Health
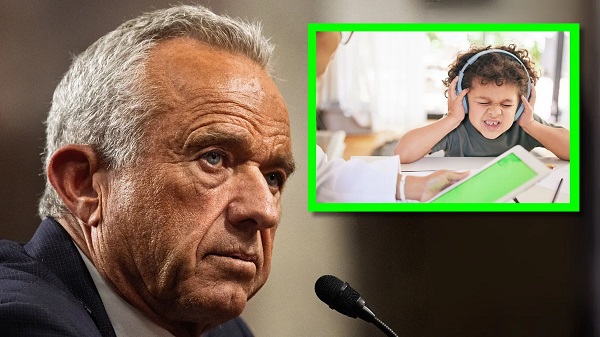
How the Trump-RFK Jr. coalition could realign US politics against Big Pharma and Big Food

From LifeSiteNews
By Jay Richards
If the unlikely coalition of Donald Trump and Robert F. Kennedy Jr. outlives the 2024 presidential election, it could reorder our political categories and leave to our children and grandchildren a quite different future.
When Robert F. Kennedy, Jr. endorsed Donald Trump on Aug. 23, the corporate press and conventional Washington, D.C., analysts mostly missed the real story: It was the moment that a disparate, diverse, and potentially disruptive throng of average Americans became a coalition.
Although RFK, Jr. is famous – or infamous, depending on your view – for his criticisms of vaccines, that wasn’t the theme of his lengthy speech. He spoke instead about an unholy alliance – a cartel – of industries, corporate media, government regulatory agencies, and even nonprofit “charities” that is making us fat and sick. This problem doesn’t fit the simple taxonomy of “public” and “private” or “left” and “right” that served us well during the Cold War.
Kennedy has been a voice in the wilderness warning about this cartel for years. Most Americans first became aware of it during the 2020 pandemic. Here’s the basic story: COVID-19 itself was likely the product of dangerous gain-of-function research conducted by the Wuhan Institute of Virology in China. That’s bad enough. But Communist China didn’t act alone. This work was funded, at least in part, by the U.S. government’s National Institutes of Health and laundered through the nonprofit EcoHealth Alliance.
Once the virus was out, the absurd and counterproductive lockdowns and hygiene theater were pushed by global entities such as the World Health Organization. Domestically, Francis Collins, then-head of the NIH, and Anthony Fauci, then-head of the National Institute of Allergy and Infectious Diseases, worked to undermine independent experts who criticized the federal bureaucrats’ favored policies.
Collins and Fauci even orchestrated the publication of a deceptive article in Nature that claimed the virus had a natural origin. The Centers for Disease Control and Prevention and other federal entities, including the Biden White House, pressured social media platforms to censor even the best-credentialed dissenters.
Attentive Americans soon learned that public health, as a field, focuses on nudging whole populations, rather than seeking the health of individual patients.
Certain pharmaceutical companies – which pay royalties to many NIH staff, including Collins and Fauci – enjoyed a suspiciously fast and less than rigorous approval process for their mRNA “vaccines.” Vaccine mandates then created a massive artificial market for the drugs. And drug companies’ immunity from legal liability allowed them to enjoy the financial benefits of these policies without facing the downside risks from any long-term harm to those who took the vaccines.
Then, during the lockdowns, the growing awareness of the “gender-industrial complex” – media, medical professionals, pharmaceutical companies, politicians, and others who push ghoulish “gender-affirming” interventions on people distressed about their sexed bodies – further reinforced the lack of credibility of private and public health authorities.
An American epidemic of chronic diseases
For some, much of this may now seem obvious. What may be less obvious is that blame for the massive spike in many chronic “diseases of civilization” should go to the same cartel. It involves Big Government, Big Food, Big Pharma, Big Media that rely on pharmaceutical industry ad dollars, and medical lobbying outfits such as the American Academy of Pediatrics pretending to be sound science crusaders.
In his speech, Kennedy devoted many paragraphs to the “chronic disease epidemic” – including ever higher rates, even among children, of Type II diabetes and obesity, and of Alzheimer’s, which some now refer to as “Type III diabetes.” He spoke of “the insidious corruption at the FDA and the NIH, the HHS and the USDA that has caused the epidemic,” referring to the Food and Drug Administration, the Department of Health and Human Services, and the U.S. Department of Agriculture, along with the NIH.
But he didn’t stop there. He spoke of “an explosion of neurological illnesses that I never saw as a kid,” including:
ADD, ADHD, speech delay, language delay, Tourette’s Syndrome, narcolepsy, ASD, Asperger’s, autism. In the year 2000, the Autism rate was one in 1500. Now, autism rates in kids are one in 36, according to CDC; nationally, nobody’s talking about this.
He also spoke of the massive spikes in the use of antidepressants and anti-anxiety drugs. Of course, first ladies and surgeons general have launched “healthy lifestyle” campaigns, but these always parrot the conventional wisdom of the cartel. In contrast, Kennedy blamed the cartel itself, not a gluttonous public, for the chronic disease crisis. It was this cartel that gave us the war on healthy dietary fats and the ridiculous food pyramid – heavy on unhealthy ultrarefined carbohydrates and light on fat – which helped make Americans far fatter and sicker than we were before.
His speech hit a nerve, especially among parents who recognize this problem but lack a credible and effective way to fight it. They may engage in private acts of defiance – refusing the COVID-19 or Hepatitis B vaccines for their young children, or disregarding USDA warnings about the consumption of animal fat. So far, however, neither political party has taken up this topic. The Left has tended to give the administrative state the benefit of the doubt. The Right has tended to do the same for corporations.
Trump has promised that Kennedy will have a leading role in fighting America’s health crisis. That will mean taking on the cartel. But the devil is in the details. A sustained effort to “make America healthy again,” or MAHA – to complement MAGA – must be free of government interests on the one hand and industry funding and lobbyists on the other.
Maybe that’s impossible, but Kennedy as MAHA czar could mean a serious exploration of the role the cartel has played in the following:
- Restricting medical freedom
- The origin of the COVID-19 virus
- The effects of the pandemic lockdowns
- The lack of safety and effectiveness of mRNA vaccines
- The rise in childhood and adult obesity
- The rise in childhood and adult Type II diabetes
- The rise in Alzheimer’s
- The rise in allergies, food sensitivities, and asthma
- Rising rates of depression and anxiety disorders
- Rising rates of neurological disorders such as autism
- The explosion of cases of childhood gender dysphoria
- The collusion between the World Professional Association of Transgender Health and HHS officials such as transgender activist and Assistant Secretary for Health Rachel Levine
- The political agenda of transnational public health bureaucracies such as the World Health Organization
- The medicalization of the treatment for gender dysphoria with “gender-affirming care” (rather than taking a mental health approach)
- The capitulation of NIH, CDC, FDA, and HHS to gender ideology over sound science
- The lack of value and safety of the ever-growing childhood vaccine schedule
- The medical focus on symptoms rather than underlying causes and cures of diseases
- The artificial restriction of medical and therapeutic credentialing of professionals to control supply and competition
- The decline in average testosterone in males
- The rise in infertility
- The rise in opioid addiction and overdose deaths
- Unethical research sponsored by the NIH
- The incompetence of the USDA in dispensing nutrition advice
- The effect of agricultural subsidies on our health
- Environmentalist dogmas masquerading as health and nutrition advice
If Trump appoints Kennedy as the MAHA czar, it would be akin to his COVID-19 Operation Warp Speed during his first administration but without the industry taint.
Of course, that appointment could come to nothing – except that there is already a coalition forming of millions of parents across, and even orthogonal to, the political spectrum, who – as Kennedy has put it – love their children more than they hate each other. It would take both the political will in Washington and a popular constituency of average Americans to fight the biomedical security state and the cartel that fuels it.
We’re getting a glimpse of this motley resistance in the unlikely unity ticket of Trump and Kennedy and the many strange bedfellows supporting them. If this coalition outlives the 2024 presidential election, it could reorder our political categories and leave to our children and grandchildren a quite different future.
Addictions
Addiction experts demand witnessed dosing guidelines after pharmacy scam exposed

By Alexandra Keeler
The move follows explosive revelations that more than 60 B.C. pharmacies were allegedly participating in a scheme to overbill the government under its safer supply program. The scheme involved pharmacies incentivizing clients to fill prescriptions they did not require by offering them cash or rewards. Some of those clients then sold the drugs on the black market.
An addiction medicine advocacy group is urging B.C. to promptly issue new guidelines for witnessed dosing of drugs dispensed under the province’s controversial safer supply program.
In a March 24 letter to B.C.’s health minister, Addiction Medicine Canada criticized the BC Centre on Substance Use for dragging its feet on delivering the guidelines and downplaying the harms of prescription opioids.
The centre, a government-funded research hub, was tasked by the B.C. government with developing the guidelines after B.C. pledged in February to return to witnessed dosing. The government’s promise followed revelations that many B.C. pharmacies were exploiting rules permitting patients to take safer supply opioids home with them, leading to abuse of the program.
“I think this is just a delay,” said Dr. Jenny Melamed, a Surrey-based family physician and addiction specialist who signed the Addiction Medicine Canada letter. But she urged the centre to act promptly to release new guidelines.
“We’re doing harm and we cannot just leave people where they are.”
Addiction Medicine Canada’s letter also includes recommendations for moving clients off addictive opioids altogether.
“We should go back to evidence-based medicine, where we have medications that work for people in addiction,” said Melamed.
‘Best for patients’
On Feb. 19, the B.C. government said it would return to a witnessed dosing model. This model — which had been in place prior to the pandemic — will require safer supply participants to take prescribed opioids under the supervision of health-care professionals.
The move follows explosive revelations that more than 60 B.C. pharmacies were allegedly participating in a scheme to overbill the government under its safer supply program. The scheme involved pharmacies incentivizing clients to fill prescriptions they did not require by offering them cash or rewards. Some of those clients then sold the drugs on the black market.
In its Feb. 19 announcement, the province said new participants in the safer supply program would immediately be subject to the witnessed dosing requirement. For existing clients of the program, new guidelines would be forthcoming.
“The Ministry will work with the BC Centre on Substance Use to rapidly develop clinical guidelines to support prescribers that also takes into account what’s best for patients and their safety,” Kendra Wong, a spokesperson for B.C.’s health ministry, told Canadian Affairs in an emailed statement on Feb. 27.
More than a month later, addiction specialists are still waiting.
According to Addiction Medicine Canada’s letter, the BC Centre on Substance Use posed “fundamental questions” to the B.C. government, potentially causing the delay.
“We’re stuck in a place where the government publicly has said it’s told BCCSU to make guidance, and BCCSU has said it’s waiting for government to tell them what to do,” Melamed told Canadian Affairs.
This lag has frustrated addiction specialists, who argue the lack of clear guidance is impeding the transition to witnessed dosing and jeopardizing patient care. They warn that permitting take-home drugs leads to more diversion onto the streets, putting individuals at greater risk.
“Diversion of prescribed alternatives expands the number of people using opioids, and dying from hydromorphone and fentanyl use,” reads the letter, which was also co-signed by Dr. Robert Cooper and Dr. Michael Lester. The doctors are founding board members of Addiction Medicine Canada, a nonprofit that advises on addiction medicine and advocates for research-based treatment options.
“We have had people come in [to our clinic] and say they’ve accessed hydromorphone on the street and now they would like us to continue [prescribing] it,” Melamed told Canadian Affairs.
A spokesperson for the BC Centre on Substance Use declined to comment, referring Canadian Affairs to the Ministry of Health. The ministry was unable to provide comment by the publication deadline.
Big challenges
Under the witnessed dosing model, doctors, nurses and pharmacists will oversee consumption of opioids such as hydromorphone, methadone and morphine in clinics or pharmacies.
The shift back to witnessed dosing will place significant demands on pharmacists and patients. In April 2024, an estimated 4,400 people participated in B.C.’s safer supply program.
Chris Chiew, vice president of pharmacy and health-care innovation at the pharmacy chain London Drugs, told Canadian Affairs that the chain’s pharmacists will supervise consumption in semi-private booths.
Nathan Wong, a B.C.-based pharmacist who left the profession in 2024, fears witnessed dosing will overwhelm already overburdened pharmacists, creating new barriers to care.
“One of the biggest challenges of the retail pharmacy model is that there is a tension between making commercial profit, and being able to spend the necessary time with the patient to do a good and thorough job,” he said.
“Pharmacists often feel rushed to check prescriptions, and may not have the time to perform detailed patient counselling.”
Others say the return to witnessed dosing could create serious challenges for individuals who do not live close to health-care providers.
Shelley Singer, a resident of Cowichan Bay, B.C., on Vancouver Island, says it was difficult to make multiple, daily visits to a pharmacy each day when her daughter was placed on witnessed dosing years ago.
“It was ridiculous,” said Singer, whose local pharmacy is a 15-minute drive from her home. As a retiree, she was able to drive her daughter to the pharmacy twice a day for her doses. But she worries about patients who do not have that kind of support.
“I don’t believe witnessed supply is the way to go,” said Singer, who credits safer supply with saving her daughter’s life.
Melamed notes that not all safer supply medications require witnessed dosing.
“Methadone is under witness dosing because you start low and go slow, and then it’s based on a contingency management program,” she said. “When the urine shows evidence of no other drug, when the person is stable, [they can] take it at home.”
She also noted that Suboxone, a daily medication that prevents opioid highs, reduces cravings and alleviates withdrawal, does not require strict supervision.
Kendra Wong, of the B.C. health ministry, told Canadian Affairs that long-acting medications such as methadone and buprenorphine could be reintroduced to help reduce the strain on health-care professionals and patients.
“There are medications available through the [safer supply] program that have to be taken less often than others — some as far apart as every two to three days,” said Wong.
“Clinicians may choose to transition patients to those medications so that they have to come in less regularly.”
Such an approach would align with Addiction Medicine Canada’s recommendations to the ministry.
The group says it supports supervised dosing of hydromorphone as a short-term solution to prevent diversion. But Melamed said the long-term goal of any addiction treatment program should be to reduce users’ reliance on opioids.
The group recommends combining safer supply hydromorphone with opioid agonist therapies. These therapies use controlled medications to reduce withdrawal symptoms, cravings and some of the risks associated with addiction.
They also recommend limiting unsupervised hydromorphone to a maximum of five 8 mg tablets a day — down from the 30 tablets currently permitted with take-home supplies. And they recommend that doses be tapered over time.
“This protocol is being used with success by clinicians in B.C. and elsewhere,” the letter says.
“Please ensure that the administrative delay of the implementation of your new policy is not used to continue to harm the public.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
Autism
RFK Jr. Completely Shatters the Media’s Favorite Lie About Autism
 The Vigilant Fox
The Vigilant Fox
They say autism is rising because of “better diagnosis”—but RFK Jr. just blew that narrative wide open. He brought the hard data and dropped one undeniable truth the denialists can’t explain.
HHS Secretary Robert Kennedy Jr. appeared on Hannity Thursday evening and unloaded on the predominant autism narrative. It started with a bombshell reveal from Kennedy’s own childhood.
Hannity asked: “What was the number when you were a kid—and what do you think is going on?”
Kennedy replied: “There’s really good data on that.”
He pointed to one of the largest studies ever conducted—900,000 children in Wisconsin, published in a top-tier medical journal.
“It looked at 900,000 kids. It was published in a high-gravitas journal, peer-reviewed study, and they found the rate to be 0.7 out of 10,000.”
That’s less than 1 in 10,000. Today? It’s around 1 in 31.
Let that sink in.
Join 110K+ Substack readers and 1.6 million 𝕏 users who follow the work of Vigilant Fox.
Subscribe for top-tier news aggregation and exclusive stories you won’t find anywhere else.
That’s when Kennedy sounded the alarm on what’s happening now—and why it’s so catastrophic. He said the rise isn’t just in frequency—it’s in severity.
“Two years ago, it was 1 in 36. The CDC data we released this week shows 1 in 31,” Kennedy said.
“The worst state is California,” Kennedy continued, “which actually has the best collection methodologies. So they actually, probably reflect what we’re seeing nationwide.”
“In California, it’s 1 in every 20 kids, and 1 in every 12.5 boys,” he explained.
Even worse, he said the numbers are likely underreported in minority communities. And for many kids, the symptoms are devastating:
“About 25% of the population of those kids with autism, about 25% of them are nonverbal, nontoilet trained,” Kennedy explained.
“They have all of these stereotypical behaviors, the head banging, biting, toe walking, stimming, and that population is growing higher and higher.”
“It’s becoming a larger percentage, so we’re seeing many more cases that are now linked to severe intellectual disability.”
He says it’s a glaring red warning sign—and it’s past time to start acting on it.
And this was the moment that Kennedy took a flamethrower to the media narrative about autism. He shattered the core excuse we’ve all been fed—that this epidemic isn’t real, that it’s just a change in how we count it.
He’s not buying it.
“The media has bought into this industry canard, this mythology, that we’re just seeing more autism because we’re noticing it more. We’re better at recognizing it or there’s been changing diagnostic criteria.”
But the scientific literature, Kennedy said, says otherwise.
“There is study after study in the scientific literature going back, and they decided that the literature going back says decades that says that’s not true.”
He then cited a major investigation by California’s own lawmakers.
“In fact, the California legislature… asked the Mind Institute at UC Davis to look exactly at that topic. They [asked], is it real or are we just noticing it more? The Mind Institute came back and said, ‘Absolutely this is a real epidemic. This is something we’ve never seen before.’”
And he made it painfully clear:
“Anybody with common sense, Sean, would notice that, because the autism—this epidemic is only happening in our children. It’s not happening in people who are our age. And if it was better recognition, you’d see it in 70-year-old men.”
But we don’t.
And after laying out the data, dismantling the media narrative, and exposing the severity of the crisis, Kennedy concluded with a clarion call to get to the bottom of this epidemic.
That’s why he says it’s time to dig deeper—leave no stone unturned, and we may have answers sooner than you think.
“President Trump asked me to find out what’s causing it,” he told Hannity.
“And I am approaching that agnostically. We are looking at everything, we are going to do, we’re going to be very transparent in how we design the studies.”
To get real answers, he’s farming the research out to top institutions across the country—with full transparency from day one.
“We’re going to farm the studies out to 15 premier research groups from all over the country. And we’re going to be transparent about our protocols, about the data sets, and then every study will have to be replicated.”
The list of possible factors is long—and nothing is being ruled out, Kennedy explained.
“We’re going to look at mold. We’re going to look at the age of parents. We’re going to look at food and food additives. We’re going to look at pesticides and toxic exposures. We’re going to look at medicines. We’re going to look at vaccines. We’re going to look at everything.”
When asked how long it would take, Kennedy didn’t miss a beat.
“I think we’ll have some preliminary answers in six months. It will take us probably a year from then before we can have definitive answers because a lot of the studies will not go out until the end of the summer.”
For the first time in decades, someone is asking the hard questions—and demanding real answers.
This time, nothing is off-limits.
Thanks for reading. If you value the work being published here, upgrading your subscription is the most powerful way to support it. The more this Substack earns, the more I can do to improve quality and create the best reader experience possible.
Thank you for your support.
-

 2025 Federal Election2 hours ago
2025 Federal Election2 hours agoBREAKING: THE FEDERAL BRIEF THAT SHOULD SINK CARNEY
-
 2025 Federal Election13 hours ago
2025 Federal Election13 hours agoReal Homes vs. Modular Shoeboxes: The Housing Battle Between Poilievre and Carney
-

 International1 day ago
International1 day agoPope Francis has died aged 88
-

 2025 Federal Election13 hours ago
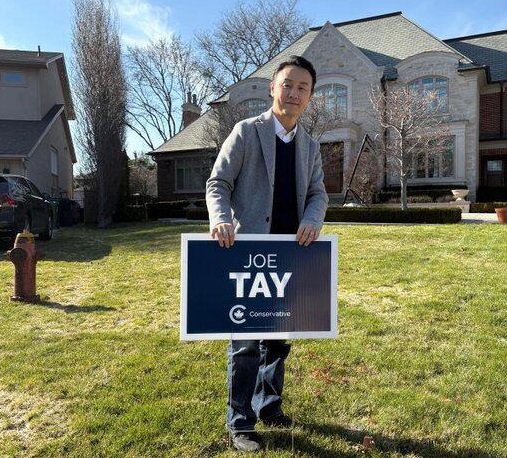
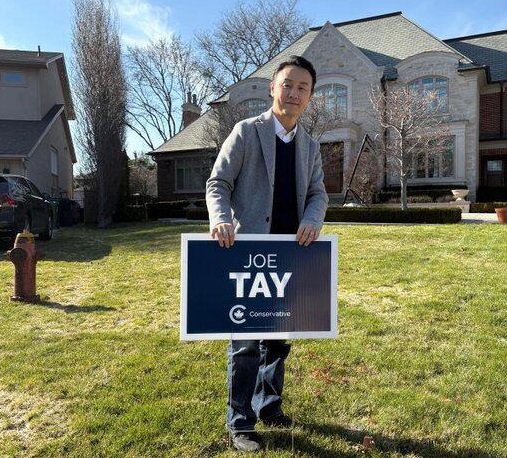
2025 Federal Election13 hours agoOttawa Confirms China interfering with 2025 federal election: Beijing Seeks to Block Joe Tay’s Election
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoCarney’s budget means more debt than Trudeau’s
-
 2025 Federal Election3 hours ago
2025 Federal Election3 hours agoCHINESE ELECTION THREAT WARNING: Conservative Candidate Joe Tay Paused Public Campaign
-

 2025 Federal Election13 hours ago
2025 Federal Election13 hours agoHow Canada’s Mainstream Media Lost the Public Trust
-

 Business1 day ago
Business1 day agoCanada Urgently Needs A Watchdog For Government Waste









