Health
Top Canadian psychiatrists urge gov’t to halt expansion of euthanasia to the mentally ill

From LifeSiteNews
Dr. Sonu Gaind, chief of psychiatry at Sunnybrook Health Sciences Centre in Toronto, said history shows that when enacting new laws relating to sensitive life matters, ‘The evidence shows that we are right less than half the time.’
Top Canadian psychiatrists warned that the country is “not ready” for the coming expansion of euthanasia to those who are mentally ill, saying expanding the procedure is not something “society should be doing” as it could lead to deaths under a “false pretense.”
As noted in a recent National Post opinion piece, seven of 17 chairs of psychiatry have written to Canadian Health Minister Mark Holland and Justice Minister Arif Virani to demand that the federal government of Prime Minister Justin Trudeau pause the expansion of medical assistance in dying (MAiD) as it is known.
On March 9, 2024, euthanasia in Canada, or MAiD as it is known, will expand to include those suffering solely from mental illness. This is a result of the 2021 passage of Bill C-7, which also allowed the chronically ill – not just the terminally ill – to qualify for so-called doctor-assisted death.
The mental illness expansion was originally set to take effect in March. However, after massive pushback from pro-life groups, conservative politicians and others, the Liberals under Trudeau delayed the introduction of the full effect of Bill C-7 until 2024 via Bill C-39, which becomes law next year.
Dr. Sonu Gaind, who works as the chief of psychiatry at Sunnybrook Health Sciences Centre in Toronto, said that history shows when it comes to enacting new laws relating to sensitive life matters, “The evidence shows that we are right less than half the time.”
Proponents of MAiD have argued that there comes a point in time when a mentally ill individual is simply not curable. However, Gaind said that the notion of “incurability” might not even be possible.
Gaind said that as the evidence shows being wrong half the time, “That means that at least half the people who assessors say, ‘You’re not going to get better from your mental illness, and you can get MAID,’ at least half of those people would have gotten better.”
“Meaning, we would have provided death under a false pretence,” he added.
Gaind said there seems to be “no consensus on this issue,” and said he “firmly” thinks “we’re not ready for further expansion.”
As it stands now, a special joint parliamentary committee on MAID has reconvened to investigate the looming expansion of MAiD to the mentally ill.
Recently, LifeSiteNews reported on how pro-euthanasia lobbyists want Canada’s assisted suicide via lethal injection laws to be extended to drug addicts, which critics warn could lead the nation down a dangerous path nearing “eugenics.”
The delay in expanding MAiD until 2024 also came after numerous public scandals, including the surfacing of reports that Canadian veterans were being offered the fatal procedure by workers at Veterans Affairs Canada (VAC).
Offering MAiD to the mentally ill is not something ‘society should be doing,’ psychiatrist says
Dr. Jitender Sareen, head of the Department of Psychiatry at the University of Manitoba, said that when it comes to MAiD, there is too much left in the hands of those who do the procedure.
“Offering people death instead of appropriate treatments” is something that “really goes against what we as a society should be doing,” Sareen said as per the National Post.
Sareen also said there is no guidance as to whether a doctor can determine whether a person is suicidal or simply wants to kill themselves via MAiD.
Recent attempts by the Conservative Party of Canada (CPC) to stop the expansion of MAiD have failed.
MPs in the House of Commons voted down a private members’ bill introduced by CPC MP Ed Fast that would have repealed the expansion of euthanasia laws to those suffering from mental illness.
Pro-life advocates, such as Angelina Ireland, president of the Delta Hospice Society (DHS), have warned the Trudeau government expansion of MAiD to those who are mentally ill will lead to allowing “MAiD allows agents of the state to kill us and it’s actually called ‘non-culpable homicide.’”
Ireland recently told LifeSiteNews that it was important she made clear to participants who attended to “speak to some inconvenient truths” about just how bad MAiD is for Canada.
“There is no avenue for us to ‘sue’ them (the government) or charge them with murder. We have abdicated our power and given the government the supreme authority — the right and the privilege to murder us,” Ireland said to LifeSiteNews, which she also told the event participants.
Euthanasia deaths have gone through the roof in Canada since it became legal in 2016.
According to Health Canada, in 2022, 13,241 Canadians died by MAiD lethal injection, which is 4.1% of all deaths in the country for that year, and a 31.2% increase from 2021.
The number of Canadians killed by lethal injection since 2016 now stands at 44,958.
armed forces
Yet another struggling soldier says Veteran Affairs Canada offered him euthanasia

From LifeSiteNews
‘It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself.’
Yet another Canadian combat veteran has come forward to reveal that when he sought help, he was instead offered euthanasia.
David Baltzer, who served two tours in Afghanistan with the Princess Patricia’s Canadian Light Infantry, revealed to the Toronto Sun that he was offered euthanasia on December 23, 2019—making him, as the Sun noted, “among the first Canadian soldiers offered therapeutic suicide by the federal government.”
Baltzer had been having a disagreement with his existing caseworker, when assisted suicide was brought up in in call with a different agent from Veteran Affairs Canada.
“It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself,” Baltzer told the Sun.“I was in my lowest down point, it was just before Christmas. He says to me, ‘I would like to make a suggestion for you. Keep an open mind, think about it, you’ve tried all this and nothing seems to be working, but have you thought about medical-assisted suicide?’”
Baltzer was stunned. “It just seems to me that they just want us to be like ‘f–k this, I give up, this sucks, I’d rather just take my own life,’” he said. “That’s how I honestly felt.”
Baltzer, who is from St. Catharines, Ontario, joined up at age 17, and moved to Manitoba to join the Princess Patricia’s Canadian Light Infantry, one of Canada’s elite units. He headed to Afghanistan in 2006. The Sun noted that he “was among Canada’s first troops deployed to Afghanistan as part Operation Athena, where he served two tours and saw plenty of combat.”
“We went out on long-range patrols trying to find the Taliban, and that’s exactly what we did,” Baltzer said. “The best way I can describe it, it was like Black Hawk Down — all of the sudden the s–t hit the fan and I was like ‘wow, we’re fighting, who would have thought? Canada hasn’t fought like this since the Korean War.”
After returning from Afghanistan, Baltzer says he was offered counselling by Veteran Affairs Canada, but it “was of little help,” and he began to self-medicate for his trauma through substance abuse (he noted that he is, thankfully, doing well today). Baltzer’s story is part of a growing scandal. As the Sun reported:
A key figure shedding light on the VAC MAID scandal was CAF veteran Mark Meincke, whose trauma-recovery podcast Operation Tango Romeo broke the story. ‘Veterans, especially combat veterans, usually don’t reach out for help until like a year longer than they should’ve,’ Meincke said, telling the Sun he waited over two decades before seeking help.
‘We’re desperate by the time we put our hands up for help. Offering MAID is like throwing a cinderblock instead of a life preserver.’ Meincke said Baltzer’s story shoots down VAC’s assertions blaming one caseworker for offering MAID to veterans, and suggests the problem is far more serious than some rogue public servant.
‘It had to have been policy. because it’s just too many people in too many provinces,” Meincke told the Sun. “Every province has service agents from that province.’
Veterans Affairs Canada claimed in 2022 that between four and 20 veterans had been offered assisted suicide; Meincke “personally knows of five, and said the actual number’s likely close to 20.” In a previous investigation, VAC claimed that only one caseworker was responsible—at least for the four confirmed cases—and that the person “was lo longer employed with VAC.” Baltzer says VAC should have military vets as caseworkers, rather than civilians who can’t understand what vets have been through.
To date, no federal party leader has referenced Canada’s ongoing euthanasia scandals during the 2025 election campaign.
2025 Federal Election
Study links B.C.’s drug policies to more overdoses, but researchers urge caution
By Alexandra Keeler
A study links B.C.’s safer supply and decriminalization to more opioid hospitalizations, but experts note its limitations
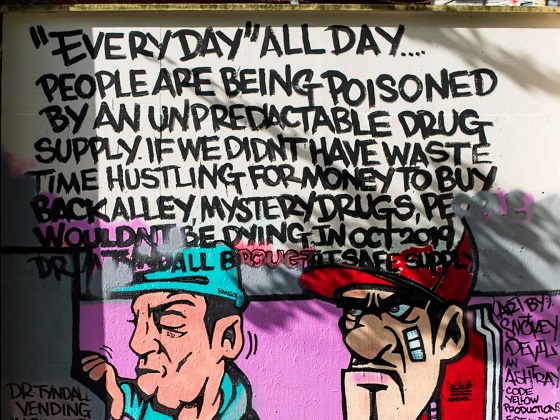
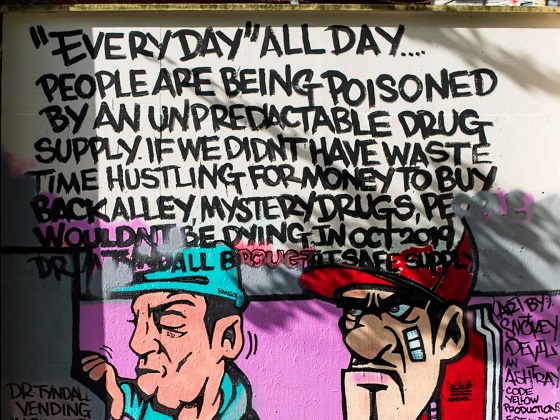
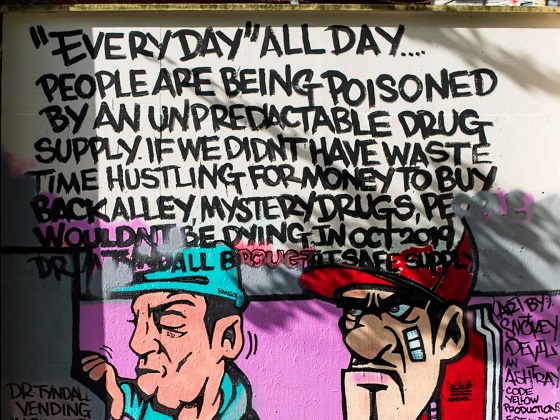
A new study says B.C.’s safer supply and decriminalization policies may have failed to reduce overdoses. Furthermore, the very policies designed to help drug users may have actually increased hospitalizations.
“Neither the safer opioid supply policy nor the decriminalization of drug possession appeared to mitigate the opioid crisis, and both were associated with an increase in opioid overdose hospitalizations,” the study says.
The study has sparked debate, with some pointing to it as proof that B.C.’s drug policies failed. Others have questioned the study’s methodology and conclusions.
“The question we want to know the answer to [but cannot] is how many opioid hospitalizations would have occurred had the policy not have been implemented,” said Michael Wallace, a biostatistician and associate professor at the University of Waterloo.
“We can never come up with truly definitive conclusions in cases such as this, no matter what data we have, short of being able to magically duplicate B.C.”
Jumping to conclusions
B.C.’s controversial safer supply policies provide drug users with prescription opioids as an alternative to toxic street drugs. Its decriminalization policy permitted drug users to possess otherwise illegal substances for personal use.
The peer-reviewed study was led by health economist Hai Nguyen and conducted by researchers from Memorial University in Newfoundland, the University of Manitoba and Weill Cornell Medicine, a medical school in New York City. It was published in the medical journal JAMA Health Forum on March 21.
The researchers used a statistical method to create a “synthetic” comparison group, since there is no ideal control group. The researchers then compared B.C. to other provinces to assess the impact of certain drug policies.
Examining data from 2016 to 2023, the study links B.C.’s safer supply policies to a 33 per cent rise in opioid hospitalizations.
The study says the province’s decriminalization policies further drove up hospitalizations by 58 per cent.
“Neither the safer supply policy nor the subsequent decriminalization of drug possession appeared to alleviate the opioid crisis,” the study concludes. “Instead, both were associated with an increase in opioid overdose hospitalizations.”
The B.C. government rolled back decriminalization in April 2024 in response to widespread concerns over public drug use. This February, the province also officially acknowledged that diversion of safer supply drugs does occur.
The study did not conclusively determine whether the increase in hospital visits was due to diverted safer supply opioids, the toxic illicit supply, or other factors.
“There was insufficient evidence to conclusively attribute an increase in opioid overdose deaths to these policy changes,” the study says.
Nguyen’s team had published an earlier, 2024 study in JAMA Internal Medicine that also linked safer supply to increased hospitalizations. However, it failed to control for key confounders such as employment rates and naloxone access. Their 2025 study better accounts for these variables using the synthetic comparison group method.
The study’s authors did not respond to Canadian Affairs’ requests for comment.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Correlation vs. causation
Chris Perlman, a health data and addiction expert at the University of Waterloo, says more studies are needed.
He believes the findings are weak, as they show correlation but not causation.
“The study provides a small signal that the rates of hospitalization have changed, but I wouldn’t conclude that it can be solely attributed to the safer supply and decrim[inalization] policy decisions,” said Perlman.
He also noted the rise in hospitalizations doesn’t necessarily mean more overdoses. Rather, more people may be reaching hospitals in time for treatment.
“Given that the [overdose] rate may have gone down, I wonder if we’re simply seeing an effect where more persons survive an overdose and actually receive treatment in hospital where they would have died in the pre-policy time period,” he said.
The Nguyen study acknowledges this possibility.
“The observed increase in opioid hospitalizations, without a corresponding increase in opioid deaths, may reflect greater willingness to seek medical assistance because decriminalization could reduce the stigma associated with drug use,” it says.
“However, it is also possible that reduced stigma and removal of criminal penalties facilitated the diversion of safer opioids, contributing to increased hospitalizations.”
Karen Urbanoski, an associate professor in the Public Health and Social Policy department at the University of Victoria, is more critical.
“The [study’s] findings do not warrant the conclusion that these policies are causally associated with increased hospitalization or overdose,” said Urbanoski, who also holds the Canada Research Chair in Substance Use, Addictions and Health Services.
Her team published a study in November 2023 that measured safer supply’s impact on mortality and acute care visits. It found safer supply opioids did reduce overdose deaths.
Critics, however, raised concerns that her study misrepresented its underlying data and showed no statistically significant reduction in deaths after accounting for confounding factors.
The Nguyen study differs from Urbanoski’s. While Urbanoski’s team focused on individual-level outcomes, the Nguyen study analyzed broader, population-level effects, including diversion.
Wallace, the biostatistician, agrees more individual-level data could strengthen analysis, but does not believe it undermines the study’s conclusions. Wallace thinks the researchers did their best with the available data they had.
“We do not have a ‘copy’ of B.C. where the policies weren’t implemented to compare with,” said Wallace.
B.C.’s overdose rate of 775 per 100,000 is well above the national average of 533.
Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, has been a vocal critic of B.C.’s decriminalization and safer supply policies.
“If the government doesn’t want to believe this study, well then I invite them to do a similar study,” she told reporters on March 27.
“Show us the evidence that they have failed to show us since 2020,” she added, referring to the year B.C. implemented safer supply.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Our content is always free – but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoTrump Has Driven Canadians Crazy. This Is How Crazy.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCarney’s Hidden Climate Finance Agenda
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoThe Anhui Convergence: Chinese United Front Network Surfaces in Australian and Canadian Elections
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoStudy links B.C.’s drug policies to more overdoses, but researchers urge caution
-

 Automotive22 hours ago
Automotive22 hours agoHyundai moves SUV production to U.S.
-

 Entertainment1 day ago
Entertainment1 day agoPedro Pascal launches attack on J.K. Rowling over biological sex views
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoWhen it comes to pipelines, Carney’s words flow both ways
-

 2025 Federal Election18 hours ago
2025 Federal Election18 hours agoAs PM Poilievre would cancel summer holidays for MP’s so Ottawa can finally get back to work