Health
Canadians face longest waits for health care on record

From the Fraser Institute
By Bacchus Barua and Mackenzie Moir
Just when you thought Canadian health care had hit rock bottom, wait times in 2024 have hit an all-time high.
According to the latest version of our annual report published by the Fraser Institute, the median wait from referral by a family doctor to treatment (averaged across 10 provinces and 12 medical specialties including surgeries) is now 30 weeks—the longest wait in the report’s history and more than three times longer than the 9.3-week median wait in 1993.
Of course, wait times vary by province, and some provinces are worse than others. In New Brunswick and Prince Edward Island, the median wait is more than one year. And even in Ontario, which reported the shortest wait times in Canada this year, patients faced a 23.6-week wait, the longest in the province’s history.
In fact, compared to last year, wait times grew in every province (except Nova Scotia where patients still faced a median wait just shy of 40 weeks this year).
There’s also considerable variation in wait times depending on the type of care. For example, patients faced the longest waits for orthopedic surgeries (57.5 weeks) and neurosurgery (46.2 weeks) and shorter waits for chemotherapy (4.7 weeks), and radiological cancer treatments (4.5 weeks). In total, the study estimated that Canadian patients were waiting for more than 1.5 million procedures in 2024.
These waits for care are not benign inconveniences. Patients may experience physical pain, psychological distress and worsening physical condition while awaiting care. This year, the 15-week median wait for treatment after seeing a specialist was more than a month and a half longer than what physicians consider a reasonable wait (8.6 weeks). And this doesn’t even include the median 15-week wait to see a specialist in the first place.
Moreover, according to the Commonwealth Fund, a U.S.-based health-care research organization, among nine universal health-care systems worldwide, last year patients in Canada were the second-most likely to report waiting longer than one month for a specialist consultation, and the most likely to report waiting more than two months for surgery. In other words, although long wait times remain a staple of Canadian health care, they are not a necessary trade-off for having universal coverage.
And to be clear, wait times are only one manifestation of the strain on Canada’s health-care system. It’s now also normal to see emergency room closures, health-care worker burnout, and data suggesting millions of Canadians are without access to a regular health-care provider.
What’s the solution to Canada’s crippling health-care wait times?
There are many options for reform. But put simply, if policymakers in Canada want to reduce wait times for patients across the country, they should learn from better-performing universal health-care countries where patients receive more timely care. With wait times this year reaching an all-time high, relief can’t come soon enough.
Addictions
There’s No Such Thing as a “Safer Supply” of Drugs

By Adam Zivo
Sweden, the U.K., and Canada all experimented with providing opioids to addicts. The results were disastrous.
[This article was originally published in City Journal, a public policy magazine and website published by the Manhattan Institute for Policy Research. We encourage our readers to subscribe to them for high-quality analysis on urban issues]
Last August, Denver’s city council passed a proclamation endorsing radical “harm reduction” strategies to address the drug crisis. Among these was “safer supply,” the idea that the government should give drug users their drug of choice, for free. Safer supply is a popular idea among drug-reform activists. But other countries have already tested this experiment and seen disastrous results, including more addiction, crime, and overdose deaths. It would be foolish to follow their example.
The safer-supply movement maintains that drug-related overdoses, infections, and deaths are driven by the unpredictability of the black market, where drugs are inconsistently dosed and often adulterated with other toxic substances. With ultra-potent opioids like fentanyl, even minor dosing errors can prove fatal. Drug contaminants, which dealers use to provide a stronger high at a lower cost, can be just as deadly and potentially disfiguring.
Because of this, harm-reduction activists sometimes argue that governments should provide a free supply of unadulterated, “safe” drugs to get users to abandon the dangerous street supply. Or they say that such drugs should be sold in a controlled manner, like alcohol or cannabis—an endorsement of partial or total drug legalization.
But “safe” is a relative term: the drugs championed by these activists include pharmaceutical-grade fentanyl, hydromorphone (an opioid as potent as heroin), and prescription meth. Though less risky than their illicit alternatives, these drugs are still profoundly dangerous.
The theory behind safer supply is not entirely unreasonable, but in every country that has tried it, implementation has led to increased suffering and addiction. In Europe, only Sweden and the U.K. have tested safer supply, both in the 1960s. The Swedish model gave more than 100 addicts nearly unlimited access through their doctors to prescriptions for morphine and amphetamines, with no expectations of supervised consumption. Recipients mostly sold their free drugs on the black market, often through a network of “satellite patients” (addicts who purchased prescribed drugs). This led to an explosion of addiction and public disorder.
Most doctors quickly abandoned the experiment, and it was shut down after just two years and several high-profile overdose deaths, including that of a 17-year-old girl. Media coverage portrayed safer supply as a generational medical scandal and noted that the British, after experiencing similar problems, also abandoned their experiment.
While the U.S. has never formally adopted a safer-supply policy, it experienced something functionally similar during the OxyContin crisis of the 2000s. At the time, access to the powerful opioid was virtually unrestricted in many parts of North America. Addicts turned to pharmacies for an easy fix and often sold or traded their extra pills for a quick buck. Unscrupulous “pill mills” handed out prescriptions like candy, flooding communities with OxyContin and similar narcotics. The result was a devastating opioid epidemic—one that rages to this day, at a cumulative cost of hundreds of thousands of American lives. Canada was similarly affected.
The OxyContin crisis explains why many experienced addiction experts were aghast when Canada greatly expanded access to safer supply in 2020, following a four-year pilot project. They worried that the mistakes of the recent past were being made all over again, and that the recently vanquished pill mills had returned under the cloak of “harm reduction.”
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Most Canadian safer-supply prescribers dispense large quantities of hydromorphone with little to no supervised consumption. Patients can receive up to 40 eight-milligram pills per day—despite the fact that just two or three are enough to cause an overdose in someone without opioid tolerance. Some prescribers also provide supplementary fentanyl, oxycodone, or stimulants.
Unfortunately, many safer-supply patients sell or trade a significant portion of these drugs—primarily hydromorphone—in order to purchase more potent illicit substances, such as street fentanyl.
The problems with safer supply entered Canada’s consciousness in mid-2023, through an investigative report I wrote for the National Post. I interviewed 14 addiction physicians from across the country, who testified that safer-supply diversion is ubiquitous; that the street price of hydromorphone collapsed by up to 95 percent in communities where safer supply is available; that youth are consuming and becoming addicted to diverted safer-supply drugs; and that organized crime traffics these drugs.
Facing pushback, I interviewed former drug users, who estimated that roughly 80 percent of the safer-supply drugs flowing through their social circles was getting diverted. I documented dozens of examples of safer-supply trafficking online, representing tens of thousands of pills. I spoke with youth who had developed addictions from diverted safer supply and adults who had purchased thousands of such pills.
After months of public queries, the police department of London, Ontario—where safer supply was first piloted—revealed last summer that annual hydromorphone seizures rose over 3,000 percent between 2019 and 2023. The department later held a press conference warning that gangs clearly traffic safer supply. The police departments of two nearby midsize cities also saw their post-2019 hydromorphone seizures increase more than 1,000 percent.
The Canadian government quietly dropped its support for safer supply last year, cutting funding for many of its pilot programs. The province of British Columbia (the nexus of the harm-reduction movement) finally pulled back support last month, after a leaked presentation confirmed that safer-supply drugs are getting sold internationally and that the government is investigating 60 pharmacies for paying kickbacks to safer-supply patients. For now, all safer-supply drugs dispensed within the province must be consumed under supervision.
Harm-reduction activists have insisted that no hard evidence exists of widespread diversion of safer-supply drugs, but this is only because they refuse to study the issue. Most “studies” supporting safer supply are produced by ideologically driven activist-scholars, who tend to interview a small number of program enrollees. These activists also reject attempts to track diversion as “stigmatizing.”
The experiences of Sweden, the United Kingdom, and Canada offer a clear warning: safer supply is a reliably harmful policy. The outcomes speak for themselves—rising addiction, diversion, and little evidence of long-term benefit.
As the debate unfolds in the United States, policymakers would do well to learn from these failures. Americans should not be made to endure the consequences of a policy already discredited abroad simply because progressive leaders choose to ignore the record. The question now is whether we will repeat others’ mistakes—or chart a more responsible course.
Our content is always free –
but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
Health
RFK Jr. says ‘everything is going to change’ with CDC vaccine policy in Michael Knowles interview
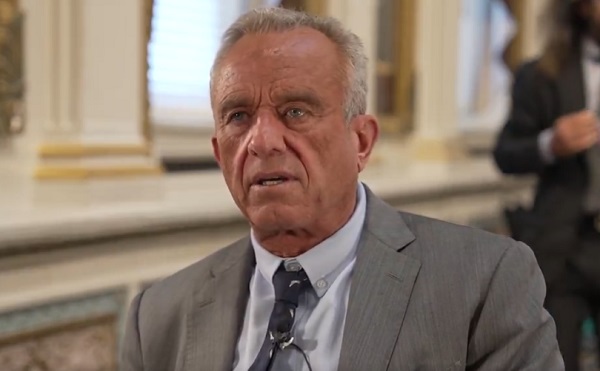
From LifeSiteNews
New Health and Human Services Director Robert F. Kennedy Jr. said the CDC’s own reporting system ‘captures fewer than 1% of vaccine injuries. It’s worthless, and everybody agrees it’s worthless.’
When Michael Knowles asked new Health and Human Services (HHS) Secretary Robert F. Kennedy Jr. if anything will change regarding the public’s justifiable concern with the growth of vaccines, Kennedy quickly shot back, “Everything is going to change.”
Kennedy pointed to the Centers for Disease Control’s current flawed VAERS (Vaccine Adverse Event Reporting System) online mechanism.
By way of example, he said, “None of the vaccines that are given during the first six months of life have ever been tested for autism. The only one was the DTP vaccine. And that one study that was done, according to the Institute of Medicine, the National Academy of Sciences, found that there was a link.”
But “They threw out that study because it was based upon CDC’s surveillance system, VAERS, and they said that system is no good.”
“That begs the question, why doesn’t CDC have a functional surveillance system?” he asked. “We’re gonna make sure they do.”
“They don’t do pre-licensing safety testing for vaccines” he continued. “They’re the only product that’s exempt. So what they say is, if there are injuries, we’ll capture them afterward.”
However, “they have a system that doesn’t capture them. In fact, CDC’s own study of its own system said it captures fewer than 1% of vaccine injuries,” Kennedy said. “It’s worthless, and everybody agrees it’s worthless.”
“Why have we gone for 39 years and nobody’s fixed it?” he wondered, promising, “We’re gonna fix it.”
“We have DOGE (which) knows how to manage data. We’re going to be able to get into these databases and give answers to the American public,” Kennedy predicted.
“We’re going to have gold standard science, we’re going to follow the science, we’re going to publish all of our datasets, which CDC has never done,” he said.
“We’re going to do replication of all of our studies, which CDC has never done. We’re going to publish our peer review, which CDC has never done,” Kennedy vowed. “So people are going to have real answers for the first time.”
The new HHS head also discussed more broadly his mission after taking over the department’s helm, the mess created by the Biden administration, his job’s challenges, and recent developments thanks to DOGE.
“HHS is a $1.9 trillion agency. It’s the biggest agency in the government. And during the Biden administration, President Biden increased its budget by 38% and increased the workforce by 17%.”
“And by every metric by which we measure public health, health accelerated its decline.”
“When I came to HHS, what I found was a sprawling bureaucracy,” with functional duplication of departments, rampant redundancy and overstaffing, with various sub-agencies often acting in a territorial, self-protecting manner rather than a synergistic one.
“Perverse incentives” sometimes drive employee’s work,” he noted.
Despite his short tenure at HHS, with the help of DOGE, Kennedy has already released 20,000 “bureaucrats” from the department’s ranks.
“We’re going from 82,000 personnel to 62,000,” said Kennedy, carefully pointing out, “We’re keeping the scientists and frontline providers.”
Kennedy said that it has been really hard to fight against the problems at HHS and NIH over the last 40 years from “the outside.”
But “now I’m on the inside,” he declared. “This is the purpose of my life. It’s what I’m going to do over the next four years.”
He concluded:
President Trump promised to return the American dream to Americans.
A healthy person has a thousand dreams. A sick person only has one.
-
 Uncategorized1 day ago
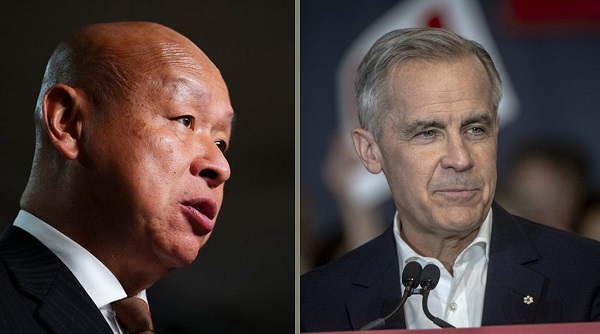
Uncategorized1 day agoPoilievre on 2025 Election Interference – Carney sill hasn’t fired Liberal MP in Chinese election interference scandal
-

 Business2 days ago
Business2 days agoCuba has lost 24% of it’s population to emigration in the last 4 years
-
 2025 Federal Election1 day ago
2025 Federal Election1 day ago2025 Election Interference – CCP Bounty on Conservative Candidate – Carney Says Nothing
-

 2025 Federal Election1 day ago
2025 Federal Election1 day ago2025 Federal Election Interference from China! Carney Pressed to Remove Liberal MP Over CCP Bounty Remark
-
 2025 Federal Election14 hours ago
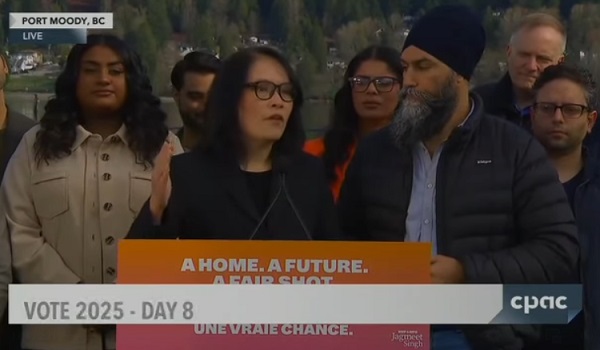
2025 Federal Election14 hours agoChinese Election Interference – NDP reaction to bounty on Conservative candidate
-
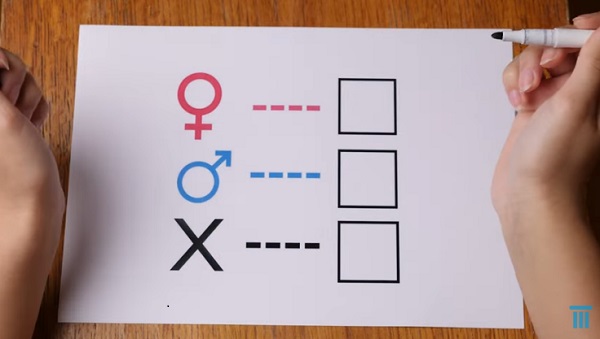 Aristotle Foundation2 days ago
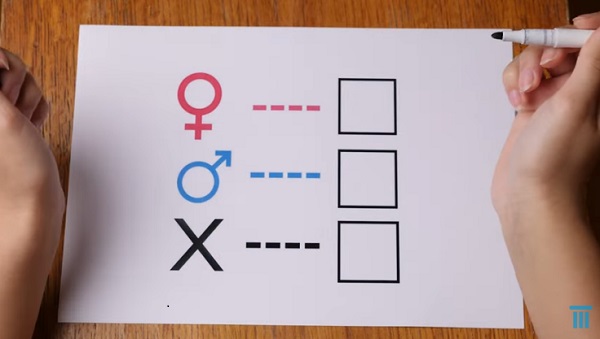
Aristotle Foundation2 days agoCanada has the world’s MOST relaxed gender policy for minors
-

 International2 days ago
International2 days agoTrump signs executive order to make Washington D.C. “safe and beautiful”
-
 Media1 day ago
Media1 day agoTop Five Huge Stories the Media Buried This Week








