Health
Last day for fans at the Player’s Championship

PGA Commissioner Jay Monahan has just held a news conference to announce the PGA’s plans moving forward this weekend and beyond.
The Player’s Championship will continue this weekend without fans after today. The thoughts are that the players can continue because they play outside, the players distance themselves anyway, and there is little to no need for any physical contact.
Here’s the statement from their Website.
The PGA TOUR is aware of rapidly changing developments regarding COVID-19. With the information currently available, THE PLAYERS Championship will continue as scheduled, although we will absolutely continue to review recommendations from the Centers for Disease Control, World Health Organization and local health administrations. This is obviously a very fluid situation that requires constant review, communication and transparency, and we are dedicated to all three aspects. The PGA TOUR will provide an additional update by 12 p.m. ET on Thursday.
In the meantime, players in the field have been notified to be prepared to play Round 1, as scheduled.
Fans who no longer wish to attend THE PLAYERS Championship may request a refund or exchange; details on how to do so will be announced shortly. Please visit PGATOUR.COM/THEPLAYERS for more information.
LISTEN: My date with self-isolation amid the Covid 19 scare – J’Lyn Nye Interview
Censorship Industrial Complex
CIA mind control never ended – it evolved and went mainstream
From LifeSiteNews
From the CIA’s MKUltra to Britain’s COVID fear tactics, governments have spent decades perfecting psychological operations against their own people.
Surveying the battlefield
For thousands of years, military strategists have understood that an army’s success often depends not on its size or even on its armaments but on its knowledge of the opponent.
After all, as Sun Tzu observes:
If you know the enemy and know yourself, you need not fear the result of a hundred battles. If you know yourself but not the enemy, for every victory gained you will also suffer a defeat. If you know neither the enemy nor yourself, you will succumb in every battle.
It follows, then, that the success of the globalists in their fifth-generation war on us all depends on their knowledge of humanity itself.
What makes people tick? What motivates and demotivates them? What stimuli do they respond to, and in what way do they respond?
From the viewpoint of those wishing to manipulate, control and subdue humanity, the knowledge of the human mind that can be gleaned from the answers to these questions is the most prized knowledge of all.
So, it shouldn’t be surprising to learn that not only scientific researchers but military planners and government officials have spent centuries trying to better understand humans and their behaviors – and, more importantly, how to mold, influence, shape, or outright control those behaviors.
Everyone knows about Ivan Pavlov’s experiments in conditioning. Any high schooler could tell you how Pavlov was able to condition dogs to salivate upon hearing the ringing of a dinner bell.
But how many know that Pavlov’s research didn’t end with his observation of canines? That he next began duplicating his experiments on human subjects? That those human experiments saw Pavlov and his protégé, Nikoli Krasnogorsky, scooping orphans off the streets, drugging them, surgically fitting them with salivation monitors and force-feeding them food so that these children, like Pavlov’s dogs, could be trained to salivate on command?

READ: Is the US Intelligence Community hiding secret weapons from the American public?
How many are familiar with the experimenters who followed in Pavlov’s footsteps? How many have seen the footage of John B. Watson’s “Little Albert” experiments, where the psychologist deliberately traumatized an 11-month-old baby in an attempt to refine the techniques of conditioning humans?
How many have read Watson himself bragging that “[a]fter conditioning, even the sight of the long whiskers of a Santa Claus mask sends the youngster scuttling away, crying and shaking his head from side to side”?

How many have followed the thread from Pavlov and Watson and the “classical conditioning” researchers to the “radical behaviorists” like B. F. Skinner and his work in perfecting operant conditioning?
How many have read Skinner’s Walden Two, in which he proposes a scheme for creating a utopian society by conditioning children from birth to assume specific roles in society?
By this point, it’s fairly common knowledge that the CIA conducted mind control experiments like Project MKUltra, using operatives like Sidney Gottlieb and Dr. Ewan Cameron to administer LSD to unwitting subjects and conduct other ghoulish experiments in mental manipulation. But how many have heard of MKSearch or MKChickwit or MKOften or any of the other spin-offs of this nightmarish research?
How many know these experiments “were designed to destabilize human personality by creating behavior disturbances, altered sex patterns, aberrant behavior using sensory deprivation and various powerful stress-producing chemicals, and mind-altering substances” and were carried out on so-called “expendables” – i.e., “people whose death or disappearance would arouse no suspicion”?
How many have heard of George Brock Chisholm, who served as the first Director-General of the World Health Organization and helped spearhead the World Federation for Mental Health? How many have read the transcript of his 1945 lecture, “The Reestablishment of Peacetime Psychiatry,” in which he declared, “If the race is to be freed from its crippling burden of good and evil it must be psychiatrists who take the original responsibility”?
And how many are aware that Chisholm’s call to action was heeded by men like British military psychiatrist Colonel John Rawlings Rees, the first president of Chisholm’s World Federation of Mental Health and chair of the infamous Tavistock Institute from 1933 to 1947?
How many know the story of how Dr. Jim Mitchell – a military retiree and psychologist who had contracted to provide training services to the CIA – took the findings of Dr. Martin Seligman on the psychological phenomenon of “learned helplessness” and weaponized them for the CIA in the service of the agency’s post-9/11 illegal torture program?
Whether the general public is aware of this documented history or not, the record shows that the last 125 years of research into the human psyche has been conducted – or at least weaponized – by Machiavellian manipulators and secret schemers whose intent is to socially engineer the masses.
And, as the science of the mind progresses in the 21st century, these social engineering schemes are only getting more effective.
The information war
The alternative media has certainly had cause to note that we here in the 21st century are the (largely unwitting) targets of a large-scale information war. This war is being waged upon us largely (though not exclusively) by our own governments.
Occasionally, stories of some of the campaigns in this war break through the information blockade, and the public catches a glimpse of the battle that is being waged against them on all fronts.
Bemused Canadians, for example, were able to read about the Canadian military’s bizarre “wolf letter” psyop in the pages of The Ottawa Citizen back in 2021. But any concerns that might have been raised by this psyop and its wild story of forged government letters and recorded wolf noises were soon quelled by the usual establishment lapdog journalists.
The whole thing, we were told, was caused by “a handful of military reservists testing psychological tactics at a weekend exercise” and “new control measures are now in place to ensure psychological operation exercises and influence activities do not reach unintended audiences” – so, obviously there’s nothing more to worry about!
Residents of the U.K., meanwhile, got their own glimpse of the infowar in 2021 when members of the Scientific Pandemic Influenza Group on Behaviour (SPI-B) – a group providing “independent, expert, social and behavioural science advice” to the U.K. government – admitted they were guilty of “using fear as a means of control.”
Tasked with providing insight on how to make Britons compliant with their government’s lockdown, social distancing, masking, and other restrictions at the beginning of the scamdemic, the SPI-B experts urged the government to increase “the perceived level of personal threat” from COVID-19. Multiple members of the SPI-B team later expressed regret about the scheme, calling it “totalitarian” and unethical.
One SPI-B member confessed: “You could call psychology ‘mind control.’ That’s what we do.”
Another put it even more bluntly: “Without a vaccine, psychology is your main weapon … Psychology has had a really good epidemic, actually.”
But to the extent that these operations ever come to public light, it is almost always in disconnected and decontextualized stories like these. Those Canadians who learned about the “wolf letter” psyop, for example, likely never read about the SPI-B scamdemic psyop, let alone connected the events together as evidence of the all-out infowar.
In recent years, however, the existence of the infowar has not only become undeniable. It is undenied.
The cognitive domain of the information battlespace
In 2022, the Associated Press published “‘Pre-bunking’ shows promise in fight against misinformation,” an article touting new research that claims to show progress in the creation of new weapons in the information war.
After detailing the usual examples of the scourge of “misinformation” – i.e., observations that erode public faith in “democratic institutions, journalism and science” – the article then reports uncritically on new techniques that are being developed to trick the public into once again trusting these demonstrably untrustworthy institutions:
New findings from university researchers and Google, however, reveal that one of the most promising responses to misinformation may also be one of the simplest.
In a paper published Wednesday in the journal Science Advances, the researchers detail how short online videos that teach basic critical thinking skills can make people better able to resist misinformation.
The researchers created a series of videos similar to a public service announcement that focused on specific misinformation techniques – characteristics seen in many common false claims that include emotionally charged language, personal attacks or false comparisons between two unrelated items.
Researchers then gave people a series of claims and found that those who watched the videos were significantly better at distinguishing false information from accurate information.
Although research like that touted by the AP is ostensibly civilian in nature, the fact that this information campaign is part of a literal military battle that is being waged against us is now starting to be admitted, as well.
In 2023, for example, the Japanese military officially added the “cognitive domain” as the latest new battle domain added to Japan’s National Defense Program Guideline. In addition to the traditional domains of territorial land, water, and airspace, and to newly added domains like space, cyberspace, and the electrogmagnetic domain, Japan’s defense authorities now claim the cognitive space as part of their remit.
According to The Global Times:
The building of such cognitive capability would also be written into the National Security Strategy, one of the three major diplomatic and security documents to be amended before the end of 2022, VOA Chinese reported, citing the theory that the Japanese defense authorities and the Self-Defense Force attach great importance to the “misinformation” released by Russia and China, consider that information spread in the Chinese language is a global trend and that cognitive warfare by the island of Taiwan against the Chinese mainland provides valuable experience for research and study.
[…]
Analysts said that cognitive warfare is a combination of digital information, media and spy technology that leads public opinion to extremes in order to affect the basis of diplomacy between countries and to realize the goals of political manipulation, citing the U.S.’ infamous “peaceful transfer of power” strategy in other countries as an example.
The recognition of the “cognitive domain” as a literal battlefield is not limited to the Japanese defense forces, however.
In 2019, the Chinese State Council Information Office released a white paper on “China’s National Defense in the New Era,” arguing that “[w]ar is evolving in form towards informationized [sic] warfare, and intelligent warfare is on the horizon.”
In 2022, Motohiro Tsuchiya, a professor at Keio University, wrote an article on “Governing Cognitive Warfare” for Governing the Global Commons: Challenges and Opportunities for US-Japan Cooperation (a publication of the German Marshall Fund of the United States!) in which he warned that the threat of “intelligentized warfare” by China and other U.S. State Department bogeymen necessitated U.S. cooperation to “create and promote rules and norms that can effectively govern cyberwarfare.”
And, perhaps inevitably, it wasn’t long before it was discovered that the real threat in this new “cognitive domain” isn’t the ChiComs or the CRINKs or any other outside force, but… *drumroll, please*… online conspiracy theorists!
That’s right, in 2023, Tomoko Nagasako, a research fellow at The Sasakawa Peace Foundation, penned “The Threat of Conspiracy Theories in the Battle for the Cognitive Domain – A Consideration of the Status of Conspiracy Theories in Japan Based on Attempts at Regime Destruction Overseas.” As you might guess from that title, the article provides “an overview of the state of conspiracy theories overseas and in Japan,” details how these dastardly conspiracy theorists present a threat to national security “[f]rom the perspective of cognitive warfare,” and proposes countermeasures to address these grave dangers to the nation.
And what “conspiracy theories” does Nagasako cite in her piece? That there exists a “deep state” over and above the surface-level government, that the COVID vaccines were harmful, that the U.S. has conducted biological weapons research in Ukraine in recent years… you know, the usual harebrained ideas that only kooky conspiracy realists would even entertain.
Yes, for those who haven’t received the memo yet: there most certainly is a war for your mind. It certainly is taking place right now. It is being waged by militaries around the world. The target of these wars is, more often than not, these very militaries’ fellow countrymen.
To those who are just waking up to this war, you have my deepest sympathy. Realizing that you are a target in a battle you didn’t even know you were fighting in a “cognitive domain” you never even knew existed must be wildly disorienting, to say the least.
But here’s the bad news: new technologies are being developed that will make all of this history – from Pavlov to Skinner to Mitchell to SPI-B – and all of these secret operations – from MKUltra to MKChickwit – and all of these military campaigns – from Chisholm and Rees and the machinations of the Tavistock minions to the ChiComs and the Japanese and the development of cognitive warfare – seem like small potatoes.
As we shall see in a follow-up article, the technology to rewire the brain – quite literally – is already being tested and deployed. And, once these technologies are ready to be unleashed on the public, they may bring the age-old dream of the dictators for total domination of the human population to reality.
Reprinted with permission from the Corbett Report.
Daily Caller
Daily Caller EXCLUSIVE: Trump’s Broad Ban On Risky Gain-Of-Function Research Nears Completion


From the Daily Caller News Foundation
By Emily Kopp
President Donald Trump could sign a sweeping executive order banning gain-of-function research — research that makes viruses more dangerous in the lab — as soon as May 6, according to a source who has worked with the National Security Council on the issue.
The executive order will take a broad strokes approach, banning research amplifying the infectivity or pathogenicity of any virulent and replicable pathogen, according to the source, who requested anonymity to speak candidly about the anticipated executive action. But significant unresolved issues remain, according to the source, including whether violators will be subject to criminal penalties as bioweaponeers.
The executive order is being steered by Gerald Parker, head of the White House Office of Pandemic Preparedness and Response Policy, which has been incorporated into the NSC. Parker did not respond to requests for comment.
Dear Readers:
As a nonprofit, we are dependent on the generosity of our readers.
Please consider making a small donation of any amount here. Thank you!
In the process of drafting the executive order, Parker has frozen out the federal agencies that have for years championed gain-of-function research and staved off regulation — chiefly Anthony Fauci’s former institute, the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
The latest policy guidance on gain-of-function research, unveiled under the Biden administration in 2024, was previously expected to go into effect May 6. According to a March 25 letter cosigned by the American Society for Microbiology, the Association for Biosafety and Biosecurity International, and Council on Governmental Relations, organizations that conduct pathogen research have not received direction from the NIH on that guidance — suggesting the executive order would supersede the May 6 deadline.
The 2024 guidance altered the scope of experiments subject to more rigorous review, but charged researchers, universities and funding agencies like NIH with its implementation, which critics say disincentivizes reporting. Many scientists say that researchers and NIH should not be the primary entities conducting cost–benefit analyses of pandemic virus studies.
Parker previously served as the head of the National Science Advisory Board for Biosecurity (NSABB), a group of outside experts that advises NIH on biosecurity matters, and in that role recommended that Congress stand up a new government agency to advise on gain-of-function research. Former Centers for Disease Control and Prevention Director Robert Redfield has also endorsed moving gain-of-function research decision making out of the NIH to an independent commission.
“Given the well documented lapses in the NIH review process, policymakers should … remove final approval of any gain-of function research grants from NIH,” Redfield said in a February op-ed.
It remains to be seen whether the executive order will articulate carveouts for gain-of-function research without risks of harm such as research on non-replicative pseudoviruses, which can be used to study viral evolution without generating pandemic viruses.
It also remains to be seen whether the executive order will define “gain-of-function research” tightly enough to stand up to legal scrutiny should a violator be charged with a crime.
Risky research on coronaviruses funded by the NIH at the Wuhan Institute of Virology through the U.S. nonprofit EcoHealth Alliance typifies the loopholes in NIH’s existing regulatory framework, some biosecurity experts say.
Documents obtained through the Freedom of Information Act in 2023 indicated that EcoHealth Alliance President Peter Daszak submitted a proposal to the Pentagon in 2018 called “DEFUSE” describing gain-of-function experiments on viruses similar to SARS-CoV-2 but downplayed to his intended funder the fact that many of the tests would occur in Wuhan, China.
Daszak and EcoHealth were both debarred from federal funding in January 2025 but have faced no criminal charges.
“I don’t know that criminal penalties are necessary. But we do need more sticks in biosafety as well as carrots,” said a biosecurity expert who requested anonymity to avoid retribution from his employer for weighing in on the expected policy. “For instance, biosafety should be a part of tenure review and whether you get funding for future work.”
Some experts say that it is likely that the COVID-19 crisis was a lab-generated pandemic, and that without major policy changes it might not be the last one.
“Gain-of-function research on potential pandemic pathogens caused the COVID-19 pandemic, killing 20 million and costing $25 trillion,” said Richard Ebright, a Rutgers University microbiologist and longtime critic of high-risk virology, to the Daily Caller News Foundation. “If not stopped, gain-of-function research on potential pandemic pathogens likely will cause future lab-generated pandemics.”
-

 Daily Caller1 day ago
Daily Caller1 day agoTrump Executive Orders ensure ‘Beautiful Clean’ Affordable Coal will continue to bolster US energy grid
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoBREAKING from THE BUREAU: Pro-Beijing Group That Pushed Erin O’Toole’s Exit Warns Chinese Canadians to “Vote Carefully”
-
 Business1 day ago
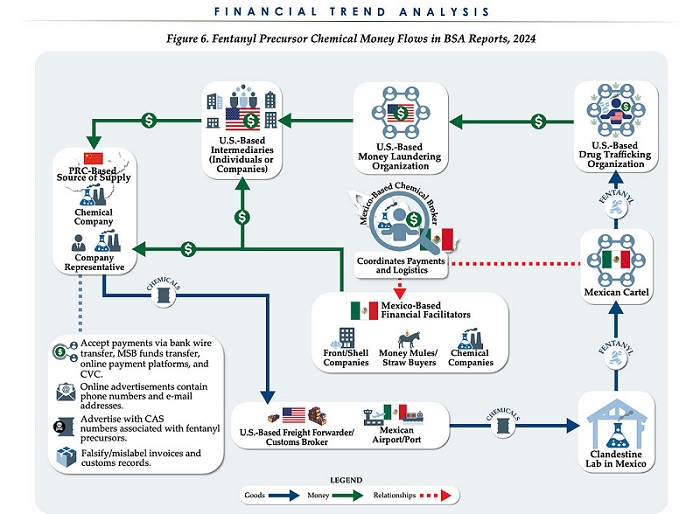
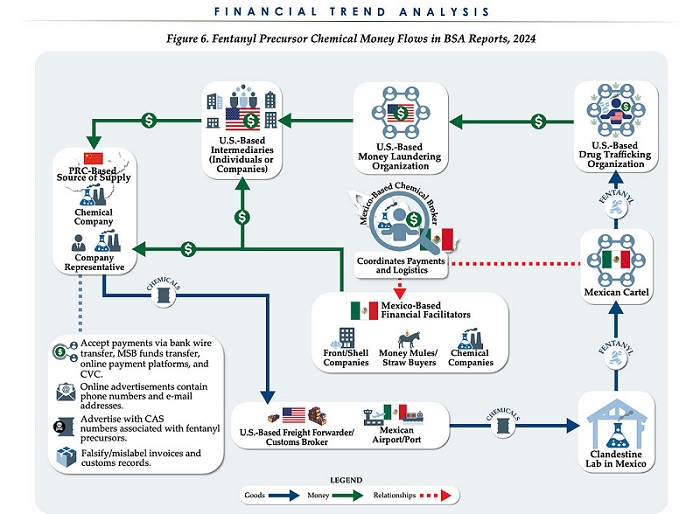
Business1 day agoChina, Mexico, Canada Flagged in $1.4 Billion Fentanyl Trade by U.S. Financial Watchdog
-

 COVID-191 day ago
COVID-191 day agoTamara Lich and Chris Barber trial update: The Longest Mischief Trial of All Time continues..
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoTucker Carlson Interviews Maxime Bernier: Trump’s Tariffs, Mass Immigration, and the Oncoming Canadian Revolution
-
 Energy1 day ago
Energy1 day agoStraits of Mackinac Tunnel for Line 5 Pipeline to get “accelerated review”: US Army Corps of Engineers
-
 2025 Federal Election1 day ago
2025 Federal Election1 day agoAllegations of ethical misconduct by the Prime Minister and Government of Canada during the current federal election campaign
-

 Business2 days ago
Business2 days agoDOGE Is Ending The ‘Eternal Life’ Of Government