International
Pope Francis appears frail as he returns to Vatican following 38-day hospital stay

From LifeSiteNews
By Michael Haynes, Snr. Vatican Correspondent
The Pope blessed the gathered crowd at Rome’s Gemelli hospital before leaving to return to his Vatican residence.
Pope Francis made his return to the Vatican Sunday, after first greeting crowds from the balcony of the Gemelli hospital.
For the first time in 38 days, Pope Francis appeared before the public eye on Sunday. Greeting crowds who had gathered outside the Gemelli hospital where he has been treated for double pneumonia since February 14, Francis was noticeably weakened and frail.
He wore no nasal cannulas during his less than three minute greeting on the balcony. But the toll of being without oxygen was marked, as Francis appeared particularly breathless as he was wheeled back inside.
Pope Francis gives a blessing from the Gemelli hospital window at Angelus time this morning, marking first time he has been seen since February 14.
He has now returned to the Vatican after leaving the hospital earlier today. https://t.co/jOFgg1envg pic.twitter.com/2TQhgRpLNV
— Michael Haynes 🇻🇦 (@MLJHaynes) March 23, 2025
Francis thanked the crowds before singling out and praising a woman who had brought a bouquet of flowers with her.
Accompanied by his personal nurse Massimiliano Strappetti, Francis did not seem able to raise his arms freely. After a very brief few words of thanks, Francis had to be reminded to give his blessing before then being wheeled inside by Strappetti.
This was the first time the Pope had been seen in-person since his hospitalization in mid-February – an event which his doctors noted Saturday was fraught with considerable life-threatening danger for the Pope.
Following his balcony appearance – which was live-streamed on the Vatican News media channels – Francis was driven back to the Vatican in his customary Fiat 500. But he made an unscheduled stop at St. Mary Major’s on the journey, giving the bouquet of flowers he had noticed at the hospital to the Cardinal Rolandas Makrickas, the co-adjutor priest of Francis’ favored Roman basilica.
The event was in keeping with Francis’ long-established custom of visiting the icon of Mary, Salus Populi Romani, in the basilica before and after every papal trip he has made. Indeed he has announced his desire to be buried in the basilica, and preparations have begun accordingly to ready an area close to the icon for his interment.
As stipulated by his doctors on Saturday, Francis will now begin a convalescence period of at least two months.
His motor and respiratory therapy will continue, as evidenced by the undeniable need for oxygen yesterday when he did not use it for three minutes on the balcony.
Doctors stated during Saturday’s press conference that Francis nearly lost his life twice during his time in the hospital, confirming reports which had circulated about the Pope’s condition. Indeed, Dr. Sergio Alfieri, who leads the Pope’s medical team, said that when Francis was hospitalized February 14 he “presented [with] an acute respiratory failure,” which led to “severe” double pneumonia.
Doctor leading Pope Francis' medical team confirms past seriousness of Francis' condition, incl 2 times his life was in danger
When Francis was hospitalized Feb 14 he "presented [with] an acute respiratory failure," which led to "severe" double pneumonia.
Details on @LifeSite https://t.co/2aSyyMA99g pic.twitter.com/sfBJaYhLzo— Michael Haynes 🇻🇦 (@MLJHaynes) March 22, 2025
Nurse Strappetti and Dr. Luigi Carbone – who is deputy director of the Health and Hygiene Department of Vatican City State and Francis’ physician in the Vatican – will coordinate the daily medical care of the Pope.
His social contact is limited by necessity as doctors warn about the danger of his contracting any new infection. As such, it will likely be the case that his already small inner circle of three secretaries and medical staff will be those who form part of Francis’ daily household.
While a regular visitor in the Pope’s normal schedule, Cardinal Secretary of State Pietro Parolin only visited Francis three times in his 38-day hospitalization. Such a distance between them would suggest that Parolin himself might not be anticipated to be as regular a visitor as in the past.
For now, though, Francis’ pontificate is going to be placed under particular scrutiny. He has returned to the Vatican but he is expected to be a much more hidden and vocally quiet pontiff than before.
Yet perhaps, bereft of voice, he will focus more on issuing documents and pushing through agendas he has long had in mind – such as the recent three-year extension of the Synod on Synodality.
Doctors described him as eager to return to work. His appearance on Sunday gave the impression of a man much more frail than the image painted by his clinical team.
Whether a quiet period will descend upon Vatican hill, or a season of frenzied activity begins, now remains to be seen.
Regardless, speculation of a conclave has already long begun thanks to Francis’ hospitalization, and cardinals will likely be ever more on the lookout for candidates as the year progresses.
2025 Federal Election
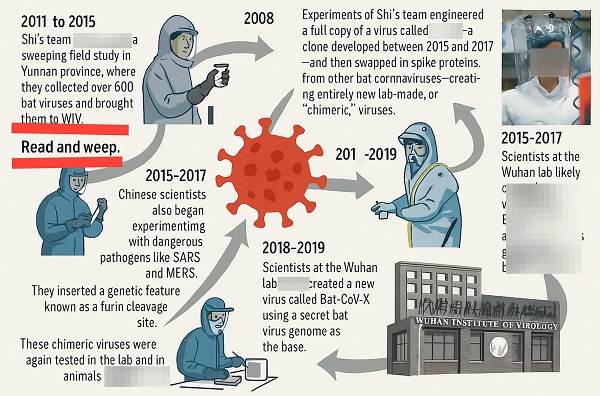
Bureau Exclusive: Chinese Election Interference Network Tied to Senate Breach Investigation

As Canada’s election unfolds, fresh questions emerge over whether foreign interference has reached Parliament’s inner chambers.
A Canadian Parliamentarian assessed by national security officials to be part of a Toronto-based Chinese consulate election interference network was the subject of a high-profile foreign interference investigation into an alleged breach of Canada’s Senate, The Bureau has confirmed through multiple intelligence sources.
Sources said the investigation examined allegations that the Parliamentarian enabled a close associate—described as a female Chinese national—to bypass Senate security protocols.
A source familiar with the Senate breach allegation said the probe was triggered by a complaint from a sitting Canadian senator, who believed they had observed a troubling pattern of behavior involving the Parliamentarian and their Chinese companion. The concern, the source said, centered on the alleged bypassing of Senate security screening, unauthorized entry into the parliamentary precinct, and access to secure Government of Canada computer systems.
While The Bureau could not independently confirm whether the allegations were ultimately substantiated, the details align closely with broader risks outlined in NSICOP’s 2024 findings on foreign interference, which stated that CSIS’s investigations were valid, and that China—and other states, including India—had established deeply concerning relationships with Canadian lawmakers.
NSICOP warned that Parliamentarians across all parties are potential targets for interference by foreign states. The committee found that such operations may be overt or covert, and that members of both the House of Commons and the Senate are considered “high-value” targets. Foreign states, the report stated, “use traditional tradecraft to build relationships that can be used to influence, coerce or exploit.”
NSICOP concluded that during the period under review, Beijing “developed clandestine networks surrounding candidates and elected officials to gain undisclosed influence and leverage over nomination processes, elections, parliamentary business and government decision-making.”
Records indicate that the Parliamentarian in question has maintained longstanding ties to several diaspora organizations affiliated with the Chinese Communist Party—including the Jiangsu Commerce Council of Canada, a business group based in Markham linked to Beijing’s United Front Work Department, and now tied to a controversial meeting with Prime Minister Mark Carney during his leadership campaign in January.
Specifically on Chinese interference, NSICOP’s explosive report stated: “The United Front Work Department… has established community organizations to facilitate influence operations against specific members of Parliament and infiltrated existing community associations to reorient them toward supporting CCP policies and narratives.”
In an interview with The Bureau, a sitting senator—who asked not to be named due to the sensitivity of the matter—was asked whether they believed NSICOP’s findings were valid and whether Chinese state actors had influenced the Senate.
“Without a doubt. Without a doubt,” the senator said. “I’ve seen it with my own eyes. Some speeches in the Senate of Canada—one would not be surprised if they had been written directly in the offices of the United Front in Beijing. Many of the senators, if you see the positions they articulate, the way they articulate and the way they vote, speaks volumes about who they stand with. But the one thing about being a public office holder—at some point in time, you’ve got to stand on your feet.”
Those observations are echoed by findings in the NSICOP report, which states: “Foreign states developed clandestine networks surrounding candidates and elected officials to gain undisclosed influence.”
The report also found that “some Parliamentarians are either semi-witting or witting participants in the efforts of foreign states to interfere in Canadian politics… including providing privileged information to foreign intelligence officers.”
However, Justice Marie-Josée Hogue, in a contrary conclusion issued through her federal inquiry, assessed that “no evidence” had been presented of intentional wrongdoing by Parliamentarians implicated in CSIS foreign interference investigations. Instead, she concluded that some officials may have made “bad decisions.”
Still, specifics of the investigation into the Parliamentarian strongly resemble the broader findings of NSICOP—particularly if the allegation of providing inappropriate access to Canada’s Senate facilities to a Chinese national is substantiated.
In interviews conducted between 2022 and 2025, The Bureau’s sources—who requested anonymity due to fears of professional retribution—said they believe Canada’s national security agencies were inhibited from pursuing broader investigations into Parliamentarians and politicians across all levels of government. They described how CSIS agents’ efforts to advance foreign interference cases were at times delayed or obstructed by senior managers reluctant to scrutinize powerful political figures.
More broadly, the sources asserted that CSIS remains structurally constrained from effectively investigating senior officials and Parliamentarians. As a result, they warned, investigations into those broadly referenced in the 2024 NSICOP Special Report on Foreign Interference have not—and likely could not—produce meaningful deterrence against ongoing threats from China and other hostile foreign states.
The Bureau’s review of open-source records shows that the Parliamentarian at the center of the Senate allegations has, from the 2019 CSIS investigation to the present, maintained significant ties to multiple Canadian organizations linked to the Chinese Communist Party’s United Front Work Department.
These include the Confederation of Toronto Chinese Canadian Organizations, the Jiangsu Commerce Council of Canada, and a third British Columbia–based entity, which has documented connections to both the United Front and the Chinese People’s Political Consultative Conference—an entity the U.S. Central Intelligence Agency has identified as Beijing’s central united front body.
The matter has gained urgency in the context of Canada’s ongoing federal election, in which Mark Carney’s party has come under scrutiny following The Globe and Mail’s revelation of his campaign’s January 2025 meeting with JCCC leadership—a meeting Carney’s team later denied. Conservative leader Pierre Poilievre has also faced criticism over his 2022 leadership race, which, according to documents and interviews reviewed by The Bureau, was allegedly targeted by both Chinese foreign interference networks and individuals aligned with the Indian government.
As previously reported by The Bureau, during the pandemic, several Liberal Party officials were involved in a PPE shipment initiative coordinated with the JCCC and authorities tied to the Chinese Communist Party. Official CCP correspondence praised the JCCC’s donations to China, and the group’s response acknowledged its operations were “organized under the guidance” of the United Front Work Department and other Party-aligned bodies. One co-signer of that letter was a senior Liberal organizer who had also served as JCCC president.
Health
Trump admin directs NIH to study ‘regret and detransition’ after chemical, surgical gender transitioning

From LifeSiteNews
Ample evidence has surfaced in recent years to warrant the White House’s investigation
The Trump administration has made a break with the long-standing government policy of near 100% affirmation of the transgender industry’s efforts and has directed the National Institutes of Health (NIH) to study the negative impacts on mental and physical health of so-called “gender transitioning” on adults and children.
The Department of Health and Human Services (HHS), which oversees NIH, “has been directed to fund research on a few specific areas” regarding “chemical and surgical mutilation” of children and adults,” according to multiple reports.
In particular, the Trump administration wants to investigate “regret and detransition following social transition as well as chemical and surgical mutilation of children and adults” and “outcomes from children who have undergone social transition and/or chemical and surgical mutilation.”
The new directives to the biomedical agency were reportedly included in an email to several NIH directors from then-Acting NIH Director Matthew Memoli shortly after Trump took office.
“This is very important to the President and the Secretary (of HHS, Robert F. Kennedy Jr.),” Memoli wrote.
Unhappy about the Trump administration’s move to uncover the hidden, shadowy side of the burgeoning transgender industry, pro-transgender activists working within the medical research community were quick to criticize the move.
The term “chemical or surgical mutilation” was “deeply offensive,” said Harry Barbee, assistant professor at the Johns Hopkins Bloomberg School of Public Health.
“This terminology has no place in serious scientific or public health discourse,” Barbee complained. “The language has been historically used to stigmatize trans people. Even the phrase(s) ‘regret’ and ‘detransition’ can be weaponized.”
“What they’re looking for is a political answer not a scientific one,” Adrian Shanker, who served as deputy assistant secretary for health policy at HHS under President Biden, told NPR. “That should be an alarm for everyone who cares about the scientific integrity of the National Institutes of Health.”
While those who derive a living focusing on developing and expanding the transgender industry resent the implication that there might be a dark side to their efforts, more than ample evidence has surfaced in recent years to warrant the White House’s investigation on behalf of vulnerable Americans, especially children, who have shown to be highly susceptible to what has been called the “transgender contagion.”
Many oft-ignored detransitioners attest to the physical and mental harm of reinforcing gender confusion as well as to the bias and negligence of the medical establishment on the subject, many of whom take an activist approach to their profession and begin cases with a predetermined conclusion in favor of “transitioning.”
A study published earlier this year in the Oxford Journal of Sexual Medicine found that undergoing sex-change surgery, far from reducing depression rates among the gender dysphoric, substantially increased rates not only of depression but of anxiety, suicidal ideation, and substance use disorders.
This study, along with scores of others conducted in recent years, explodes the media-enforced narrative that so-called “gender affirming” medical treatments are necessary for the happiness and well-being of the gender-confused.
Short video displays deep regret after sex-change treatments and surgery
A short video – just 34 seconds long – displays the extreme distress and anxiety of those who resorted to surgery and hormone treatments to “transition” earlier in their lives, only to experience deep regret later on.
The video presents a cautionary tale, dispelling the myth that parents need to allow their children to transition in order to be happy.
“Society is marketing a horrifically harmful, fashionable new trend to children that brings about a life of depression, confusion, drug use and STD’s,” the caption reads. “Please inform yourselves and help your children.”
Former transgender: ‘Regret’ and ‘detransitioning’ are the new trans frontier
Walt Heyer, a former “transgender woman” who for many years has maintained a global outreach to those who experience sex change regret, has been sounding the alarm about the one-size-fits-all approach of the trans medical industry for years.
“The science of surgical interventions is not yet settled regarding the long-term consequences of transgender therapy,” Heyer noted during a 2017 Symposium at the University of Hong Kong. “As of today, we don’t have any objective, conclusive research.”
“I feel ‘regret’ and ‘detransitioning’ will become the next transgender frontier,” Heyer said. “So be prepared.”
“There is an ever-increasing number of former transgenders, like myself, who are now requesting gender reversals,” he said.
“As a former female transgender, I can see the exploding social trend that has developed into a significant transgender contagion —now even an epidemic— that has captivated young children as well as young adults who have come to believe they’re the opposite sex on just the weight of social media and feelings … in some cases taking drastic measures to change their bodies,” Heyer said.
“More and more, I get reports from families telling me that their teen children suddenly came out as a transgender without any prior history of discomfort with their biological sex,” said Heyer, describing what has come to be called “rapid onset gender dysphoria.”
“Current psychotherapeutic practice involves the immediate affirmation of the young person’s self-diagnosis,” he lamented.
Heyer explained that many surgically transformed men and women suffer from a complex number of sexual, emotional, psychiatric and psychological comorbid disorders such as autogynephilia, dissociative disorders like schizophrenia, body dysmorphic disorder, and a host of other undiagnosed disorders that were not resolved by the recommended therapy of changing genders.
Heyer spoke from his own experience as he explained that if such disorders were considered and treated adequately, sexual transitioning would probably be greatly reduced. The role of these “comorbid” conditions tends to surface later as trans individuals begin to question their decision to transition to the opposite sex.
“We find this out from the ‘regretters,’” Heyer said. “We don’t find it out early on. We find it out afterward when they’re seeking help … and we find out that these comorbid disorders existed early on.”
A significant body of evidence now shows that “affirming” gender confusion carries serious harms, especially when done with impressionable children who lack the mental development, emotional maturity, and life experience to consider the long-term ramifications of the decisions being pushed on them or full knowledge about the long-term effects of life-altering, physically transformative, and often irreversible surgical and chemical procedures.
Studies find that more than 80 percent of children suffering gender dysphoria outgrow it on their own by late adolescence, and that “transition” procedures fail to resolve gender-confused individuals’ heightened tendency to engage in self-harm and suicide – and even exacerbate it, including by reinforcing their confusion and neglecting the actual root causes of their mental strife.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoASK YOURSELF! – Can Canada Endure, or Afford the Economic Stagnation of Carney’s Costly Climate Vision?
-

 Alberta2 days ago
Alberta2 days agoMade in Alberta! Province makes it easier to support local products with Buy Local program
-

 2025 Federal Election22 hours ago
2025 Federal Election22 hours agoEuthanasia is out of control in Canada, but nobody is talking about it on the campaign trail
-

 2025 Federal Election9 hours ago
2025 Federal Election9 hours agoMEI-Ipsos poll: 56 per cent of Canadians support increasing access to non-governmental healthcare providers
-
 2025 Federal Election17 hours ago
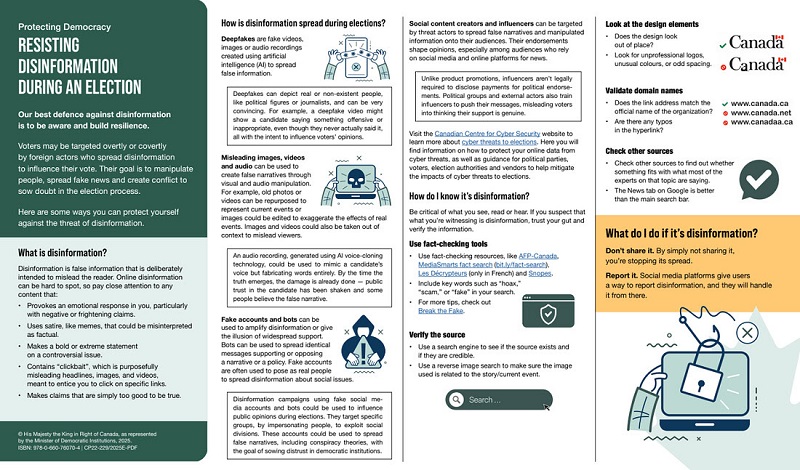
2025 Federal Election17 hours agoAI-Driven Election Interference from China, Russia, and Iran Expected, Canadian Security Officials Warn
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCSIS Warned Beijing Would Brand Conservatives as Trumpian. Now Carney’s Campaign Is Doing It.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoInside Buttongate: How the Liberal Swamp Tried to Smear the Conservative Movement — and Got Exposed
-

 illegal immigration1 day ago
illegal immigration1 day agoDespite court rulings, the Trump Administration shows no interest in helping Abrego Garcia return to the U.S.