Mental Health
Mental Health, MAID, and Governance in Trudeau’s Canada

|
|
The Opposition with Dan Knight
A Critical Examination of Governance, Ethical Implications, and the Search for Compassionate Solutions in a Nation in Crisis
The mental health crisis in Canada, deepened and exacerbated under Prime Minister Justin Trudeau’s leadership, has laid bare the stark realities and the fundamental cracks in our national mental health support structures. The haunting statistics released by the Angus Reid Institute have catapulted this crisis to the forefront of national discourse, but it seems that the ramifications extend far beyond mere numbers. Approximately 80% of Canadians are grappling with the inadequate availability of mental health resources, and the governmental response, or lack thereof, has amplified this concern.
Under Trudeau’s regime, the pervasive decline in mental health has not only been met with superficial commitments but has also seen the advancement of policies that many argue are an affront to the sanctity of life and individual liberty, namely, the Medical Assistance in Dying (MAID) legislation.
The Trudeau administration, amidst the throes of a profound mental health crisis, had pledged a seemingly substantial $4.5 billion over five years to address mental health care during the 2021 federal election. However, the tangible execution of this commitment remains elusive, with the funds ostensibly being absorbed into broader health care allocations. A dire need, once seemingly acknowledged, now seemingly diluted in priorities.
It’s in this same disconcerting timeframe that the contentious discussions around MAID have intensified. The proposed legislative modifications seek to expand the eligibility criteria to include individuals whose sole medical condition is a mental illness. This proposition has resulted in a fierce national debate and has amplified concerns over the values and the ethical compass guiding our nation’s leadership.
While the inception of MAID in 2016 found support among 64% of Canadians, the broadening of its scope to include mental illnesses has sparked widespread hesitation and reflection on its ethical implications. A mere 28% of Canadians support allowing those with only a mental illness to seek MAID. This shift in public sentiment is indicative of a collective realization of the complex moral, ethical, and societal implications of such a policy in a nation already strained by a lack of mental health support.
There’s an unsettling correlation between the difficulties in accessing mental health care and the support for the expansion of MAID. Two in five Canadians who’ve encountered barriers in accessing mental health care express support for the inclusion of mental illnesses in MAID eligibility. This correlation rings alarm bells about the level of desperation and despair fueled by inadequate mental health resources and support.
The MAID legislation, particularly its proposed expansion, is symptomatic of a deeper, more entrenched disregard for life and liberty. The policies and legislation emanating from Trudeau’s administration seem to foster an environment where the value of life is underplayed, and individual freedoms are undervalued. Rather than addressing the root causes and formulating holistic, compassionate solutions for mental health struggles, the government seems poised to offer an expedited escape route, overlooking the sanctity of life and the intrinsic rights of the individuals.
The urgency to address mental health challenges, especially those disproportionately affecting women, young adults, and lower-income households, is paramount. It requires genuine, sustained commitments and actions, far removed from mere electoral promises and rhetoric. The dialogue surrounding MAID, although crucial, risks overshadowing the fundamental issues at hand – the acute need for enhanced, accessible mental health care resources and a governmental ethos that values and preserves life and liberty.
In light of these pivotal concerns, this beckons a grave question to us all: Is this truly the Canada we desire? A Canada where, when faced with life’s vicissitudes, the solution provided by the government is simply to opt for MAID? Or do we yearn for a Canada that embodies hope, a belief that circumstances can, and will, improve? When 2025 arrives, the bell will indeed toll for Justin Trudeau and his Liberal compatriots, and we, as staunch Canadians, will need to rise to the occasion and answer this question. It’s a query not merely about policies or governance but about the very soul and essence of our great nation.
Subscribe to The Opposition with Dan Knight
I’m an independent Canadian journalist exposing corruption, delivering unfiltered truths and untold stories. Join me on Substack for fearless reporting that goes beyond headlines
armed forces
Yet another struggling soldier says Veteran Affairs Canada offered him euthanasia

From LifeSiteNews
‘It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself.’
Yet another Canadian combat veteran has come forward to reveal that when he sought help, he was instead offered euthanasia.
David Baltzer, who served two tours in Afghanistan with the Princess Patricia’s Canadian Light Infantry, revealed to the Toronto Sun that he was offered euthanasia on December 23, 2019—making him, as the Sun noted, “among the first Canadian soldiers offered therapeutic suicide by the federal government.”
Baltzer had been having a disagreement with his existing caseworker, when assisted suicide was brought up in in call with a different agent from Veteran Affairs Canada.
“It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself,” Baltzer told the Sun.“I was in my lowest down point, it was just before Christmas. He says to me, ‘I would like to make a suggestion for you. Keep an open mind, think about it, you’ve tried all this and nothing seems to be working, but have you thought about medical-assisted suicide?’”
Baltzer was stunned. “It just seems to me that they just want us to be like ‘f–k this, I give up, this sucks, I’d rather just take my own life,’” he said. “That’s how I honestly felt.”
Baltzer, who is from St. Catharines, Ontario, joined up at age 17, and moved to Manitoba to join the Princess Patricia’s Canadian Light Infantry, one of Canada’s elite units. He headed to Afghanistan in 2006. The Sun noted that he “was among Canada’s first troops deployed to Afghanistan as part Operation Athena, where he served two tours and saw plenty of combat.”
“We went out on long-range patrols trying to find the Taliban, and that’s exactly what we did,” Baltzer said. “The best way I can describe it, it was like Black Hawk Down — all of the sudden the s–t hit the fan and I was like ‘wow, we’re fighting, who would have thought? Canada hasn’t fought like this since the Korean War.”
After returning from Afghanistan, Baltzer says he was offered counselling by Veteran Affairs Canada, but it “was of little help,” and he began to self-medicate for his trauma through substance abuse (he noted that he is, thankfully, doing well today). Baltzer’s story is part of a growing scandal. As the Sun reported:
A key figure shedding light on the VAC MAID scandal was CAF veteran Mark Meincke, whose trauma-recovery podcast Operation Tango Romeo broke the story. ‘Veterans, especially combat veterans, usually don’t reach out for help until like a year longer than they should’ve,’ Meincke said, telling the Sun he waited over two decades before seeking help.
‘We’re desperate by the time we put our hands up for help. Offering MAID is like throwing a cinderblock instead of a life preserver.’ Meincke said Baltzer’s story shoots down VAC’s assertions blaming one caseworker for offering MAID to veterans, and suggests the problem is far more serious than some rogue public servant.
‘It had to have been policy. because it’s just too many people in too many provinces,” Meincke told the Sun. “Every province has service agents from that province.’
Veterans Affairs Canada claimed in 2022 that between four and 20 veterans had been offered assisted suicide; Meincke “personally knows of five, and said the actual number’s likely close to 20.” In a previous investigation, VAC claimed that only one caseworker was responsible—at least for the four confirmed cases—and that the person “was lo longer employed with VAC.” Baltzer says VAC should have military vets as caseworkers, rather than civilians who can’t understand what vets have been through.
To date, no federal party leader has referenced Canada’s ongoing euthanasia scandals during the 2025 election campaign.
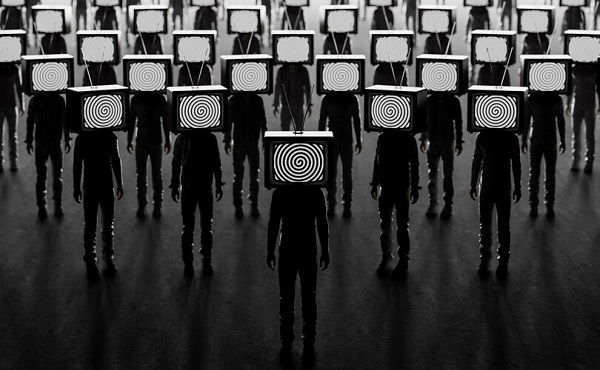
Censorship Industrial Complex
CIA mind control never ended – it evolved and went mainstream
From LifeSiteNews
From the CIA’s MKUltra to Britain’s COVID fear tactics, governments have spent decades perfecting psychological operations against their own people.
Surveying the battlefield
For thousands of years, military strategists have understood that an army’s success often depends not on its size or even on its armaments but on its knowledge of the opponent.
After all, as Sun Tzu observes:
If you know the enemy and know yourself, you need not fear the result of a hundred battles. If you know yourself but not the enemy, for every victory gained you will also suffer a defeat. If you know neither the enemy nor yourself, you will succumb in every battle.
It follows, then, that the success of the globalists in their fifth-generation war on us all depends on their knowledge of humanity itself.
What makes people tick? What motivates and demotivates them? What stimuli do they respond to, and in what way do they respond?
From the viewpoint of those wishing to manipulate, control and subdue humanity, the knowledge of the human mind that can be gleaned from the answers to these questions is the most prized knowledge of all.
So, it shouldn’t be surprising to learn that not only scientific researchers but military planners and government officials have spent centuries trying to better understand humans and their behaviors – and, more importantly, how to mold, influence, shape, or outright control those behaviors.
Everyone knows about Ivan Pavlov’s experiments in conditioning. Any high schooler could tell you how Pavlov was able to condition dogs to salivate upon hearing the ringing of a dinner bell.
But how many know that Pavlov’s research didn’t end with his observation of canines? That he next began duplicating his experiments on human subjects? That those human experiments saw Pavlov and his protégé, Nikoli Krasnogorsky, scooping orphans off the streets, drugging them, surgically fitting them with salivation monitors and force-feeding them food so that these children, like Pavlov’s dogs, could be trained to salivate on command?

READ: Is the US Intelligence Community hiding secret weapons from the American public?
How many are familiar with the experimenters who followed in Pavlov’s footsteps? How many have seen the footage of John B. Watson’s “Little Albert” experiments, where the psychologist deliberately traumatized an 11-month-old baby in an attempt to refine the techniques of conditioning humans?
How many have read Watson himself bragging that “[a]fter conditioning, even the sight of the long whiskers of a Santa Claus mask sends the youngster scuttling away, crying and shaking his head from side to side”?

How many have followed the thread from Pavlov and Watson and the “classical conditioning” researchers to the “radical behaviorists” like B. F. Skinner and his work in perfecting operant conditioning?
How many have read Skinner’s Walden Two, in which he proposes a scheme for creating a utopian society by conditioning children from birth to assume specific roles in society?
By this point, it’s fairly common knowledge that the CIA conducted mind control experiments like Project MKUltra, using operatives like Sidney Gottlieb and Dr. Ewan Cameron to administer LSD to unwitting subjects and conduct other ghoulish experiments in mental manipulation. But how many have heard of MKSearch or MKChickwit or MKOften or any of the other spin-offs of this nightmarish research?
How many know these experiments “were designed to destabilize human personality by creating behavior disturbances, altered sex patterns, aberrant behavior using sensory deprivation and various powerful stress-producing chemicals, and mind-altering substances” and were carried out on so-called “expendables” – i.e., “people whose death or disappearance would arouse no suspicion”?
How many have heard of George Brock Chisholm, who served as the first Director-General of the World Health Organization and helped spearhead the World Federation for Mental Health? How many have read the transcript of his 1945 lecture, “The Reestablishment of Peacetime Psychiatry,” in which he declared, “If the race is to be freed from its crippling burden of good and evil it must be psychiatrists who take the original responsibility”?
And how many are aware that Chisholm’s call to action was heeded by men like British military psychiatrist Colonel John Rawlings Rees, the first president of Chisholm’s World Federation of Mental Health and chair of the infamous Tavistock Institute from 1933 to 1947?
How many know the story of how Dr. Jim Mitchell – a military retiree and psychologist who had contracted to provide training services to the CIA – took the findings of Dr. Martin Seligman on the psychological phenomenon of “learned helplessness” and weaponized them for the CIA in the service of the agency’s post-9/11 illegal torture program?
Whether the general public is aware of this documented history or not, the record shows that the last 125 years of research into the human psyche has been conducted – or at least weaponized – by Machiavellian manipulators and secret schemers whose intent is to socially engineer the masses.
And, as the science of the mind progresses in the 21st century, these social engineering schemes are only getting more effective.
The information war
The alternative media has certainly had cause to note that we here in the 21st century are the (largely unwitting) targets of a large-scale information war. This war is being waged upon us largely (though not exclusively) by our own governments.
Occasionally, stories of some of the campaigns in this war break through the information blockade, and the public catches a glimpse of the battle that is being waged against them on all fronts.
Bemused Canadians, for example, were able to read about the Canadian military’s bizarre “wolf letter” psyop in the pages of The Ottawa Citizen back in 2021. But any concerns that might have been raised by this psyop and its wild story of forged government letters and recorded wolf noises were soon quelled by the usual establishment lapdog journalists.
The whole thing, we were told, was caused by “a handful of military reservists testing psychological tactics at a weekend exercise” and “new control measures are now in place to ensure psychological operation exercises and influence activities do not reach unintended audiences” – so, obviously there’s nothing more to worry about!
Residents of the U.K., meanwhile, got their own glimpse of the infowar in 2021 when members of the Scientific Pandemic Influenza Group on Behaviour (SPI-B) – a group providing “independent, expert, social and behavioural science advice” to the U.K. government – admitted they were guilty of “using fear as a means of control.”
Tasked with providing insight on how to make Britons compliant with their government’s lockdown, social distancing, masking, and other restrictions at the beginning of the scamdemic, the SPI-B experts urged the government to increase “the perceived level of personal threat” from COVID-19. Multiple members of the SPI-B team later expressed regret about the scheme, calling it “totalitarian” and unethical.
One SPI-B member confessed: “You could call psychology ‘mind control.’ That’s what we do.”
Another put it even more bluntly: “Without a vaccine, psychology is your main weapon … Psychology has had a really good epidemic, actually.”
But to the extent that these operations ever come to public light, it is almost always in disconnected and decontextualized stories like these. Those Canadians who learned about the “wolf letter” psyop, for example, likely never read about the SPI-B scamdemic psyop, let alone connected the events together as evidence of the all-out infowar.
In recent years, however, the existence of the infowar has not only become undeniable. It is undenied.
The cognitive domain of the information battlespace
In 2022, the Associated Press published “‘Pre-bunking’ shows promise in fight against misinformation,” an article touting new research that claims to show progress in the creation of new weapons in the information war.
After detailing the usual examples of the scourge of “misinformation” – i.e., observations that erode public faith in “democratic institutions, journalism and science” – the article then reports uncritically on new techniques that are being developed to trick the public into once again trusting these demonstrably untrustworthy institutions:
New findings from university researchers and Google, however, reveal that one of the most promising responses to misinformation may also be one of the simplest.
In a paper published Wednesday in the journal Science Advances, the researchers detail how short online videos that teach basic critical thinking skills can make people better able to resist misinformation.
The researchers created a series of videos similar to a public service announcement that focused on specific misinformation techniques – characteristics seen in many common false claims that include emotionally charged language, personal attacks or false comparisons between two unrelated items.
Researchers then gave people a series of claims and found that those who watched the videos were significantly better at distinguishing false information from accurate information.
Although research like that touted by the AP is ostensibly civilian in nature, the fact that this information campaign is part of a literal military battle that is being waged against us is now starting to be admitted, as well.
In 2023, for example, the Japanese military officially added the “cognitive domain” as the latest new battle domain added to Japan’s National Defense Program Guideline. In addition to the traditional domains of territorial land, water, and airspace, and to newly added domains like space, cyberspace, and the electrogmagnetic domain, Japan’s defense authorities now claim the cognitive space as part of their remit.
According to The Global Times:
The building of such cognitive capability would also be written into the National Security Strategy, one of the three major diplomatic and security documents to be amended before the end of 2022, VOA Chinese reported, citing the theory that the Japanese defense authorities and the Self-Defense Force attach great importance to the “misinformation” released by Russia and China, consider that information spread in the Chinese language is a global trend and that cognitive warfare by the island of Taiwan against the Chinese mainland provides valuable experience for research and study.
[…]
Analysts said that cognitive warfare is a combination of digital information, media and spy technology that leads public opinion to extremes in order to affect the basis of diplomacy between countries and to realize the goals of political manipulation, citing the U.S.’ infamous “peaceful transfer of power” strategy in other countries as an example.
The recognition of the “cognitive domain” as a literal battlefield is not limited to the Japanese defense forces, however.
In 2019, the Chinese State Council Information Office released a white paper on “China’s National Defense in the New Era,” arguing that “[w]ar is evolving in form towards informationized [sic] warfare, and intelligent warfare is on the horizon.”
In 2022, Motohiro Tsuchiya, a professor at Keio University, wrote an article on “Governing Cognitive Warfare” for Governing the Global Commons: Challenges and Opportunities for US-Japan Cooperation (a publication of the German Marshall Fund of the United States!) in which he warned that the threat of “intelligentized warfare” by China and other U.S. State Department bogeymen necessitated U.S. cooperation to “create and promote rules and norms that can effectively govern cyberwarfare.”
And, perhaps inevitably, it wasn’t long before it was discovered that the real threat in this new “cognitive domain” isn’t the ChiComs or the CRINKs or any other outside force, but… *drumroll, please*… online conspiracy theorists!
That’s right, in 2023, Tomoko Nagasako, a research fellow at The Sasakawa Peace Foundation, penned “The Threat of Conspiracy Theories in the Battle for the Cognitive Domain – A Consideration of the Status of Conspiracy Theories in Japan Based on Attempts at Regime Destruction Overseas.” As you might guess from that title, the article provides “an overview of the state of conspiracy theories overseas and in Japan,” details how these dastardly conspiracy theorists present a threat to national security “[f]rom the perspective of cognitive warfare,” and proposes countermeasures to address these grave dangers to the nation.
And what “conspiracy theories” does Nagasako cite in her piece? That there exists a “deep state” over and above the surface-level government, that the COVID vaccines were harmful, that the U.S. has conducted biological weapons research in Ukraine in recent years… you know, the usual harebrained ideas that only kooky conspiracy realists would even entertain.
Yes, for those who haven’t received the memo yet: there most certainly is a war for your mind. It certainly is taking place right now. It is being waged by militaries around the world. The target of these wars is, more often than not, these very militaries’ fellow countrymen.
To those who are just waking up to this war, you have my deepest sympathy. Realizing that you are a target in a battle you didn’t even know you were fighting in a “cognitive domain” you never even knew existed must be wildly disorienting, to say the least.
But here’s the bad news: new technologies are being developed that will make all of this history – from Pavlov to Skinner to Mitchell to SPI-B – and all of these secret operations – from MKUltra to MKChickwit – and all of these military campaigns – from Chisholm and Rees and the machinations of the Tavistock minions to the ChiComs and the Japanese and the development of cognitive warfare – seem like small potatoes.
As we shall see in a follow-up article, the technology to rewire the brain – quite literally – is already being tested and deployed. And, once these technologies are ready to be unleashed on the public, they may bring the age-old dream of the dictators for total domination of the human population to reality.
Reprinted with permission from the Corbett Report.
-

 Automotive2 days ago
Automotive2 days agoHyundai moves SUV production to U.S.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoAs PM Poilievre would cancel summer holidays for MP’s so Ottawa can finally get back to work
-

 armed forces1 day ago
armed forces1 day agoYet another struggling soldier says Veteran Affairs Canada offered him euthanasia
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPoilievre Campaigning To Build A Canadian Economic Fortress
-

 Opinion10 hours ago
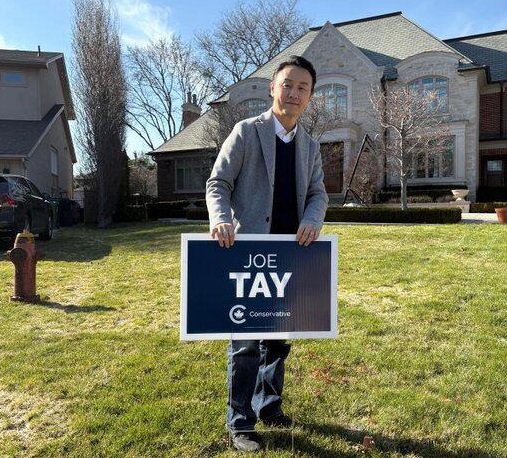
Opinion10 hours agoCanadians Must Turn Out in Historic Numbers—Following Taiwan’s Example to Defeat PRC Election Interference
-

 International18 hours ago
International18 hours agoHistory in the making? Trump, Zelensky hold meeting about Ukraine war in Vatican ahead of Francis’ funeral
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoThe Cost of Underselling Canadian Oil and Gas to the USA
-

 Automotive2 days ago
Automotive2 days agoCanadians’ Interest in Buying an EV Falls for Third Year in a Row