can make an informed choice.” He added, “We are doing that science today.”
Kennedy was asked about Daisy Hildebrand, the young girl in Texas whose funeral he attended. Her death had been cited in headlines as proof of a growing measles crisis.
“It was very nice to be able to meet the parents in person and spend the whole day with them and share their lives with them and get to know their community,” he said. “The community was very welcoming and loving towards me.”
Kennedy described the experience warmly: “The Mennonite community was beautiful to me.” He added, “I went to a large lunch with the whole community and you had boys and girls sitting together and nobody was on a cell phone.”
That’s when Kennedy dropped the real bombshell: the child didn’t die from measles.
“The child whose funeral I attended this week was hospitalized three times from other illnesses,” he said. “She got measles and she got over the measles, according to her parents.” He added, “I saw the medical report on it today and the thing that killed her was not the measles, but it was a bacteriological infection.”
And it wasn’t the first time the media misled the public. Last month, another child’s death was falsely blamed on measles. But the truth is that it was a case of catastrophic medical error.
“Her death is the result of an egregious medical error,” CHD’s Mary Holland told Steve Bannon. “This girl wound up in the hospital because she did have some difficulty breathing, and instead of giving her breathing care, you’ll understand from the specialists with me that she got inaccurate, wrong-headed medical care, and that’s why she died.”
She added, “She did not die from measles. She died from a medical error, the third leading cause of death in this country.”
Thanks for reading. If you value the work being published here, upgrading your subscription is the most powerful way to support it. The more this Substack earns, the more we can expand the team, improve quality, and create the best reader experience possible.
For the full experience, upgrade your subscription.
Health
Red Deer Hospital Lottery – Previous Supporter Draw Deadline!

|
|
|
|
|
|
-

 Also Interesting2 days ago
Also Interesting2 days agoMortgage Mayhem: How Rising Interest Rates Are Squeezing Alberta Homeowners
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoConservative Party urges investigation into Carney plan to spend $1 billion on heat pumps
-

 Also Interesting2 days ago
Also Interesting2 days agoExploring Wildrobin Technological Advancements in Live Dealer Games
-
 2025 Federal Election2 days ago
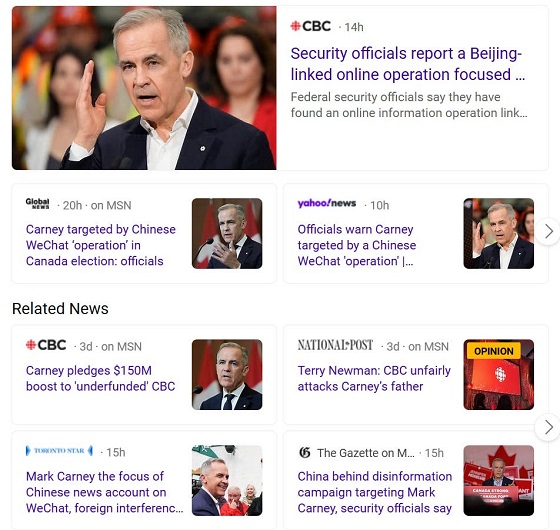
2025 Federal Election2 days agoCommunist China helped boost Mark Carney’s image on social media, election watchdog reports
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoFifty Shades of Mark Carney
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoCorporate Media Isn’t Reporting on Foreign Interference—It’s Covering for It
-

 Justice2 days ago
Justice2 days agoCanadian government sued for forcing women to share spaces with ‘transgender’ male prisoners
-

 Business1 day ago
Business1 day agoStocks soar after Trump suspends tariffs