Addictions
New organizations for mental health and addictions to provide focused care and take pressure off health system

Refocusing health care: mental health and addiction
Alberta’s government is creating two new organizations that will support the development of the mental health and addiction system of care.
In November 2023, Alberta’s government announced it would be refocusing health care with the creation of four new organizations that will be responsible for the oversight and delivery of health care services in the province. The four new organizations include acute care, continuing care, primary care and mental health and addiction. The mental health and addiction organization will be the first of these to be established when it becomes an entity later this year.
The new mental health and addiction organization, Recovery Alberta, will be responsible for the delivery of mental health and addiction services currently delivered by Alberta Health Services (AHS). In addition, Alberta’s government is establishing the Canadian Centre of Recovery Excellence (CoRE) to support Alberta’s government in building recovery-oriented systems of care by researching best practices for recovery from around the world, analyzing data and making evidence-based recommendations.
“Refocusing health care enables us to better prioritize the health care and services Albertans need. Giving Albertans living with mental health or addiction challenges an opportunity to pursue recovery and live a contributing life is the responsible and compassionate thing to do. I am so proud of the work we have done to be leaders on recovery, and I am looking forward to seeing both Recovery Alberta and the Canadian Centre of Recovery Excellence continue this work for years to come.”
“Alberta is leading the country with the development of the Alberta Recovery Model to address mental health and addiction challenges. The establishment of these two new organizations will support the delivery of recovery-oriented services to Albertans and will further cement Alberta as a leader in the field. We are proud to establish Recovery Alberta and CoRE as part of the Alberta Recovery Model.”
“We’re making good progress on refocusing health care in Alberta. Today marks a pivotal milestone towards creating a system that truly serves the needs of Albertans. Through this refocused approach, our aim is to prioritize the needs of individuals and families to find a primary care provider, get urgent care without long waits, access the best continuing care options, and have robust support systems for addiction recovery and mental health treatment.”
Recovery Alberta
In August 2023, Alberta’s Ministry of Mental Health and Addiction began the process of consolidating the delivery of mental health and addiction services within AHS, a process that was completed in November 2023 with no disruption to services.
Recovery Alberta will report to the Ministry of Mental Health and Addiction and further support the Ministry’s mandate to provide high-quality, recovery-oriented mental health and addiction services to Albertans. It is anticipated Recovery Alberta will be fully operational by summer 2024 and will operate with an annual budget of $1.13 billion from Alberta’s government. This funding currently supports the delivery of mental health and addiction services through AHS.
The current provincial leadership team for Addiction and Mental Health and Correctional Health Services within AHS will form the leadership team of Recovery Alberta. When Recovery Alberta is fully established, Kerry Bales, the current Chief Program Officer for Addiction and Mental Health and Correctional Health Services within AHS will be appointed as CEO. Dr. Nick Mitchell, Provincial Medical Director, Addiction and Mental Health and Correctional Health Services within AHS, will become the Provincial Medical Director for Recovery Alberta.
“Recovery Alberta will build on the strong foundation of existing mental health and addiction services that staff and clinicians deliver. By working closely with Alberta Mental Health and Addiction and the Canadian Centre of Recovery Excellence, Recovery Alberta will continue to set a high standard of care for mental health and addiction recovery across the province, and beyond.”
“Albertans deserve patient-centered care when and where they need it. By establishing Recovery Alberta, we have an opportunity to work together in a new way to make that a reality for our patients and our communities.”
While timelines are dependent on legislative amendments yet to be introduced, the Ministry of Mental Health and Addiction is aiming to establish the corporate structure of Recovery Alberta by June 3. Following the establishment of the corporate structure and executive team, staff and services would begin operation under the banner of Recovery Alberta on July 1.
Frontline workers and service providers will continue to be essential to care for Albertans. To ensure stability of services to Albertans, there will be no changes to terms and conditions of employment for AHS addiction and mental health staff transitioning to Recovery Alberta. Additionally, there will be no changes to grants or contracts for service providers currently under agreement with AHS upon establishment of Recovery Alberta.
Canadian Centre of Recovery Excellence (CoRE)
Alberta’s government has been leading the country in creating a system focused on recovery by building on evidence-based best practices from around the world. In five years, Alberta has removed user fees for treatment, increased publicly funded treatment capacity by 55 per cent and built two recovery communities with nine more on the way. Alberta’s government has also pioneered new best practices such as making evidence-based treatment medication available same day with no cost and no waitlist across the province through the Virtual Opioid Dependency Program.
To continue the innovative work required to improve the mental health and addiction system, Alberta’s government is creating the Canadian Centre of Recovery Excellence to inform best practices in mental health and addiction, conduct research and program evaluation and support the development of evidence-based policies for mental health and addiction. CoRE will be established as a crown corporation through legislation to be introduced this spring.
Alberta’s government has committed $5 million through Budget 2024 to support the establishment of CoRE. It is anticipated CoRE will be operational by this summer.
The CoRE leadership team will consist of Kym Kaufmann, former Deputy Minister of Mental Health and Community Wellness in Manitoba as the CEO. She will be supported by Dr. Nathaniel Day as Chief Scientific Officer of CoRE. Dr. Day currently serves as the Medical Director of Addiction and Mental Health within AHS.
“There is a need for more scientific evidence on how best to help those impacted by addiction within our society. The Canadian Centre of Recovery Excellence will generate new and expanded evidence on the most effective means to support individuals to start and sustain recovery.”
“The Canadian Centre of Recovery Excellence will provide the research and data we need to understand what works best when it comes to recovery. This new expertise and expanded evidence will provide us with further insight into how we can support communities, service providers and frontline staff to effectively help those living with addiction and mental health challenges.”
Quick facts
- Budget 2024 will invest more than $1.55 billion to continue building the Alberta Recovery Model.
- This includes a $1.13 billion transfer from Health to Mental Health and Addiction (MHA) for mental health and addiction services currently delivered by Alberta Health Services.
- Virtual engagement sessions for AHS staff and service providers will be held on April 11, 16, 17 and 22.
Related information
2025 Federal Election
Poilievre to invest in recovery, cut off federal funding for opioids and defund drug dens

From Conservative Party Communications
Poilievre will Make Recovery a Reality for 50,000 Canadians
Conservative Leader Pierre Poilievre pledged he will bring the hope that our vulnerable Canadians need by expanding drug recovery programs, creating 50,000 new opportunities for Canadians seeking freedom from addiction. At the same time, he will stop federal funding for opioids, defund federal drug dens, and ensure that any remaining sites do not operate within 500 meters of schools, daycares, playgrounds, parks and seniors’ homes, and comply with strict new oversight rules that focus on pathways to treatment.
More than 50,000 people have lost their lives to fentanyl since 2015—more Canadians than died in the Second World War. Poilievre pledged to open a path to recovery while cracking down on the radical Liberal experiment with free access to illegal drugs that has made the crisis worse and brought disorder to local communities.
Specifically, Poilievre will:
- Fund treatment for 50,000 Canadians. A new Conservative government will fund treatment for 50,000 Canadians in treatment centres with a proven record of success at getting people off drugs. This includes successful models like the Bruce Oake Recovery Centre, which helps people recover and reunite with their families, communities, and culture. To ensure the best outcomes, funding will follow results. Where spaces in good treatment programs exist, we will use them, and where they need to expand, these funds will allow that.
- Ban drug dens from being located within 500 metres of schools, daycares, playgrounds, parks, and seniors’ homes and impose strict new oversight rules. Poilievre also pledged to crack down on the Liberals’ reckless experiments with free access to illegal drugs that allow provinces to operate drug sites with no oversight, while pausing any new federal exemptions until evidence justifies they support recovery. Existing federal sites will be required to operate away from residential communities and places where families and children frequent and will now also have to focus on connecting users with treatment, meet stricter regulatory standards or be shut down. He will also end the exemption for fly-by-night provincially-regulated sites.
“After the Lost Liberal Decade, Canada’s addiction crisis has spiralled out of control,” said Poilievre. “Families have been torn apart while children have to witness open drug use and walk through dangerous encampments to get to school. Canadians deserve better than the endless Liberal cycle of crime, despair, and death.”
Since the Liberals were first elected in 2015, our once-safe communities have become sordid and disordered, while more and more Canadians have been lost to the dangerous drugs the Liberals have flooded into our streets. In British Columbia, where the Liberals decriminalized dangerous drugs like fentanyl and meth, drug overdose deaths increased by 200 percent.
The Liberals also pursued a radical experiment of taxpayer-funded hard drugs, which are often diverted and resold to children and other vulnerable Canadians. The Vancouver Police Department has said that roughly half of all hydromorphone seizures were diverted from this hard drugs program, while the Waterloo Regional Police Service and Niagara Regional Police Service said that hydromorphone seizures had exploded by 1,090% and 1,577%, respectively.
Despite the death and despair that is now common on our streets, bizarrely Mark Carney told a room of Liberal supporters that 50,000 fentanyl deaths in Canada is not “a crisis.” He also hand-picked a Liberal candidate who said the Liberals “would be smart to lean into drug decriminalization” and another who said “legalizing all drugs would be good for Canada.”
Carney’s star candidate Gregor Robertson, an early advocate of decriminalization and so-called safe supply, wanted drug dens imposed on communities without any consultation or public safety considerations. During his disastrous tenure as Vancouver Mayor, overdoses increased by 600%.
Alberta has pioneered an approach that offers real hope by adopting a recovery-focused model of care, leading to a nearly 40 percent reduction in drug-poisoning deaths since 2023—three times the decrease seen in British Columbia. However, we must also end the Liberal drug policies that have worsened the crisis and harmed countless lives and families.
To fund this policy, a Conservative government will stop federal funding for opioids, defund federal drug dens, and sue the opioid manufacturers and consulting companies who created this crisis in the first place.
“Canadians deserve better than the Liberal cycle of crime, despair, and death,” said Poilievre. “We will treat addiction with compassion and accountability—not with more taxpayer-funded poison. We will turn hurt into hope by shutting down drug dens, restoring order in our communities, funding real recovery, and bringing our loved ones home drug-free.”
Addictions
There’s No Such Thing as a “Safer Supply” of Drugs

By Adam Zivo
Sweden, the U.K., and Canada all experimented with providing opioids to addicts. The results were disastrous.
[This article was originally published in City Journal, a public policy magazine and website published by the Manhattan Institute for Policy Research. We encourage our readers to subscribe to them for high-quality analysis on urban issues]
Last August, Denver’s city council passed a proclamation endorsing radical “harm reduction” strategies to address the drug crisis. Among these was “safer supply,” the idea that the government should give drug users their drug of choice, for free. Safer supply is a popular idea among drug-reform activists. But other countries have already tested this experiment and seen disastrous results, including more addiction, crime, and overdose deaths. It would be foolish to follow their example.
The safer-supply movement maintains that drug-related overdoses, infections, and deaths are driven by the unpredictability of the black market, where drugs are inconsistently dosed and often adulterated with other toxic substances. With ultra-potent opioids like fentanyl, even minor dosing errors can prove fatal. Drug contaminants, which dealers use to provide a stronger high at a lower cost, can be just as deadly and potentially disfiguring.
Because of this, harm-reduction activists sometimes argue that governments should provide a free supply of unadulterated, “safe” drugs to get users to abandon the dangerous street supply. Or they say that such drugs should be sold in a controlled manner, like alcohol or cannabis—an endorsement of partial or total drug legalization.
But “safe” is a relative term: the drugs championed by these activists include pharmaceutical-grade fentanyl, hydromorphone (an opioid as potent as heroin), and prescription meth. Though less risky than their illicit alternatives, these drugs are still profoundly dangerous.
The theory behind safer supply is not entirely unreasonable, but in every country that has tried it, implementation has led to increased suffering and addiction. In Europe, only Sweden and the U.K. have tested safer supply, both in the 1960s. The Swedish model gave more than 100 addicts nearly unlimited access through their doctors to prescriptions for morphine and amphetamines, with no expectations of supervised consumption. Recipients mostly sold their free drugs on the black market, often through a network of “satellite patients” (addicts who purchased prescribed drugs). This led to an explosion of addiction and public disorder.
Most doctors quickly abandoned the experiment, and it was shut down after just two years and several high-profile overdose deaths, including that of a 17-year-old girl. Media coverage portrayed safer supply as a generational medical scandal and noted that the British, after experiencing similar problems, also abandoned their experiment.
While the U.S. has never formally adopted a safer-supply policy, it experienced something functionally similar during the OxyContin crisis of the 2000s. At the time, access to the powerful opioid was virtually unrestricted in many parts of North America. Addicts turned to pharmacies for an easy fix and often sold or traded their extra pills for a quick buck. Unscrupulous “pill mills” handed out prescriptions like candy, flooding communities with OxyContin and similar narcotics. The result was a devastating opioid epidemic—one that rages to this day, at a cumulative cost of hundreds of thousands of American lives. Canada was similarly affected.
The OxyContin crisis explains why many experienced addiction experts were aghast when Canada greatly expanded access to safer supply in 2020, following a four-year pilot project. They worried that the mistakes of the recent past were being made all over again, and that the recently vanquished pill mills had returned under the cloak of “harm reduction.”
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Most Canadian safer-supply prescribers dispense large quantities of hydromorphone with little to no supervised consumption. Patients can receive up to 40 eight-milligram pills per day—despite the fact that just two or three are enough to cause an overdose in someone without opioid tolerance. Some prescribers also provide supplementary fentanyl, oxycodone, or stimulants.
Unfortunately, many safer-supply patients sell or trade a significant portion of these drugs—primarily hydromorphone—in order to purchase more potent illicit substances, such as street fentanyl.
The problems with safer supply entered Canada’s consciousness in mid-2023, through an investigative report I wrote for the National Post. I interviewed 14 addiction physicians from across the country, who testified that safer-supply diversion is ubiquitous; that the street price of hydromorphone collapsed by up to 95 percent in communities where safer supply is available; that youth are consuming and becoming addicted to diverted safer-supply drugs; and that organized crime traffics these drugs.
Facing pushback, I interviewed former drug users, who estimated that roughly 80 percent of the safer-supply drugs flowing through their social circles was getting diverted. I documented dozens of examples of safer-supply trafficking online, representing tens of thousands of pills. I spoke with youth who had developed addictions from diverted safer supply and adults who had purchased thousands of such pills.
After months of public queries, the police department of London, Ontario—where safer supply was first piloted—revealed last summer that annual hydromorphone seizures rose over 3,000 percent between 2019 and 2023. The department later held a press conference warning that gangs clearly traffic safer supply. The police departments of two nearby midsize cities also saw their post-2019 hydromorphone seizures increase more than 1,000 percent.
The Canadian government quietly dropped its support for safer supply last year, cutting funding for many of its pilot programs. The province of British Columbia (the nexus of the harm-reduction movement) finally pulled back support last month, after a leaked presentation confirmed that safer-supply drugs are getting sold internationally and that the government is investigating 60 pharmacies for paying kickbacks to safer-supply patients. For now, all safer-supply drugs dispensed within the province must be consumed under supervision.
Harm-reduction activists have insisted that no hard evidence exists of widespread diversion of safer-supply drugs, but this is only because they refuse to study the issue. Most “studies” supporting safer supply are produced by ideologically driven activist-scholars, who tend to interview a small number of program enrollees. These activists also reject attempts to track diversion as “stigmatizing.”
The experiences of Sweden, the United Kingdom, and Canada offer a clear warning: safer supply is a reliably harmful policy. The outcomes speak for themselves—rising addiction, diversion, and little evidence of long-term benefit.
As the debate unfolds in the United States, policymakers would do well to learn from these failures. Americans should not be made to endure the consequences of a policy already discredited abroad simply because progressive leaders choose to ignore the record. The question now is whether we will repeat others’ mistakes—or chart a more responsible course.
Our content is always free –
but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
-

 Daily Caller2 days ago
Daily Caller2 days agoTrump Executive Orders ensure ‘Beautiful Clean’ Affordable Coal will continue to bolster US energy grid
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoBREAKING from THE BUREAU: Pro-Beijing Group That Pushed Erin O’Toole’s Exit Warns Chinese Canadians to “Vote Carefully”
-
 Business2 days ago
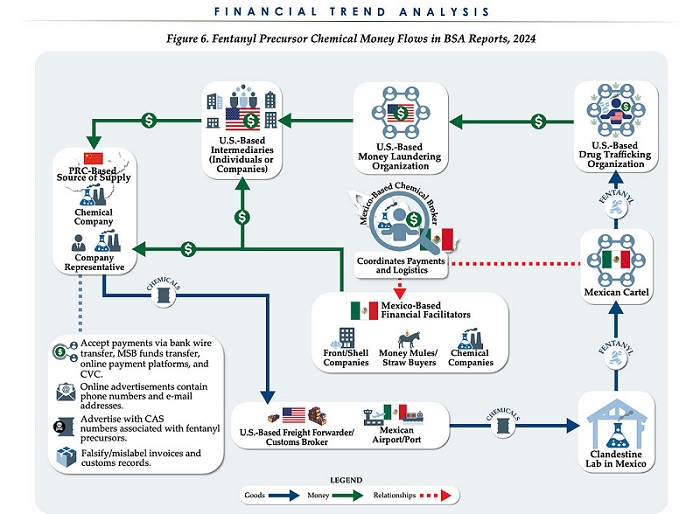
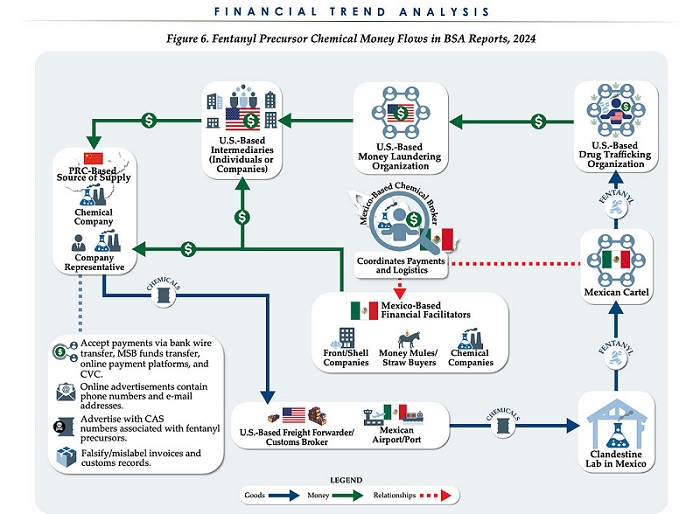
Business2 days agoChina, Mexico, Canada Flagged in $1.4 Billion Fentanyl Trade by U.S. Financial Watchdog
-

 COVID-192 days ago
COVID-192 days agoTamara Lich and Chris Barber trial update: The Longest Mischief Trial of All Time continues..
-
 2025 Federal Election18 hours ago
2025 Federal Election18 hours agoPRC-Linked Disinformation Claims Conservatives Threaten Chinese Diaspora Interests, Take Aim at PM Carney’s Debate Remark
-
 Energy2 days ago
Energy2 days agoStraits of Mackinac Tunnel for Line 5 Pipeline to get “accelerated review”: US Army Corps of Engineers
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoAllegations of ethical misconduct by the Prime Minister and Government of Canada during the current federal election campaign
-

 Daily Caller2 days ago
Daily Caller2 days agoDOJ Releases Dossier Of Deported Maryland Man’s Alleged MS-13 Gang Ties