Health
US FDA plans overhaul of decades-old medical device system
WASHINGTON — US health officials say they plan to overhaul the country’s decades-old system for approving most medical devices, which experts have long criticized for failing to catch problems with risky implants and medical instruments.
The Food and Drug Administration announced plans Monday aimed at making sure new medical devices reflect up-to-date safety and effectiveness features. The system targeted by the actions generally allows manufacturers to launch new products based on similarities to decades-old products, not new clinical testing.
The FDA’s pledge came one day after the publication of a global investigation into medical device safety by more than 50 media organizations, including The Associated Press. The probe, led by the International Consortium of Investigative Journalists, analyzed more than 8 million device-related health records, including death and injury reports and recalls.
Matthew Perrone, The Associated Press
Health
WHO member states agree on draft of ‘pandemic treaty’ that could be adopted in May

From LifeSiteNews
The WHO draft ‘pandemic accord’ includes data sharing between governments and pharmaceutical companies to develop ‘pandemic-related health products,’ though it would not apply to the US.
Representatives of WHO member states have agreed on a draft of the “pandemic accord” that is scheduled to be voted on next month.
“The nations of the world made history in Geneva today,” Dr. Tedros Adhanom Ghebreyesus, Director-General of the WHO, said after the member states agreed on the draft of the pandemic treaty on Wednesday.
“In reaching consensus on the Pandemic Agreement, not only did they put in place a generational accord to make the world safer, they have also demonstrated that multilateralism is alive and well, and that in our divided world, nations can still work together to find common ground, and a shared response to shared threats. I thank WHO’s Member States, and their negotiating teams, for their foresight, commitment and tireless work. We look forward to the World Health Assembly’s consideration of the agreement and – we hope – its adoption,” the WHO leader continued.
The agreement was reached by the Intergovernmental Negotiating Body (INB), the committee set up by the WHO to negotiate the treaty, after more than three years of negotiations.
According to the WHO’s press release, the core pandemic treaty draft includes the establishment of “a pathogen access and benefit sharing system,” allowing the sharing of data between governments and pharmaceutical companies aimed at quickly developing and supplying “pandemic-related health products” during a pandemic. These “health products” could be dangerous mRNA injections, similar to those rolled out and imposed on large parts of the world population during the COVID-19 crisis.
The WHO claims that the “proposal affirms the sovereignty of countries to address public health matters within their borders, and provides that nothing in the draft agreement shall be interpreted as providing WHO any authority to direct, order, alter or prescribe national laws or policies, or mandate States to take specific actions, such as ban or accept travellers, impose vaccination mandates or therapeutic or diagnostic measures or implement lockdowns.”
The WHO seems to be responding to critics of the Pandemic Treaty, who have argued it is a power grab by the WHO. It would give the global organization unchecked power whenever it declares that any health risk is a “pandemic.” However, the new draft has not yet been made public, making a thorough assessment impossible.
WHO director-general Ghebreyesus engaged in his typical fear-mongering, stating, “Virus is the worst enemy. (It) could be worse than a war.”
READ: WHO director Tedros calls for ‘more aggressive’ action against COVID shot critics
While the WHO pandemic treaty and the amendments to the International Health Regulations (IHR) failed to pass last year, the new version of the agreement could be passed by a two-thirds majority at the annual World Health Assembly (May 19-27, 2025) next month.
However, the U.S. was not part of the negotiations and would not be bound by the agreement since President Donald Trump withdrew the country from the international body in January 2025 after taking office for his second term. Argentine President Javier Milei announced in February that his country will also leave the WHO, following Trump’s example. If more countries were to leave the WHO, the pandemic agreement could be ineffective in practice, even if it were to pass in May.
Autism
RFK Jr. Exposes a Chilling New Autism Reality
 The Vigilant Fox
The Vigilant Fox
Autism rates are exploding. The “experts” say they’re clueless. But Kennedy believes he knows exactly where to look.
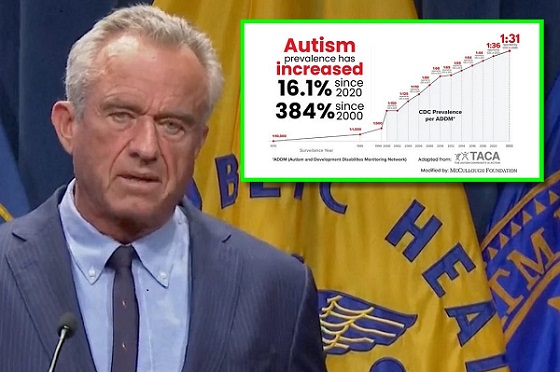
HHS Secretary RFK Jr. just held a press conference to respond to the CDC’s latest numbers on autism rates in the United States.
The findings were impossible to ignore, and Kennedy didn’t sugarcoat just how dire the situation had become.
He revealed that 1 in 31 American children are now diagnosed with autism.
For boys, the numbers are even worse—1 in 20.
And in California, where data tracking is considered the most thorough in the country, the rate may be as high as 1 in 12.5 boys. According to Kennedy, that figure likely reflects a national trend.
Just two years ago, the national rate was 1 in 36. Now, it’s jumped dramatically—and Kennedy says he’s determined to find out why.
“The ASD prevalence rate in 8-year-olds is now 1 in 31. Shocking. There is an extreme risk for boys. Overall, the risk for boys of getting an autism diagnosis in this country is now 1 in 20.
“And as high in California, which has the best data collection.
“So it probably also reflects the national trend—1 in 12.5 boys. This is part of an unrelenting upward trend. The prevalence two years ago was 1 in 36,” Kennedy lamented.
He didn’t hold back in calling out the media and powerful industries, accusing them of covering up environmental factors that are contributing to the crisis.
Kennedy blasted the “epidemic denialists,” pointing to a 1992 ADDM report as proof that autism rates have exploded nearly fivefold in just three decades. Back then, the rate was 1 in 150. Today, it’s 1 in 31.
“It’s clear that the rates are real,” Kennedy stressed.
“Year by year there is a steady, relentless increase. I want it because this epidemic denial has become a feature in the mainstream media and it’s based on an industry canard.
“Obviously there are people who don’t want us to look at environmental exposures,” he said.
He also took direct aim at the claim that today’s rising autism rates are simply the result of better awareness or improved diagnosis.
To prove his point, Kennedy cited a peer-reviewed 1987 study from North Dakota, where researchers attempted to identify every child in the state with a developmental disorder.
They didn’t cut corners. They analyzed medical records, confirmed diagnoses, and even conducted in-person evaluations across a population of 180,000 children. Then, they followed that same group for 12 years.
If you still believe autism rates are only rising because doctors are “getting better at diagnosing it,” Kennedy said, you’d have to believe that the original researchers somehow missed nearly all the cases—98.8 percent of them.
But that’s not what happened.
“They went back in 2000 and found that they had missed exactly one child,” he said.
“They weren’t missing all these cases. The epidemic is real.”
Then came one of the most infuriating parts of the press conference: Kennedy revealed how autism research funding has been misdirected for years.
He said the National Institutes of Health (NIH) has pumped 10 to 20 times more money into studying genetic causes of autism than into researching environmental ones.
That, Kennedy said, is a dead end.
“This is a preventable disease. We know it’s an environmental exposure. It has to be. Genes do not cause epidemics,” he argued.
That’s why Kennedy says he’s redirecting resources toward the kind of research that’s long been neglected—into environmental factors.
“And that’s where we’re going to find the answer,” he added.
The most emotional moment came at the end, when Kennedy spoke from the heart about what this epidemic is doing to children—and to families.
“These are children who should not be suffering like this,” he said.
“These are kids who, many of them, were fully functional and regressed because of some environmental exposure into autism when they’re two years old. These are kids who will never pay taxes, they’ll never hold a job, they’ll never play baseball, they’ll never write a poem, they’ll never go out on a date.
Many of them will never use a toilet unassisted.”
“We have to recognize we are doing this to our children and we need to put an end to it,” Kennedy declared.
Thanks for reading! This post took time and care to put together, and I did my best to give this story the coverage it deserved.
If you like my work and want to support me and my family and help keep this page going strong,
the most powerful thing you can do is sign up for the email list and become a paid subscriber.
Your monthly subscription goes further than you think. Thank you so much for your support.
A little bit about me: I spent over a decade working as a licensed healthcare professional. But when the Biden administration rolled out its vaccine mandates, I couldn’t stay silent. My conscience simply wouldn’t let me.
That’s when I started this page.
Since then, I’ve shared thousands of clips featuring doctors and scientists who were brave enough to question the official COVID narrative. Along the way, we’ve reached billions of views and helped millions of people see the side of the story the government didn’t want out.
These days, I’m going even deeper—breaking down interviews with dissenting experts and revisiting forgotten science to uncover what you haven’t been told about cancer, cholesterol, fasting, sunlight, and more.
If you’re looking for clear, honest information without corporate spin, you’re in the right place. Follow me for straight-to-the-point clips and threads that challenge the narrative—featuring credible experts you rarely hear from in the mainstream.
Follow on 𝕏: @VigilantFox
Telegram: t.me/VigilantFox
Rumble: rumble.com/c/VigilantFox
Email List: vigilantfox.com
The Vigilant Fox is a reader-supported Substack publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Invite your friends and earn rewards
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoRCMP Whistleblowers Accuse Members of Mark Carney’s Inner Circle of Security Breaches and Surveillance
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoMEI-Ipsos poll: 56 per cent of Canadians support increasing access to non-governmental healthcare providers
-

 Health2 days ago
Health2 days agoTrump admin directs NIH to study ‘regret and detransition’ after chemical, surgical gender transitioning
-
 Business8 hours ago
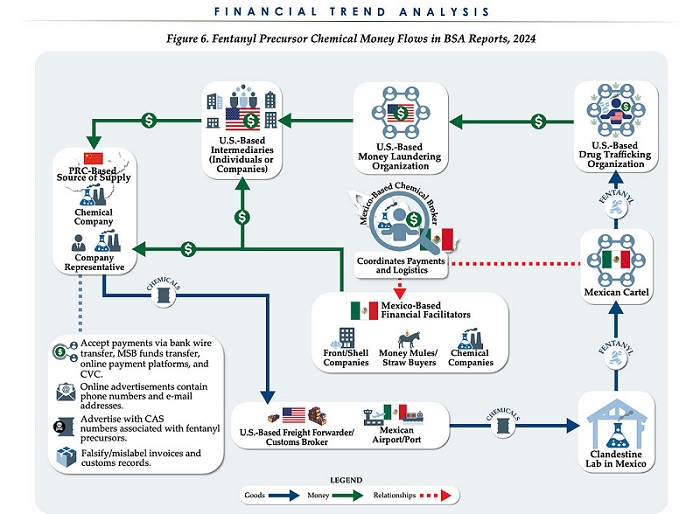
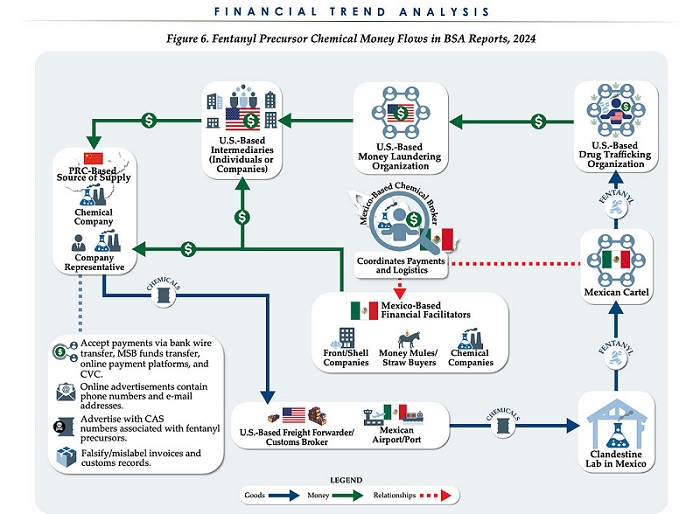
Business8 hours agoChina, Mexico, Canada Flagged in $1.4 Billion Fentanyl Trade by U.S. Financial Watchdog
-

 Daily Caller6 hours ago
Daily Caller6 hours agoTrump Executive Orders ensure ‘Beautiful Clean’ Affordable Coal will continue to bolster US energy grid
-
 2025 Federal Election17 hours ago
2025 Federal Election17 hours agoTucker Carlson Interviews Maxime Bernier: Trump’s Tariffs, Mass Immigration, and the Oncoming Canadian Revolution
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoBureau Exclusive: Chinese Election Interference Network Tied to Senate Breach Investigation
-

 Autism2 days ago
Autism2 days agoAutism Rates Reach Unprecedented Highs: 1 in 12 Boys at Age 4 in California, 1 in 31 Nationally