Fraser Institute
Enough talk, we need to actually do something about Canadian health care

From the Macdonald Laurier Institute
By J. Edward Les for Inside Policy
Canada spends more on health care as a percentage of GDP than almost all other OECD countries, yet we rank behind most of them when it comes to outcomes that matter.
I drove a stretch of road near Calgary’s South Health Campus the other day, a section with a series of three intersections in a span of less than a few hundred metres. That is, I tried to drive it – but spent far more time idling than moving.
At each intersection, after an interminable wait, the light turned green just as the next one flipped to red, grinding traffic to a halt just after it got rolling. It was excruciating; I’m quite sure I spied a snail on crutches racing by – no doubt making a beeline (snail-line?) for the ER a stone’s throw away.
The street’s sluggishness is perhaps reflective of the hospital next to it, given that our once-cherished universal health care system has crumbled into a universal waiting system – a system seemingly crafted (like that road) to obstruct flow rather than enable it. In fact, the pace of medical care delivery in this country has become so glacial that even a parking lot by comparison feels like the Indianapolis Speedway.
The health care crisis grows more dire by the day. Reforms are long overdue. Canada spends more on health care as a percentage of GDP than almost all other OECD countries, yet we rank behind most of them when it comes to outcomes that matter.
And we’re paying with our lives: according to the Canadian Institute for Health Information, thousands of Canadians die each and every year because of the inefficiencies of our system.
Yet for all that we are paralyzed by the enormity and complexity of the mushrooming disaster. We talk about solutions – and then we talk and talk some more. But for all the talking, precious little action is taken.
I’m reminded of an Anne Lamotte vignette, related in her bestselling book Bird By Bird:
Thirty years ago my older brother, who was ten years old at the time, was trying to get a report written on birds that he’d had three months to write, which was due the next day. We were out at our family cabin in Bolinas, and he was at the kitchen table close to tears, surrounded by binder paper and pencils and unopened books about birds, immobilized by the hugeness of the task ahead. Then my father sat down beside him, put his arm around my brother’s shoulder, and said, “Bird by bird, buddy. Just take it bird by bird.”
So it is with Canadian health care: we’ve wasted years wringing our hands about the woeful state of affairs, while doing precious little about it.
Enough procrastinating. It’s time to tackle the crisis, bird by bird.
One thing we can do is to let doctors be doctors. A few weeks ago, in a piece titled “Should Doctors Mind Their Own Business?”, I questioned the customary habit of doctors hanging out their shingles in small independent community practices. Physicians spend long years of training to master their craft, years during which they receive no training in business methods whatsoever, and then we expect them to master those skills off to the side of their exam rooms. Some do it well, but many do not – and it detracts from their attention to patients.
We don’t install newly minted teachers in classrooms and at the same time task them with the keeping the lights on, managing the supply chain, overseeing staffing and payroll, and all the other mechanics of running schools. Why do we expect that of doctors?
Keeping doctors embedded within large, expensive, inefficient, bureaucracy-choked hospitals isn’t the solution, either.
There’s a better way, I argued in my essay: regional medical centres – centres built and administered in partnership with the private sector.
Such centres would allow practitioners currently practicing in the community to ply their trade unencumbered by the nuts and bolts of running a business; and they would allow us to decant a host of services from hospitals, which should be reserved for what only hospitals can do: emergency services, inpatient care, surgeries, and the like.
In short, we should let doctors be doctors, and hospitals be hospitals.
To garner feedback, I dumped my musings into a couple of online physician forums to which I belong, tagged with the query: “Food for thought, or fodder for the compost bin?”
The verdict? Hands down, the compost bin.
I was a bit taken aback, initially. Offended, even – because who among us isn’t in love with their own ideas?
But it quickly became evident from my peers’ comments that I’d been misunderstood. Not because my doctor friends are dim, but because I hadn’t been clear.
When I proposed in my essay that we “leave the administration and day-to-day tasks of running those centres to business folks who know what they’re doing,” my colleagues took that to mean that doctors would be serving at the beck and call of a tranche of ill-informed government-enabled administrators – and they reacted to the notion with anaphylactic derision. And understandably so: too many of us have long and painful experience with thick layers of health care bureaucracy seemingly organized according to the Peter Principle, with people promoted to – and permanently stuck at – the level of their incompetence.
But I didn’t mean to suggest – not for a minute – that doctors shouldn’t be engaged in running these centres. I also wrote: “None of which is to suggest that doctors shouldn’t be involved, by aptitude and inclination, in influencing the set-up and management of regional centres – of course, they should.”
Of course they should. There are plenty of physicians equipped with both the skills and interest needed to administer these centres; and they should absolutely be front and centre in leading them.
But more than that: everyone should have skin in the game. All workers have the right to share in the success of an enterprise; and when they do, everybody wins. When everyone is pulling in the same direction because everyone shares in the wins, waste and inefficiencies are rooted out like magic.
Contrast that to how hospitals are run, with scarcely anyone aware of the actual cost of the blood tests or CT scans they order or the packets of suture and gauze they rip open, and with the motivations of administrative staff, nurses, doctors, and other personnel running off in more directions than a flock of headless chickens. The capacity for waste and inefficiencies is almost limitless.
I don’t mean to suggest that the goal of regional medical centres should be to turn a profit; but fiscal prudence and economic accountability are to be celebrated, because money not wasted is money that can be allocated to enhancing patient care.
Nor do I mean to intimate that sensible resource management should be the only parameter tracked; patient outcomes and patient satisfaction are paramount.
What should government’s role be in all this? Initially, to incentivize the creation of these centres via public-private partnerships; and then, crucially, to encourage competition among them and to reward innovation and performance, with optimization of the three key metrics – patient outcomes, patient satisfaction, and economic accountability – always in focus.
No one should be mandated to work in non-hospital regional medical centres. It’s a free country (or it should be): doctors should be free to hang out their own community shingles if they wish. But if we build the model correctly, my contention is that most medical professionals will prefer to work collaboratively under one roof with a diverse group of colleagues, unencumbered by the mundanities of running a business, but also free of choking hospital bureaucracy.
I connected a couple weeks ago with the always insightful economist Jack Mintz (who is also a distinguished fellow at the Macdonald-Laurier Institute). Mintz sits on the board of a Toronto-area hospital and sees first-hand “the problems with the lack of supply, population growth, long wait times between admission and getting a bed, emergency room overuse,” and so on.
“Something has to give,” he said. “Probably more resources but better managed. We really need major reform.”
On that we can all agree. We can’t carry on this way.
So, let’s stop idling; and let’s green-light some fixes.
As Samwise Gamgee said in The Lord of the Rings, “It’s the job that’s never started as takes longest to finish.”
Dr. J. Edward Les is a pediatrician in Calgary who writes on politics, social issues, and other matters.
Business
Clean energy transition price tag over $150 billion and climbing, with very little to show for it

From the Fraser Institute
By Jake Fuss, Julio Mejía, Elmira Aliakbari, Karen Graham and Jock Finlayson
Ottawa and the four biggest provinces have spent (or foregone revenues) of at least $158 billion to create at most 68,000 “clean” jobs since 2014
Despite the hype of a “clean” economic transition, governments in Ottawa and in the four largest provinces have spent or foregone revenues of more than $150 billion (inflation-adjusted) on low-carbon initiatives since 2014/15, but have only created, at best, 68,000 clean jobs, according to two new studies published by the Fraser Institute, an independent, non-partisan Canadian public policy think-tank.
“Governments, activists and special interest groups have been making a lot of claims about the opportunities of a clean economic transition, but after a decade of policy interventions and more than $150 billion in taxpayers’ money, the results are
extremely underwhelming,” said Elmira Aliakbari, director of natural resource studies and co-author of The Fiscal Cost of Canada’s Low-Carbon Economy.
The study finds that since 2014/15, the federal government and provincial governments in the country’s four largest provinces (Ontario, Quebec, Alberta and British Columbia) combined have spent and foregone revenues of $158 billion (inflation adjusted to 2024 dollars) trying to create clean jobs, as defined by Statistics Canada’s Environmental and Clean Technology Products Economic Account.
Importantly, that cost estimate is conservative since it does not account for an exhaustive list of direct government spending and it does not measure the costs from Canada’s other six provinces, municipalities, regulatory costs and other economic
costs because of the low-carbon spending and tax credits.
A second study, Sizing Canada’s Clean Economy, finds that there was very little change over the 2014 to 2023 period in terms of the share of the total economy represented by the clean economy. For instance, in 2014, the clean economy represented 3.1 per cent of GDP compared to 3.6 per cent in 2023.
“The evidence is clear—the much-hyped clean economic transition has failed to fundamentally transform Canada’s $3.3 trillion economy,” said study co-author and Fraser Institute senior fellow Jock Finlayson.
State of the Green Economy
- The Fiscal Cost of Canada’s Low-Carbon Economy documents spending initiatives by the federal government and the governments of Ontario, British Columbia, Alberta, and Quebec since 2014 to promote the low-carbon economy, as well as how much revenue they have foregone through offering tax credits.
- Overall, the combined cost of spending and tax credits supporting a low-carbon economy by the federal government and the four provincial governments is estimated at $143.6 billion from 2014–15 to 2024–25, in nominal terms. When adjusted for inflation, the total reaches $158 billion in 2024 dollars.
- These estimates are based on very conservative assumptions, and they do not cover every program area or government-controlled expenditure related to the low-carbon economy and/or reducing greenhouse gas emissions.
- Sizing Canada’s Green Economy assesses the composition, growth, share of Gross Domestic Product (GDP) output, and employment of Canada’s “clean economy” from 2014 to 2023.
- Canada’s various environmental and clean technology industries collectively have accounted for between 3.07% and 3.62% of all-industry GDP over the 10-year period from 2014 to 2023. While it has grown, the sector as a whole has not been expanding at a pace that meaningfully exceeds the growth of the overall Canadian economy, despite significant policy attention and mounting public subsidies.
- The clean economy represents a respectable and relatively stable share of Canada’s $3.3 trillion economy. However, it remains a small part of Canada’s broader industrial mix, it is not a major source of export earnings, and it is not about to supplant the many other industries that underpin the country’s prosperity and dominate its international exports.
Alberta
B.C. would benefit from new pipeline but bad policy stands in the way

From the Fraser Institute
By Julio Mejía and Elmira Aliakbari
Bill C-69 (a.k.a. the “no pipelines act”) has added massive uncertainty to the project approval process, requiring proponents to meet vague criteria that go far beyond any sensible environmental concerns—for example, assessing any project’s impact on the “intersection of sex and gender with other identity factors.”
In case you haven’t heard, the Alberta government plans to submit a proposal to the federal government to build an oil pipeline from Alberta to British Columbia’s north coast.
But B.C. Premier Eby dismissed the idea, calling it a project imported from U.S. politics and pursued “at the expense of British Columbia and Canada’s economy.” He’s simply wrong. A new pipeline wouldn’t come at the expense of B.C. or Canada’s economy—it would strengthen both. In fact, particularly during the age of Trump, provinces should seek greater cooperation and avoid erecting policy barriers that discourage private investment and restrict trade and market access.
The United States remains the main destination for Canada’s leading exports, oil and natural gas. In 2024, nearly 96 per cent of oil exports and virtually all natural gas exports went to our southern neighbour. In light of President Trump’s tariffs on Canadian energy and other goods, it’s long past time to diversify our trade and find new export markets.
Given that most of Canada’s oil and gas is landlocked in the Prairies, pipelines to coastal terminals are the only realistic way to reach overseas markets. After the completion of the Trans Mountain Pipeline Expansion (TMX) project in May 2024, which transports crude oil from Alberta to B.C. and opened access to Asian markets, exports to non-U.S. destinations increased by almost 60 per cent. This new global reach strengthens Canada’s leverage in trade negotiations with Washington, as it enables Canada to sell its energy to markets beyond the U.S.
Yet trade is just one piece of the broader economic impact. In its first year of operation, the TMX expansion generated $13.6 billion in additional revenue for the economy, including $2.0 billion in extra tax revenues for the federal government. By 2043, TMX operations will contribute a projected $9.2 billion to Canada’s economic output, $3.7 billion in wages, and support the equivalent of more than 36,000 fulltime jobs. And B.C. stands to gain the most, with $4.3 billion added to its economic output, nearly $1 billion in wages, and close to 9,000 new jobs. With all due respect to Premier Eby, this is good news for B.C. workers and the provincial economy.
In contrast, cancelling pipelines has come at a real cost to B.C. and Canada’s economy. When the Trudeau government scrapped the already-approved Northern Gateway project, Canada lost an opportunity to increase the volume of oil transported from Alberta to B.C. and diversify its trading partners. Meanwhile, according to the Canadian Energy Centre, B.C. lost out on nearly 8,000 jobs a year (or 224,344 jobs in 29 years) and more than $11 billion in provincial revenues from 2019 to 2048 (inflation-adjusted).
Now, with the TMX set to reach full capacity by 2027/28, and Premier Eby opposing Alberta’s pipeline proposal, Canada may miss its chance to export more to global markets amid rising oil demand. And Canadians recognize this opportunity—a recent poll shows that a majority of Canadians (including 56 per cent of British Columbians) support a new oil pipeline from Alberta to B.C.
But, as others have asked, if the economic case is so strong, why has no private company stepped up to build or finance a new pipeline?
Two words—bad policy.
At the federal level, Bill C-48 effectively bans large oil tankers from loading or unloading at ports along B.C.’s northern coast, undermining the case for any new private-sector pipeline. Meanwhile, Bill C-69 (a.k.a. the “no pipelines act”) has added massive uncertainty to the project approval process, requiring proponents to meet vague criteria that go far beyond any sensible environmental concerns—for example, assessing any project’s impact on the “intersection of sex and gender with other identity factors.” And the federal cap on greenhouse gas (GHG) emissions exclusively for the oil and gas sector will inevitably force a reduction in oil and gas production, again making energy projects including pipelines less attractive to investors.
Clearly, policymakers in Canada should help diversify trade, boost economic growth and promote widespread prosperity in B.C., Alberta and beyond. To achieve this goal, they should put politics aside, focus of the benefits to their constituents, and craft regulations that more thoughtfully balance environmental concerns with the need for investment and economic growth.
-
 International2 days ago
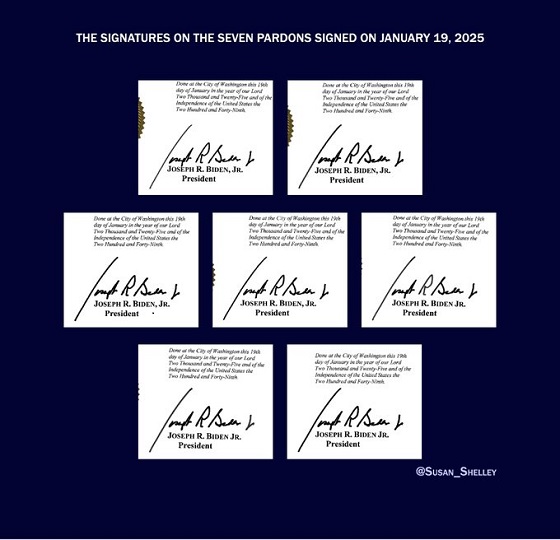
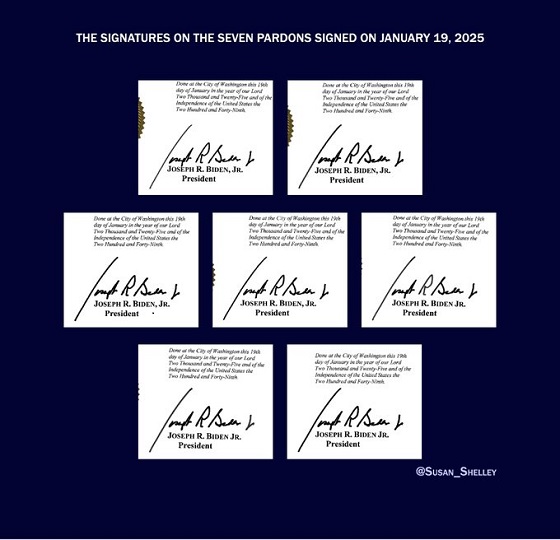
International2 days agoBiden’s Autopen Orders declared “null and void”
-

 Business2 days ago
Business2 days agoTrans Mountain executive says it’s time to fix the system, expand access, and think like a nation builder
-

 Business1 day ago
Business1 day agoCanada has given $109 million to Communist China for ‘sustainable development’ since 2015
-

 National13 hours ago
National13 hours agoCanadian MPs order ethics investigation into Mark Carney’s corporate interests
-

 Business2 days ago
Business2 days agoCanada’s combative trade tactics are backfiring
-

 Canada Free Press2 days ago
Canada Free Press2 days agoThe real genocide is not taking place in Gaza, but in Nigeria
-

 Banks18 hours ago
Banks18 hours agoBank of Canada Cuts Rates to 2.25%, Warns of Structural Economic Damage
-

 Opinion1 day ago
Opinion1 day agoBritish Columbians protest Trump while Eby brings their province to its knees