Opinion
High school calls police, bans parents from soccer games for silently supporting girls-only teams

From LifeSiteNews
The ‘No Trespass’ order alleged that parents wearing the pink wristbands ‘had the effect of intimidating, threatening, harassing, and discouraging’ the boy playing on the opposing girls team.
A New Hampshire high school halted a girls soccer game last week and called the police after parents, who were dismayed about a female-identifying male playing on the opposing team, were found to be wearing pink wristbands as a means of silent, peaceful protest.
Two parents subsequently received a notice from the superintendent of schools banning them from attending their daughters’ future games, asserting that by distributing the pink wristbands, which carried the simple message, “XX” (referring to the two chromosomes indicating the female sex), had the effect of “intimidating, threatening, harassing, and discouraging” the boy playing on the opposing girls team.
A NO TRESPASS order from Superintendent Mary Kelley sent to parent Anthony Foote of Bow, New Hampshire, alleges that “prior to and during the soccer game,” he “brought and distributed pink armbands to parents and other attendees to protest the participation of a transgender female student on the other team.”
“You are hereby prohibited from entering the buildings, grounds, and property of the Bow School District, including but not limited to all school administrative office buildings, parking lots, and athletic fields, until further notice,” the terse notice declared.
“You are also prohibited from attending any Bow School District athletic or extra-curricular event, on or off school grounds.”
“My daughter’s playing in the homecoming game this weekend, and I’m banned until the 23rd,” Foote told the NHJournal. “I can’t watch her play in homecoming — which is ridiculous.”
Foote told the NHJournal that he doesn’t care about what Parker Tirrell, the male student playing on the rival team, wants to do with his life.
“What I do care about is that my daughter could be physically hurt, maybe not by Parker because he’s not the biggest kid on the field. But there’s a chance that next time will be different,” Foote said.
Gov. Chris Sununu had signed the Fairness in Women’s Sports Act into law in July, making the Granite State the 26th state to keep males from participating in girls’ sports events.
However, U.S. District Court Judge Landya McCafferty prevented the law from being enforced.
“Judge Landya McCafferty”s ruling has settled the question of allowing males to compete as girls for the moment … but the issue of free speech is not resolved,” NHJournal’s Michael Graham noted. “It’s possible the school’s treatment of these parents violates their First Amendment rights, or that the school district’s interpretation of what is ‘disruptive behavior’ could be viewed by a court as too expansive.”
Foote also said he’s concerned that social pressure may prevent a large number of parents from expressing their views about the matter of boys competing in girls’ sports.
“Bow is a very blue town, and the people who run things will defend any liberal issue. It’s hard to speak out. But I would say there’s a silent majority,” Foote said. “There are firemen, there are police officers, there are teachers from other towns. They don’t agree, but they have to think about their finances. They have to protect their families. They can’t say anything.”
Parental concerns about their daughters being injured by males playing on what not so long ago were “female only” sports teams are by no means unfounded.
In nearby Massachusetts earlier this year, a gender-confused male playing on a girls high school basketball team injured three female players, causing the remaining female teammates to fear for their safety.
The Daily Item reported that Collegiate Charter School of Lowell ended its February 8 game against the KIPP Academy girls basketball team after just 16 minutes due to the KIPP team’s inclusion of a male player reportedly six feet tall with facial hair.
Earlier this year, LifeSiteNews’ Calvin Freiburger explained:
Inclusion of gender-confused individuals in opposite-sex sports is promoted by leftists as a matter of “inclusivity,” but critics note that indulging “transgender” athletes undermines the original rational basis for having sex-specific athletics in the first place, thereby depriving female athletes of recognition and professional or academic opportunities.
There have been numerous high-profile examples in recent years of men winning women’s competitions, and research affirms that physiology gives males distinct athletic advantages that cannot be fully negated by hormone suppression.
In a 2019 paper published by the Journal of Medical Ethics, New Zealand researchers found that “healthy young men (do) not lose significant muscle mass (or power) when their circulating testosterone levels were reduced to (below International Olympic Committee guidelines) for 20 weeks” and “indirect effects of testosterone” on factors such as bone structure, lung volume, and heart size “will not be altered by hormone therapy;” therefore, “the advantage to transwomen (biological men) afforded by the (International Olympic Committee) guidelines is an intolerable unfairness.”
armed forces
Carney’s ‘Shared Sacrifice’ Is a Lie. Only Veterans Are Bleeding for This Budget

How the 2025 Federal Budget Demands More From Those Who’ve Already Given Everything
I’ve lived the word sacrifice.
Not the political kind that comes in speeches and press releases the real kind. The kind Mark Carney wouldn’t know if it slapped him in the face. The kind that costs sleep, sanity, blood. I’ve watched friends trade comfort for duty, and I’ve watched some of them leave in body bags while the rest of us carried the weight of their absence. So when the Prime Minister stood up this year and told Canadians the new budget would “require sacrifice,” I felt that familiar tightening in the gut the one every veteran knows. You brace for impact. You hope the pain lands in a place that makes sense.
It didn’t.
Kelsi Sheren is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Six months into Mark Carney’s limp imitation of leadership, it’s painfully clear who’s actually paying the bill. The 2025 budget somehow managing to bleed the country dry while still projecting a $78-billion deficit shields the political class, funnels money toward his network of insiders, and then quietly hacks away at the one department that should be sacrosanct: Veterans Affairs Canada.
If there’s one group that’s earned the right to be spared from government-imposed scarcity, it’s the people who carried this country’s flag into danger. Veterans don’t “symbolize” sacrifice they embody it on the daily And when Ottawa tightens the belt on VAC, the consequences aren’t abstract. They’re brutal and direct, causing nothing but more death and destruction. But Mark Carney doesn’t lose sleep over veterans killing themselves.
Punishment disguised as budgeting for a veteran means the difference between keeping a roof or sleeping in a truck. Punishment disguised as budgeting means PTSD left untreated until it turns a human being into another suicide statistic. Punishment disguised as budgeting means a veteran choosing between groceries and medication because some number-shuffler in Ottawa wants to pretend they’re being “responsible.”
This isn’t fiscal restraint it’s political betrayal wrapped in government stationery. Ottawa sells it as hard choices, but the hardness always falls on the backs of the same people: the ones who already paid more than their share, the ones who can’t afford another hit. Carney and his cabinet won’t feel a thing. Not one missed meal. Not one sleepless night. Not one flashback.
But the men and women who already paid in flesh? They’re the ones being told to give more.
That’s not sacrifice.
That’s abandonment dressed up as fiscal policy.
And Canadians need to recognize it for what it is a government that demands loyalty while refusing to give any in return. The fine print in the government’s own documents reveals what the slogans won’t.
Over the next two years, VAC plans to cut $2.227 billion from its “Benefits, Services and Support” programs. [2] Broader “savings initiatives” reach $4.4 billion over four years, much of it through reductions to the medical-cannabis program that thousands of veterans rely on to manage chronic pain and PTSD. [3] Independent analysts estimate yearly losses of roughly $900 million once the cuts are fully implemented. [4]
To put that in perspective: no other department is seeing reductions on this scale. Not Defence, not Infrastructure, not the Prime Minister’s Office thats for damn sure. Only the people who’ve already paid their debt to this country are being asked to give again.
The government’s line is tidy: “We’re not cutting services we’re modernizing. Artificial Intelligence will streamline processing and improve efficiency.”
That sounds fine until you read the departmental notes. The “modernization” translates into fewer human case managers, longer waits, and narrower eligibility. It’s austerity dressed up as innovation. I’ve coached veterans through the system. They don’t need algorithms; they need advocates who understand trauma, identity loss, and the grind of reintegration. They need empathy, not automation.
This isn’t abstract accounting. Behind every dollar is a life on the edge, the human cost and toll is very real.
- Homelessness: Veterans make up a disproportionate number of Canada’s homeless population. Cutting benefits only deepens that crisis.
- Mental Health: Parliament’s ongoing study on veteran suicide shows rising rates of despair linked to delays and denials in VAC services. [5] Knowing MAID for mental illness alone in 2027 will take out a significant amount of us.
- Food Insecurity: A 2024 VAC survey found nearly one in four veterans reported struggling to afford basic groceries. That’s before these cuts.
We talk about “service” like it ends with deployment. It doesn’t. Service continues in how a nation cares for those who carried its battles, and this doesn’t include the cannabis cut to medication or the fight’s we have to fight when they tell us our injuries are “not service related”
The insult is magnified by the timing. These cuts were announced just days before November 11 Remembrance Day, when Canadians bow their heads and say, “We will remember them.”
Apparently, the government remembered to draft the talking points but forgot the meaning behind them, not a single one of the liberal government should have been allowed to show their faces to veteran’s or at a ceremony. They’re nothing but liars, grifters and traitors to this nation. Yes I’m talking about Jill McKnight and Mark Carney.
The budget still runs the second-largest deficit in Canadian history. [6]
Veteran cuts don’t fix that. They barely dent it. What they do is let the government say it’s “finding efficiencies” while avoiding the real structural overspending that created the problem in the first place. When a government chooses to protect its pet projects and insider contracts while pulling support from veterans, that’s not fiscal discipline it’s moral cowardice. The worst part is that This isn’t an isolated move. It fits a six-month pattern: large, attention-grabbing announcements about “reform,” followed by fine print that concentrates power and shifts burden downward. Veterans just happen to be the first visible casualty.
The same budget expands spending in other politically convenient areas green-transition subsidies, digital-governance infrastructure, and administration while the people who once embodied service are told to tighten their belts.
As a combat veteran, I know what it’s like to come home and realize that the fight didn’t end overseas it just changed terrain. We fought for freedom abroad only to watch bureaucratic neglect wage a quieter war here at home. Veterans don’t ask for privilege. They ask for respect, for competence, for follow-through on the promises this country made when it sent them into harm’s way.
Here’s what really needs to change, the liberal government has to go, thats step one. Restore VAC funding immediately. Any “savings” plan that touches benefits, services, or support should be scrapped. End the AI façade. Efficiency can’t replace empathy. Keep human case workers who understand the veteran experience. Audit and transparency. Publish a detailed breakdown of where VAC funds are cut and who approved it. Canadians deserve to see the receipts. National accountability. Every MP who voted for this budget should face veterans in their constituency and explain it, face-to-face.
Budgets are moral documents. They show what a country values. By slashing VAC while running record deficits, this government declared that veterans are expendable line items, not national obligations. The Prime Minister promised “shared sacrifice.” But the only people truly sacrificing are the ones who already gave more than most Canadians ever will.
Sacrifice isn’t about spreadsheets; it’s about service. It’s what every veteran understood when they raised their right hand. This government’s brand of sacrifice asking wounded soldiers to pay for political mismanagement isn’t austerity. It’s abandonment.
Canada owes its veterans more than a wreath once a year. It owes them respect written into every budget, not erased from it.
KELSI SHEREN
Footnotes
[1] The Guardian, “Canada’s 2025 Federal Budget Adds Tens of Billions to Deficit as Carney Spends to Dampen Tariffs Effect,” Nov 5 2025.
[2] True North Wire, “Liberal Budget to Cut $4.23 Billion from Veterans Affairs,” Nov 2025.
[3] StratCann, “Budget 2025 Includes Goal of Saving $4.4 Billion in Medical Cannabis Benefits,” Nov 2025.
[4] Canadian Centre for Policy Alternatives, “Where Will the Federal Government Cut to Pay for Military Spending and Tax Cuts?” Nov 2025.
[5] House of Commons Standing Committee on Veterans Affairs, “Study on Veteran Suicide and Sanctuary Trauma,” ongoing 2025.
[6] CBC News, “Federal Budget 2025 Deficit Second Largest in Canadian History,” Nov 2025.
Kelsi Sheren is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Artificial Intelligence
Trump’s New AI Focused ‘Manhattan Project’ Adds Pressure To Grid

From the Daily Caller News Foundation
Will America’s electricity grid make it through the impending winter of 2025-26 without suffering major blackouts? It’s a legitimate question to ask given the dearth of adequate dispatchable baseload that now exists on a majority of the major regional grids according to a new report from the North American Electric Reliability Corporation (NERC).
In its report, NERC expresses particular concern for the Texas grid operated by the Electric Reliability Council of Texas (ERCOT), where a rapid buildout of new, energy hogging AI datacenters and major industrial users is creating a rapid increase in electricity demand. “Strong load growth from new data centers and other large industrial end users is driving higher winter electricity demand forecasts and contributing to continued risk of supply shortfalls,” NERC notes.
Texas, remember, lost 300 souls in February 2021 when Winter Storm Uri put the state in a deep freeze for a week. The freezing temperatures combined with snowy and icy conditions first caused the state’s wind and solar fleets to fail. When ERCOT implemented rolling blackouts, they denied electricity to some of the state’s natural gas transmission infrastructure, causing it to freeze up, which in turn caused a significant percentage of natural gas power plants to fall offline. Because the state had already shut down so much of its once formidable fleet of coal-fired plants and hasn’t opened a new nuclear plant since the mid-1980s, a disastrous major blackout that lingered for days resulted.
Dear Readers:
As a nonprofit, we are dependent on the generosity of our readers.
Please consider making a small donation of any amount here.
Thank you!
This country’s power generation sector can either get serious about building out the needed new thermal capacity or disaster will inevitably result again, because demand isn’t going to stop rising anytime soon. In fact, the already rapid expansion of the AI datacenter industry is certain to accelerate in the wake of President Trump’s approval on Monday of the Genesis Mission, a plan to create another Manhattan Project-style partnership between the government and private industry focused on AI.
It’s an incredibly complex vision, but what the Genesis Mission boils down to is an effort to build an “integrated AI platform” consisting of all federal scientific datasets to which selected AI development projects will be provided access. The concept is to build what amounts to a national brain to help accelerate U.S. AI development and enable America to remain ahead of China in the global AI arm’s race.
So, every dataset that is currently siloed within DOE, NASA, NSF, Census Bureau, NIH, USDA, FDA, etc. will be melded into a single dataset to try to produce a sort of quantum leap in AI development. Put simply, most AI tools currently exist in a phase of their development in which they function as little more than accelerated, advanced search tools – basically, they’re in the fourth grade of their education path on the way to obtaining their doctorate’s degree. This is an effort to invoke a quantum leap among those selected tools, enabling them to figuratively skip eight grades and become college freshmen.
Here’s how the order signed Monday by President Trump puts it: “The Genesis Mission will dramatically accelerate scientific discovery, strengthen national security, secure energy dominance, enhance workforce productivity, and multiply the return on taxpayer investment into research and development, thereby furthering America’s technological dominance and global strategic leadership.”
It’s an ambitious goal that attempts to exploit some of the same central planning techniques China is able to use to its own advantage.
But here’s the thing: Every element envisioned in the Genesis Mission will require more electricity: Much more, in fact. It’s a brave new world that will place a huge amount of added pressure on power generation companies and grid managers like ERCOT. Americans must hope and pray they’re up to the task. Their track records in this century do not inspire confidence.
David Blackmon is an energy writer and consultant based in Texas. He spent 40 years in the oil and gas business, where he specialized in public policy and communications.
-

 COVID-191 day ago
COVID-191 day agoCrown seeks to punish peaceful protestor Chris Barber by confiscating his family work truck “Big Red”
-

 Agriculture18 hours ago
Agriculture18 hours agoHealth Canada indefinitely pauses plan to sell unlabeled cloned meat after massive public backlash
-

 MAiD2 days ago
MAiD2 days agoHealth Canada suggests MAiD expansion by pre-approving ‘advance requests’
-

 Alberta1 day ago
Alberta1 day agoPremier Danielle Smith says attacks on Alberta’s pro-family laws ‘show we’ve succeeded in a lot of ways’
-

 Indigenous1 day ago
Indigenous1 day agoCanadian mayor promises to ‘vigorously defend’ property owners against aboriginal land grab
-
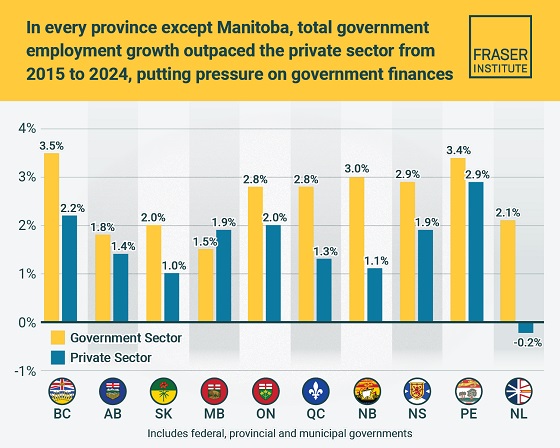
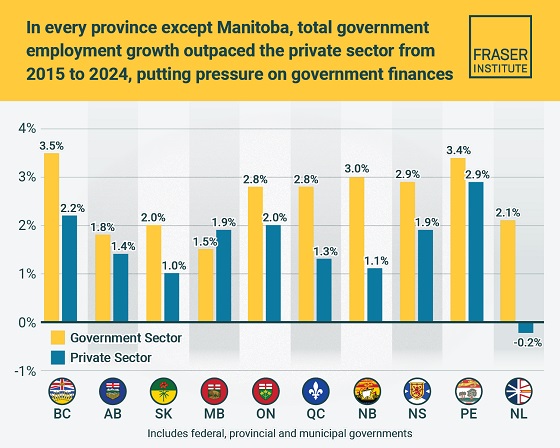 Business2 days ago
Business2 days agoTaxpayers paying wages and benefits for 30% of all jobs created over the last 10 years
-

 Health1 day ago
Health1 day agoOrgan donation industry’s redefinitions of death threaten living people
-

 Daily Caller2 days ago
Daily Caller2 days agoEXCLUSIVE: Here’s An Inside Look At The UN’s Disastrous Climate Conference