Health
Dr. Malone: Bird flu ‘emergency’ in California is a case of psychological bioterrorism

From LifeSiteNews
Contrary to initial reporting from corporate media, the WHO, and the apocalyptic mutterings of Dr. Peter Hotez, there continues to be no evidence indicating the circulation of a highly pathogenic version of bird flu in either animal or human populations.
What is the current threat assessment for Avian Influenza, and has it changed?
I previously established and published a brief baseline threat assessment for Avian Influenza on July 2, 2024. Four dominant parameters must be considered when assessing a potential infectious disease threat to human populations:
- Disease severity (a measurable objective truth)
- Mechanism of transmission and observed transmissibility (an experimentally testable objective truth)
- Evidence of sustained human-to-human transmission (a measurable objective truth)
- Assessment of anticipated future risk (subjective, speculative, and hypothetical)
Politicians and their allies (in BioPharma, academia, and other sectors) have a variety of conflicts of interest and agendas which are not aligned with objective, dispassionate assessment and response to public health and infectious disease issues, and cannot be relied upon to analyze and respond to these key parameters objectively.
An assessment of the conflicts of interest and political agenda(s) of California’s Gavin Newsom is beyond the scope of this analysis. Still, please remember that Governor Newsom clearly mismanaged and overreacted to the COVID threat, as did the World Economic Forum that trained and coached (coaches?) him as a “Young Leader” and clearly continues to influence his political postures.
Although California has remained under Democrat party control – in significant part consequent to “rank choice” voting policies – during the recent presidential election there was a clear shift and momentum toward the Republican party across the majority of the state.
California has a very large dairy industry, and I know that a leader in and representative of that industry has close connections to Newsom. The presence of the virus in Southern California dairy farms is widespread, with over 300 dairy herds testing positive in the last 30 days
Has the threat assessment circa July 2024 changed? Let’s revisit the basics:
Disease severity, December 2024
Disease severity continues to be mild, with the exception of one new case which apparently triggered Newsom to declare a state of emergency in California.
According to Newsweek, “A person in Louisiana was hospitalized in critical condition with severe respiratory symptoms from a bird flu infection, according to state health officials. The patient had been in contact with sick and dead birds in a backyard flock, according to the CDC. Louisiana health officials said the patient is older than 65 and has underlying medical conditions.”
Here is the current CDC threat summary
- H5 bird flu is widespread in wild birds worldwide and is causing outbreaks in poultry and U.S. dairy cows with several recent human cases in U.S. dairy and poultry workers.
- While the current public health risk is low, CDC is watching the situation carefully and working with states to monitor people with animal exposures.
- CDC is using its flu surveillance systems to monitor for H5 bird flu activity in people.



The CDC charts above document that the risk of H5 in humans is low, disease severity is low, and although massive testing has occurred, there are only 61 total “exposure” sources found from cattle, birds, and other mammals.
There are a total of three human cases picked up from the CDC flu surveillance program since February 25, 2024, and a total of 58 cases in the U.S., after testing almost 10,000 people who were exposed to infected animals.
In sum, the profile of disease severity has not changed since July 2024. As opposed to initial reporting from corporate media, dark warnings from the WHO and Dr. Tedros, and the apocalyptic mutterings of Dr. Peter Hotez, there continues to be no evidence indicating the circulation of a highly pathogenic version of this virus in either animal or human populations.
Mechanism of transmission and observed transmissibility
All reported U.S. transmission events involve human exposure in the context of intensive contact during animal husbandry or other known animal hosts, indicating that the mechanism of transmission remains intensive exposure to infected animals and animal carcasses. No change from July 2024.
Evidence of sustained human-to-human transmission
No evidence of sustained human-to-human transmission, now or in the past with this currently circulating variant.
Assessment of anticipated future risk
This appears to be the crux of Newsom’s alarmist response involving the declaration of a “State of Emergency” for bird flu in California. A statement from the governor’s office characterized the move as a “proactive action to strengthen robust state response” to avian influenza A (H5N1), also known as bird flu.
“This proclamation is a targeted action to ensure government agencies have the resources and flexibility they need to respond quickly to this outbreak,” Newsom said in a statement. “Building on California’s testing and monitoring system – the largest in the nation – we are committed to further protecting public health, supporting our agriculture industry, and ensuring that Californians have access to accurate, up-to-date information.”
He added, “While the risk to the public remains low, we will continue to take all necessary steps to prevent the spread of this virus.”
This statement demonstrates either a profound ignorance of the mechanism by which animal influenza viruses spread, including avian influenza, or the presence of a hidden agenda. With a wide range of animal reservoirs, including migratory waterfowl, there is no way that the state of California can prevent the spread of this virus.
READ: Australian doctor who criticized COVID jabs has his suspension reversed
Conclusion
There has been no significant change in the current threat assessment associated with Avian Influenza relative to July 2024. The CDC, which has recently been implicated in industrial-scale “PsyWar” deployment of psychological bioterrorism regarding COVID and has an organizational conflict of interest in promoting vaccines and vaccine uptake, characterizes the current public health risk as low.
My conclusion regarding the Newsom declaration of a “State of Emergency” for bird flu in California is that it is being driven by a hidden agenda. There are multiple hypotheses regarding what that hidden agenda may be, but Newsom’s statement that, “Building on California’s testing and monitoring system – the largest in the nation – we are committed to further protecting public health, supporting our agriculture industry, and ensuring that Californians have access to accurate, up-to-date information,” suggests that this declaration may, at a minimum, reflect advocacy by and for California’s infectious disease testing industry, which includes both academic and commercial components.
Reprinted with permission from Robert Malone.
Alberta
A Christmas wish list for health-care reform

From the Fraser Institute
By Nadeem Esmail and Mackenzie Moir
It’s an exciting time in Canadian health-care policy. But even the slew of new reforms in Alberta only go part of the way to using all the policy tools employed by high performing universal health-care systems.
For 2026, for the sake of Canadian patients, let’s hope Alberta stays the path on changes to how hospitals are paid and allowing some private purchases of health care, and that other provinces start to catch up.
While Alberta’s new reforms were welcome news this year, it’s clear Canada’s health-care system continued to struggle. Canadians were reminded by our annual comparison of health care systems that they pay for one of the developed world’s most expensive universal health-care systems, yet have some of the fewest physicians and hospital beds, while waiting in some of the longest queues.
And speaking of queues, wait times across Canada for non-emergency care reached the second-highest level ever measured at 28.6 weeks from general practitioner referral to actual treatment. That’s more than triple the wait of the early 1990s despite decades of government promises and spending commitments. Other work found that at least 23,746 patients died while waiting for care, and nearly 1.3 million Canadians left our overcrowded emergency rooms without being treated.
At least one province has shown a genuine willingness to do something about these problems.
The Smith government in Alberta announced early in the year that it would move towards paying hospitals per-patient treated as opposed to a fixed annual budget, a policy approach that Quebec has been working on for years. Albertans will also soon be able purchase, at least in a limited way, some diagnostic and surgical services for themselves, which is again already possible in Quebec. Alberta has also gone a step further by allowing physicians to work in both public and private settings.
While controversial in Canada, these approaches simply mirror what is being done in all of the developed world’s top-performing universal health-care systems. Australia, the Netherlands, Germany and Switzerland all pay their hospitals per patient treated, and allow patients the opportunity to purchase care privately if they wish. They all also have better and faster universally accessible health care than Canada’s provinces provide, while spending a little more (Switzerland) or less (Australia, Germany, the Netherlands) than we do.
While these reforms are clearly a step in the right direction, there’s more to be done.
Even if we include Alberta’s reforms, these countries still do some very important things differently.
Critically, all of these countries expect patients to pay a small amount for their universally accessible services. The reasoning is straightforward: we all spend our own money more carefully than we spend someone else’s, and patients will make more informed decisions about when and where it’s best to access the health-care system when they have to pay a little out of pocket.
The evidence around this policy is clear—with appropriate safeguards to protect the very ill and exemptions for lower-income and other vulnerable populations, the demand for outpatient healthcare services falls, reducing delays and freeing up resources for others.
Charging patients even small amounts for care would of course violate the Canada Health Act, but it would also emulate the approach of 100 per cent of the developed world’s top-performing health-care systems. In this case, violating outdated federal policy means better universal health care for Canadians.
These top-performing countries also see the private sector and innovative entrepreneurs as partners in delivering universal health care. A relationship that is far different from the limited individual contracts some provinces have with private clinics and surgical centres to provide care in Canada. In these other countries, even full-service hospitals are operated by private providers. Importantly, partnering with innovative private providers, even hospitals, to deliver universal health care does not violate the Canada Health Act.
So, while Alberta has made strides this past year moving towards the well-established higher performance policy approach followed elsewhere, the Smith government remains at least a couple steps short of truly adopting a more Australian or European approach for health care. And other provinces have yet to even get to where Alberta will soon be.
Let’s hope in 2026 that Alberta keeps moving towards a truly world class universal health-care experience for patients, and that the other provinces catch up.
Health
FDA warns ‘breast binder’ manufacturers to stop marketing to gender-confused girls

From LifeSiteNews
Dr. Marty Makary took aim at the transgender-medical-industrial complex that has exploded in recent years during a recent press conference.
Food and Drug Administration (FDA) commissioner Dr. Marty Makary has sternly warned companies manufacturing “breast binders” to cease marketing and supplying their product to gender-confused girls seeking to make their bodies appear masculine.
“Today the FDA is taking action,” said Makary in a press conference. “We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.”
“Breast binders are a class one medical device with legitimate medical users, such as being used by women after breast cancer surgery,” but “these binders are not benign,” he cautioned. “Long-term usage has been associated with pain, compromised lung function, and even difficulty breast feeding later in life.”
“The warning letters will formally notify the companies of their significant regulatory violations and require prompt corrective action,” said the FDA head.
.@DrMakaryFDA: “Today the FDA is taking action. We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.” pic.twitter.com/6JNAy36223
— HHS Rapid Response (@HHSResponse) December 18, 2025
The warning letter addressed to California manufacturer, GenderBender, notes that the company’s website states that “[c]hest binding is the practice of compressing breast mass into a more masculine shape, often done in the LGBTQ community for gender euphoria.”
“Your firm should take prompt action to address any violations identified in this letter. Failure to adequately address this matter may result in regulatory action being initiated by the FDA without further notice. These actions include, but are not limited to, seizure and injunction,” advised the FDA.
During his presentation, Makary took aim at the transgender-medical-industrial complex that has exploded in recent years.
“One of the most barbaric features of a society is the genital mutilation of its children,” observed Makary.
“Pushing transgender ideology in children is predatory, it’s wrong, and it needs to stop,” he declared.
“This ideology is a belief system that some teachers, some pediatricians, and others are selling to children without their parents knowing sometimes, or with a deliberate attempt to remove parents from the decision making,” Makary explained.
To witness society “putting kids on a path of chest binders, drugs, castration, mastectomies, and other procedures is a path that now many kids regret,” he lamented, as he pointed to Chloe Cole, who has reverted to her God-given femininity after undergoing so-called “gender-affirming” surgery as a teen.
Cole is a leading voice for young people who have “detransitioned” after having medically, surgically, and socially attempted to “transition” to a member of the opposite sex.
.@DrMakaryFDA: “Pushing transgender ideology in children is predatory, it's wrong, and it needs to stop.” pic.twitter.com/TXxWNEtNZk
— HHS Rapid Response (@HHSResponse) December 18, 2025
-

 Energy24 hours ago
Energy24 hours agoWhy Japan wants Western Canadian LNG
-
 Business20 hours ago
Business20 hours agoMainstream media missing in action as YouTuber blows lid off massive taxpayer fraud
-

 Business1 day ago
Business1 day agoWhat Do Loyalty Rewards Programs Cost Us?
-

 Business23 hours ago
Business23 hours agoLand use will be British Columbia’s biggest issue in 2026
-
 International11 hours ago
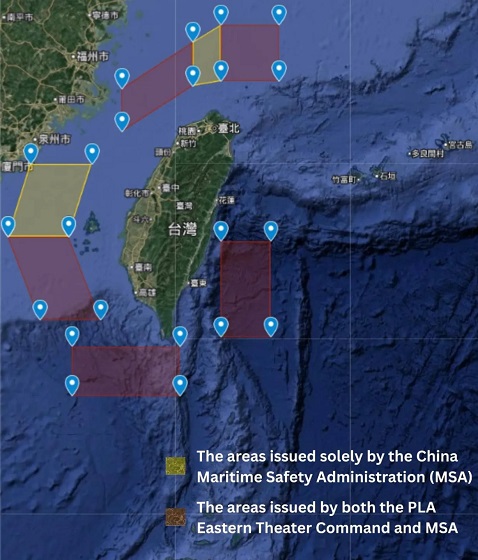
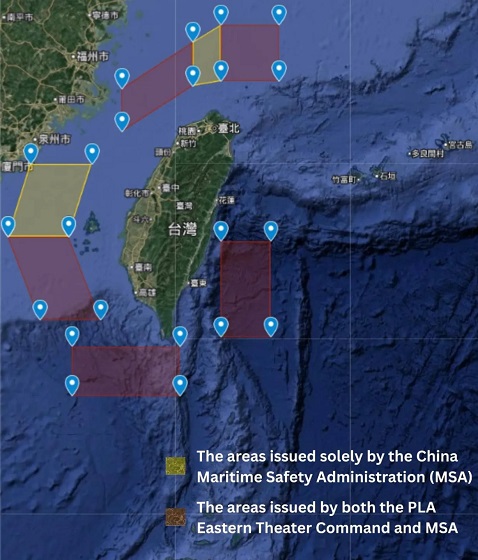
International11 hours agoChina Stages Massive Live-Fire Encirclement Drill Around Taiwan as Washington and Japan Fortify
-

 Haultain Research1 day ago
Haultain Research1 day agoSweden Fixed What Canada Won’t Even Name
-

 Energy12 hours ago
Energy12 hours agoRulings could affect energy prices everywhere: Climate activists v. the energy industry in 2026
-

 Business20 hours ago
Business20 hours agoStripped and shipped: Patel pushes denaturalization, deportation in Minnesota fraud




