Health
Canadian dentists desperate for details on federal dental care plan
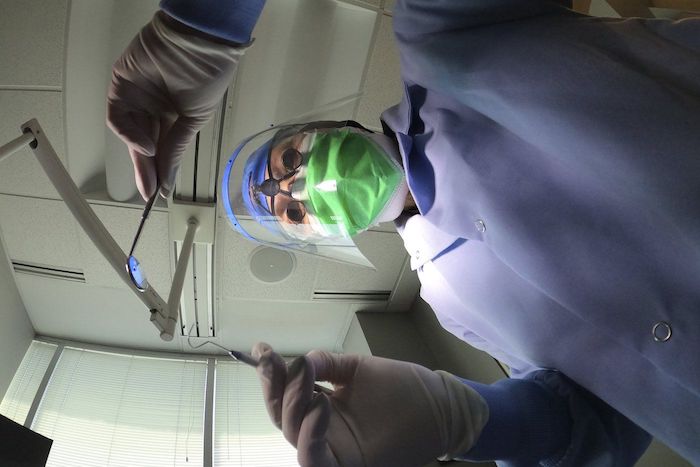
News release from Canada’s Provincial and Territorial Dental Associations
Canadian dentists to MPs: We need answers about the Canadian Dental Care Plan
Lack of consultation with provincial and territorial dental associations is worrying
There are only two months left before the Canadian Dental Care Plan (CDCP) becomes available to many more Canadians. Yet more than 25,000 dentists nationwide are in the dark about how the Government of Canada will safeguard access to dental care.
In a letter sent to Members of Parliament (MPs) this week, the presidents of provincial and territorial dental associations across the country asked how the government will:
- Safeguard employer-provided dental plans that two-thirds of Canadians currently have access to?
- Ensure that a strong federal program can be coordinated with existing provincial programs?
- Protect patient choice and maintain the patient-provider relationship?
- Ensure minimal, efficient administration that promotes timely access to care?
- Respect the costs of delivering dental care to maximize provider participation?
- Increase the number of dental assistants and dental hygienists to meet the demands of the CDCP?
Dentists want to champion a CDCP that will respect patients, providers, and taxpayers. The provincial and territorial dental associations are concerned that the CDCP has been compromised by a lack of meaningful consultation with dentists – who will be expected to deliver on the government’s promises.
The CDCP is currently in final planning stages, with a potential rollout in 2024 that will attempt to increase access to uninsured Canadians under 18, people with disabilities, and seniors who have an annual family income of less than $90,000. Dentists believe all Canadians need access to dental care. If not done properly, two-thirds of Canadians who have great employer-provided dental plans could lose their coverage and be forced into a worse plan. Costs would then skyrocket, which means the $13 billion over five years the government set aside would not be enough to sustain the plan.
Let’s take the time to get it right. We can increase access to dental care right now through an expansion of the interim measure already in place – the Canada Dental Benefit. This establishes a fixed dollar amount that a patient can use to be reimbursed for dental-related expenses.
Facts:
- Canada’s provincial and territorial dental associations represent more than 25,000 licensed dentists working in more than 16,000 offices. They treat more than 30 million Canadians every year and employ at least 50,0001 oral health care workers.
- Over 60 per cent of Canadians have a dentist they visit on a regular basis.2
- A recent survey commissioned by Health Canada found that nearly nine out 10 Canadians are satisfied with the Canada Dental Benefit.3
Quotes:
“To succeed, this plan needs to work for both patients and providers, and to work in each province. What we are recommending is based on decades of experience and caring for the oral health needs of the more than 30 million people that come into our dental offices across the country every year.” — Dr. Bruce Yaholnitsky, President, Alberta Dental Association
“Poorly designed programs do not improve access to care, and they leave the most vulnerable people in society behind. This is an historic opportunity, but only if the government gets it right. Dentists have the expertise, experience, and skills to know what it takes to ensure good oral and overall health.” — Dr. Rob Wolanski, President, British Columbia Dental Association
“As dentists we are excited to be a part of this Canadian dental care program, but there are key critical issues that need to be included for this program to be successful.” — Dr. Scott Leckie, President, Manitoba Dental Association
“New Brunswick dentists are already extremely busy with the recent spike in population and the backlog in demand for services related to Covid-19. This program was intended to provide dental care to the 35 per cent of Canadians who are uninsured. It needs to be easy to understand and to administer, and to be fair to all parties, including patients, dental care providers and taxpayers. Canadians need to know what benefits are being provided and which are not, before they arrive at the dental clinic.” — Dr. Joanah Campbell, President, New Brunswick Dental Society
“The new program must be sustainable in terms of funding, and easy to understand and access. It has to be patient-centred and work for everyone.” — Dr. Shane Roberts, President, Newfoundland & Labrador Dental Association
“While the CDCP has the potential to improve the lives of many Canadians, this can only be achieved if it’s done right. To ensure the greatest possible outcome, we must consider all of the moving pieces and take a patient-centred approach.” — Dr. Juli Waterbury, President, Nova Scotia Dental Association
“The CDCP could be a game-changer for Canadians’ access to dental care. But we have one chance to get it right. Here in Ontario, we have seen that dental care programs developed without the input of dentists are doomed to fail. Just look at the Ontario Seniors Dental Care Program, where waiting lists are up to two years long in some areas, and some patients have to travel ridiculously long distances to receive treatment.” — Dr. Brock Nicolucci, President, Ontario Dental Association
“This new program has the potential to improve access to care for many Canadians. It must be sustainable, patient-centred, and easy to access for patients. A poorly designed program will not improve access to care which is something we would like to avoid. We want this to work for Canadians.” — Dr. Derek Thiessen, President, College of Dental Surgeons of Saskatchewan
Addictions
Why B.C.’s new witnessed dosing guidelines are built to fail

Photo by Acceptable at English Wikipedia, ‘Two 1 mg pills of Hydromorphone, prescribed to me after surgery.’ [Licensed under CC BY-SA 3.0, via Wikimedia Commons]
By Alexandra Keeler
B.C. released new witnessed dosing guidelines for safer supply opioids. Experts say they are vague, loose and toothless
This February, B.C pledged to reintroduce witnessed dosing to its controversial safer supply program.
Safer supply programs provide prescription opioids to people who use drugs. Witnessed dosing requires patients to consume those prescribed opioids under the supervision of a health-care professional, rather than taking their drugs offsite.
The province said it was reintroducing witnessed dosing to “prevent the diversion of prescribed opioids and hold bad actors accountable.”
But experts are saying the government’s interim guidelines, released April 29, are fundamentally flawed.
“These guidelines — just as any guidelines for safer supply — do not align with addiction medicine best practices, period,” said Dr. Leonara Regenstreif, a primary care physician specializing in substance use disorders. Regenstreif is a founding member of Addiction Medicine Canada, an advocacy group that represents 23 addiction specialists.
Addiction physician Dr. Michael Lester, who is also a founding member of the group, goes further.
“Tweaking a treatment protocol that should not have been implemented in the first place without prior adequate study is not much of an advancement,” he said.
Witnessed dosing
Initially, B.C.’s safer supply program was generally administered through witnessed dosing. But in 2020, to facilitate access amidst pandemic restrictions, the province moved to “take-home dosing,” allowing patients to take their prescription opioids offsite.
After pandemic restrictions were lifted, the province did not initially return to witnessed dosing. Rather, it did so only recently, after a bombshell government report alleged more than 60 B.C. pharmacies were boosting sales by encouraging patients to fill unnecessary opioid prescriptions. This incentivized patients to sell their medications on the black market.
B.C.’s interim guidelines, developed by the BC Centre on Substance Use at the government’s request, now require all new safer supply patients to begin with witnessed dosing.
But for existing patients, the guidelines say prescribers have discretion to determine whether to require witnessed dosing. The guidelines define an existing patient as someone who was dispensed prescription opioids within the past 30 days.
The guidelines say exemptions to witnessed dosing are permitted under “extraordinary circumstances,” where witnessed dosing could destabilize the patient or where a prescriber uses “best clinical judgment” and determines diversion risk is “very low.”
Holes
Clinicians say the guidelines are deliberately vague.
Regenstreif described them as “wordy, deliberately confusing.” They enable prescribers to carry on as before, she says.
Lester agrees. Prescribers would be in compliance with these guidelines even if “none of their patients are transferred to witnessed dosing,” he said.
In his view, the guidelines will fail to meet their goal of curbing diversion.
And without witnessed dosing, diversion is nearly impossible to detect. “A patient can take one dose a day and sell seven — and this would be impossible to detect through urine testing,” Lester said.
He also says the guidelines do not remove the incentive for patients to sell their drugs to others. He cites estimates from Addiction Medicine Canada that clients can earn up to $20,000 annually by selling part of their prescribed supply.
“[Prescribed safer supply] can function as a form of basic income — except that the community is being flooded with addictive and dangerous opioids,” Lester said.
Regenstreif warns that patients who had been diverting may now receive unnecessarily high doses. “Now you’re going to give people a high dose of opioids who don’t take opioids,” she said.
She also says the guidelines leave out important details on adjusting doses for patients who do shift from take-home to witnessed dosing.
“If a doctor followed [the guidelines] to the word, and the patient followed it to the word, the patient would go into withdrawal,” she said.
The guidelines assume patients will swallow their pills under supervision, but many crush and inject them instead, Regenstreif says. Because swallowing is less potent, a higher dose may be needed.
“None of that is accounted for in this document,” she said.
Survival strategy
Some harm reduction advocates oppose a return to witnessed dosing, saying it will deter people from accessing a regulated drug supply.
Some also view diversion as a life-saving practice.
Diversion is “a harm reduction practice rooted in mutual aid,” says a 2022 document developed by the National Safer Supply Community of Practice, a group of clinicians and harm reduction advocates.
The group supports take-home dosing as part of a broader strategy to improve access to safer supply medications. In their document, they say barriers to accessing safer supply programs necessitate diversion among people who use drugs — and that the benefits of diversion outweigh the risks.
However, the risks — and harms — of diversion are mounting.
People can quickly develop a tolerance to “safer” opioids and then transition to more dangerous substances. Some B.C. teenagers have said the prescription opioid Dilaudid was a stepping stone to them using fentanyl. In some cases, diversion of these drugs has led to fatal overdoses.
More recently, a Nanaimo man was sentenced to prison for running a highly organized drug operation that trafficked diverted safer supply opioids. He exchanged fentanyl and other illicit drugs for prescription pills obtained from participants in B.C.’s safer supply program.
Recovery
Lester, of Addiction Medicine Canada, believes clinical discretion has gone too far. He says take-home dosing should be eliminated.
“Best practices in addiction medicine assume physicians prescribing is based on sound and thorough research, and ensuring that their prescribing does not cause harm to the broader community, as well as the patient,” he said.
“[Safer supply] for opioids fails in both these regards.”
He also says safer supply should only be offered as a short-term bridge to patients being started on proven treatments like buprenorphine or methadone, which help reduce drug cravings and manage withdrawal symptoms.
B.C.’s witnessed dosing guidelines say prescribers can discuss such treatment options with patients. However, the guidelines remain neutral on whether safer supply is intended as a transitional step toward longer-term treatment.
Regenstreif says this neutrality undermines care.
“[M]ost patients I’ve seen with opioid use disorder don’t want to have [this disorder],” she said. “They would rather be able to set goals and do other things.”
Oversight gaps
Currently, about 3,900 people in B.C. participate in the safer supply program — down from 5,200 in March 2023.
The B.C. government has not provided data on how many have been transitioned to witnessed dosing. Investigative journalist Rob Shaw recently reported that these data do not exist.
“The government … confirmed recently they don’t have any mechanism to track which ‘safe supply’ participants are witnessed and which [are] not,” said Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, who has been a vocal critic of safer supply.
“Without a public report and accountability there can be no confidence.”
The BC Centre on Substance Use, which developed the interim guidelines, says it does not oversee policy decisions or data tracking. It referred Canadian Affairs’ questions to B.C.’s Ministry of Health, which has yet to clarify whether it will track and publish transition data. The ministry did not respond to requests for comment by deadline.
B.C. has also not indicated when or whether it will release final guidelines.
Regenstreif says the flawed guidelines mean many people may be misinformed, discouraged or unsupported when trying to reduce their drug use and recover.
“We’re not listening to people with lived experience of recovery,” she said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
Addictions
‘Over and over until they die’: Drug crisis pushes first responders to the brink

First responders say it is not overdoses that leave them feeling burned out—it is the endless cycle of calls they cannot meaningfully resolve
The soap bottle just missed his head.
Standing in the doorway of a cluttered Halifax apartment, Derek, a primary care paramedic, watched it smash against the wall.
Derek was there because the woman who threw it had called 911 again — she did so nearly every day. She said she had chest pain. But when she saw the green patch on his uniform, she erupted. Green meant he could not give her what she wanted: fentanyl.
She screamed at him to call “the red tags” — advanced care paramedics authorized to administer opioids. With none available, Derek declared the scene unsafe and left. Later that night, she called again. This time, a red-patched unit was available. She got her dose.
Derek says he was not angry at the woman, but at the system that left her trapped in addiction — and him powerless to help.
First responders across Canada say it is not overdoses that leave them feeling burned out — it is the endless cycle of calls they cannot meaningfully resolve. Understaffed, overburdened and dispatched into crises they are not equipped to fix, many feel morally and emotionally drained.
“We’re sending our first responders to try and manage what should otherwise be dealt with at structural and systemic levels,” said Nicholas Carleton, a University of Regina researcher who studies the mental health of public safety personnel.
Canadian Affairs agreed to use pseudonyms for the two frontline workers referenced in this story. Canadian Affairs also spoke with nine other first responders who agreed to speak only on background. All of these sources cited concerns about workplace retaliation for speaking out.
Moral injury
Canada’s opioid crisis is pushing frontline workers such as paramedics to the brink.
A 2024 study of 350 Quebec paramedics shows one in three have seriously considered suicide. Globally, ambulance workers have among the highest suicide rates of public service personnel.
Between 2017 and 2024, Canadian paramedics responded to nearly 240,000 suspected opioid overdoses. More than 50,000 of those were fatal.
Yet many paramedics say overdose calls are not the hardest part of the job.
“When they do come up, they’re pretty easy calls,” said Derek. Naloxone, a drug that reverses overdoses, is readily available. “I can actually fix the problem,” he said. “[It’s a] bit of instant gratification, honestly.”
What drains him are the calls they cannot fix: mental health crises, child neglect and abuse, homelessness.
“The ER has a [cardiac catheterization] lab that can do surgery in minutes to fix a heart attack. But there’s nowhere I can bring the mental health patients.
“So they call. And they call. And they call.”
Thomas, a primary care paramedic in Eastern Ontario, echoes that frustration.
“The ER isn’t a good place to treat addiction,” he said. “They need intensive, long-term psychological inpatient treatment and a healthy environment and support system — first responders cannot offer that.”
That powerlessness erodes trust. Paramedics say patients with addictions often become aggressive, or stop seeking help altogether.
“We have a terrible relationship with the people in our community struggling with addiction,” Thomas said. “They know they will sit in an ER bed for a few hours while being in withdrawals and then be discharged with a waitlist or no follow-up.”
Carleton, of the University of Regina, says that reviving people repeatedly without improvement decreases morale.
“You’re resuscitating someone time and time again,” said Carleton, who is also director of the Psychological Trauma and Stress Systems Lab, a federal unit dedicated to mental health research for public safety personnel. “That can lead to compassion fatigue … and moral injury.”
Katy Kamkar, a clinical psychologist focused on first responder mental health, says moral injury arises when workers are trapped in ethically impossible situations — saving a life while knowing that person will be back in the same state tomorrow.
“Burnout is … emotional exhaustion, depersonalization, and reduced personal accomplishment,” she said in an emailed statement. “High call volumes, lack of support or follow-up care for patients, and/or bureaucratic constraints … can increase the risk of reduced empathy, absenteeism and increased turnover.”
Kamkar says moral injury affects all branches of public safety, not just paramedics. Firefighters, who are often the first to arrive on the scene, face trauma from overdose deaths. Police report distress enforcing laws that criminalize suffering.
Understaffed and overburdened
Staffing shortages are another major stressor.
“First responders were amazing during the pandemic, but it also caused a lot of fatigue, and a lot of people left our business because of stress and violence,” said Marc-André Périard, vice president of the Paramedic Chiefs of Canada.
Nearly half of emergency medical services workers experience daily “Code Blacks,” where there are no ambulances available. Vacancy rates are climbing across emergency services. The federal government predicts paramedic shortages will persist over the coming decade, alongside moderate shortages of police and firefighters.
Unsafe work conditions are another concern. Responders enter chaotic scenes where bystanders — often fellow drug users — mistake them for police. Paramedics can face hostility from patients they just saved, says Périard.
“People are upset that they’ve been taken out of their high [when Naloxone is administered] and not realizing how close to dying they were,” he said.
Thomas says safety is undermined by vague, inconsistently enforced policies. And efforts to collect meaningful data can be hampered by a work culture that punishes reporting workplace dangers.
“If you report violence, it can come back to haunt you in performance reviews” he said.
Some hesitate to wait for police before entering volatile scenes, fearing delayed response times.
“[What] would help mitigate violence is to have management support their staff directly in … waiting for police before arriving at the scene, support paramedics in leaving an unsafe scene … and for police and the Crown to pursue cases of violence against health-care workers,” Thomas said.
“Right now, the onus is on us … [but once you enter], leaving a scene is considered patient abandonment,” he said.
Upstream solutions
Carleton says paramedics’ ability to refer patients to addiction and mental health referral networks varies widely based on their location. These networks rely on inconsistent local staffing, creating a patchwork system where people easily fall through the cracks.
“[Any] referral system butts up really quickly against the challenges our health-care system is facing,” he said. “Those infrastructures simply don’t exist at the size and scale that we need.”
Périard agrees. “There’s a lot of investment in safe injection sites, but not as much [resources] put into help[ing] these people deal with their addictions,” he said.
Until that changes, the cycle will continue.
On May 8, Alberta renewed a $1.5 million grant to support first responders’ mental health. Carleton welcomes the funding, but says it risks being futile without also addressing understaffing, excessive workloads and unsafe conditions.
“I applaud Alberta’s investment. But there need to be guardrails and protections in place, because some programs should be quickly dismissed as ineffective — but they aren’t always,” he said.
Carleton’s research found that fewer than 10 mental health programs marketed to Canadian governments — out of 300 in total — are backed up by evidence showing their effectiveness.
In his view, the answer is not complicated — but enormous.
“We’ve got to get way further upstream,” he said.
“We’re rapidly approaching more and more crisis-level challenges… with fewer and fewer [first responders], and we’re asking them to do more and more.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
-

 Fraser Institute1 day ago
Fraser Institute1 day agoBefore Trudeau average annual immigration was 617,800. Under Trudeau number skyrocketted to 1.4 million annually
-

 MAiD1 day ago
MAiD1 day agoCanada’s euthanasia regime is already killing the disabled. It’s about to get worse
-
 Frontier Centre for Public Policy1 day ago
Frontier Centre for Public Policy1 day agoNew Book Warns The Decline In Marriage Comes At A High Cost
-

 Business1 day ago
Business1 day agoPrime minister can make good on campaign promise by reforming Canada Health Act
-

 Addictions1 day ago
Addictions1 day ago‘Over and over until they die’: Drug crisis pushes first responders to the brink
-

 International1 day ago
International1 day agoChicago suburb purchases childhood home of Pope Leo XIV
-

 Daily Caller1 day ago
Daily Caller1 day agoUSAID Quietly Sent Thousands Of Viruses To Chinese Military-Linked Biolab
-

 Energy1 day ago
Energy1 day agoLNG Export Marks Beginning Of Canadian Energy Independence




