Addictions
B.C. parents powerless to help their addicted teens

B.C. parents say the province’s safer supply program and legal treatment framework leave them powerless to help their addicted teens
On Aug. 19, 2022, Kamilah Sword took a single hydromorphone pill, believing it to be safe. She overdosed and was found dead by her grandmother the next day. She was 14.
Kamilah believed the drug was safe — despite having bought it illicitly — because she was told it came from a government-run “safer supply” program, according to Kamillah’s best friend Grace Miller and her father.
“I’ll never get to see her get married, never have grandkids, never get to see her graduate,” said Kamilah’s father, Gregory Sword, lowering his chin to keep his voice steady.
“It’s a black hole in the heart that never heals.”
Sword faced significant challenges trying to get his daughter help during the year he was aware she was struggling with addiction. He blames British Columbia’s safer supply program and the province’s legal youth treatment framework for exacerbating his daughter’s challenges and ultimately contributing to her death.
“It’s a B.C. law — you cannot force a minor into rehab without their permission,” said Sword. “You cannot parent your kid between the ages of 12 and 18 without their consent.”
Sword is now pursuing legal action against the B.C. and federal governments and several health agencies, seeking accountability for what he views as systemic failures.
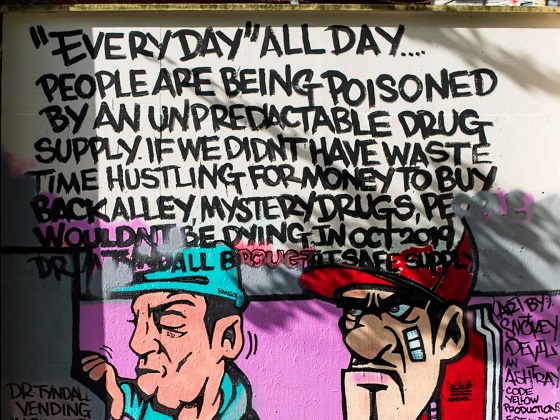
B.C.’s “Safe” supply program
B.C.’s prescribed safer supply program, which was first launched in 2020, is designed to reduce substance users’ reliance on dangerous street drugs. Users are prescribed hydromorphone — an opioid as potent as heroin — as an alternative to using potentially lethal street drugs.
However, participants in the program often sell their hydromorphone, in some cases to teenagers, to get money to buy stronger drugs like fentanyl.
According to Grace Miller, she and Kamilah would obtain hydromorphone — which is commonly referred to as Dilaudid or “dillies” — from a teenage friend who bought them in Vancouver’s Downtown Eastside. The neighbourhood, which is the epicentre of Vancouver’s drug crisis, is a 30-minute SkyTrain ride from the teenagers’ home in Port Coquitlam.
Sword says he initially thought “dillies” referred to Dairy Queen’s Dilly Bars. “My daughter would ask me for $5, [and say], ‘Yeah, we’re going to Dairy Queen for a Dilly Bar.’ I had no idea.”
He says he only learned about hydromorphone after the coroner informed him that Kamilah had three substances in her system: cocaine, MDMA and hydromorphone.
“I had to start talking to people to figure out what [hydromorphone] was and where it was coming from.”
Sword is critical of B.C.’s safer supply program for being presented as safe and for lacking monitoring safeguards. “[Kamilah] knew where [the drugs] were coming from so she felt safe because her dealer would keep on telling her, ‘This is safe supply,’” Sword said.
In February, B.C. changed how it refers to the program from “prescribed safer supply” to “prescribed alternatives.”
Grace says another problem with the program is the quantities of drugs being distributed.
“It would be a big difference if the prescriptions that they were giving out were dosed properly,” she said, noting addicts would typically sell bottles containing 14 pills, with pricing starting at $1 a pill.
‘Safer supply’
Sword estimates his daughter struggled with addiction for about 18 to 24 months before her final, fatal overdose.
After Kamilah overdosed for the first time on Aug. 21, 2021, he tried to get her into treatment. A drug counsellor told him that, because she was over 12, she would need to verbally consent. Kamilah refused treatment.
B.C.’s Infants Act allows individuals aged 12 or older to consent to their own medical treatment if they understand the treatment and its implications. The province’s Mental Health Act requires minors aged 12 to 16 to consent to addiction or mental health treatment.
While parents can request involuntary admission for children under 16, a physician or nurse practitioner must first confirm the presence of a mental disorder that requires treatment. No law specifically addresses substance-use disorders in minors.
When Kamilah was admitted to the hospital on one occasion, she underwent a standard psychiatric evaluation and was quickly discharged — despite Sword’s protests.
Ontario also has a mental health law governing involuntary care. Similar to B.C., they permit involuntary care only where a minor has been diagnosed with a mental disorder.
By contrast, Alberta’s Protection of Children Abusing Drugs Act enables a parent or guardian to obtain a court order to place a child under 18 who is struggling with addiction into a secure facility for up to 15 days for detoxification, stabilization and assessment. Alberta is unique among the provinces and territories in permitting involuntary care of minors for substance-use issues.
Grace, who also became addicted to opioids, says her recovery journey involved several failed attempts.
“I never thought I would have almost died so many times,” said Grace, who is now 16. “I never thought I would even touch drugs in my life.”
Grace’s mother Amanda (a pseudonym) faced similar struggles as Sword in trying to get help for her daughter. Amanda says she was repeatedly told nothing more could be done for Grace, because Grace would not consent to treatment.
“One time, [Grace] overdosed at home, and I had to Narcan her because she was dead in her bed,” Amanda said. “I told the paramedic, ‘Our system is broken.’ And she just said, ‘Yes, I know.’”
Yet Grace, who today has been sober for 10 months, would question whether she even had the capacity to consent to treatment when she was addicted to drugs.
Under B.C.’s Health Care (Consent) and Care Facility (Admission) Act, an adult is only considered to have consented to health care if their consent is voluntary, informed, legitimately obtained and the individual is capable of making a decision about their care.
“Mentally able to give consent?” said Grace. “No, I was never really mentally there.”
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
System failure
Today, Sword is one of two plaintiffs leading a class-action lawsuit against several provincial and federal health authorities and organizations, including the B.C. Ministry of Health, Health Canada, Vancouver Coastal Health and Vancouver Island Health.
All four of these agencies declined to comment for this story, citing the ongoing court proceedings.
The lawsuit was filed Aug. 15 and is currently awaiting certification to proceed. It alleges the coroner initially identified safer supply drugs as a cause of Kamilah’s death, but later changed the report to omit this reference due to pressure from the province or for other unknown reasons.
It further alleges B.C. and Ottawa were aware that drugs prescribed under safer supply programs were being diverted as early as March 2021, but failed to monitor or control the drugs’ distribution. It points to a Health Canada report and data showing increased opioid-related problems from safer supply programs.
According to Amanda, Kamilah had wanted to overcome her addiction but B.C.’s system failed her.
“I had multiple conversations with Kamilah, and I know Kamilah wanted to get clean,” she says. “But she felt so stuck, like she couldn’t do it, and she felt guilty and ashamed.”
Grace, who battled addiction for four years, is relieved to be sober.
“I’ve never, ever been happier. I’ve never been healthier. It’s the best thing I’ve done for myself,” she said. “It’s just hard when you don’t have your best friend to do it with.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Break The Needle. Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
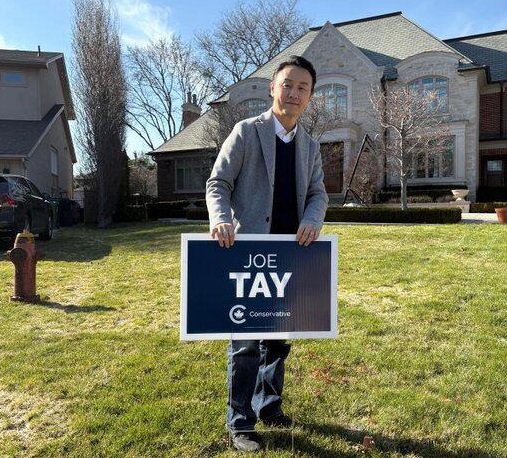
2025 Federal Election
Study links B.C.’s drug policies to more overdoses, but researchers urge caution
By Alexandra Keeler
A study links B.C.’s safer supply and decriminalization to more opioid hospitalizations, but experts note its limitations
A new study says B.C.’s safer supply and decriminalization policies may have failed to reduce overdoses. Furthermore, the very policies designed to help drug users may have actually increased hospitalizations.
“Neither the safer opioid supply policy nor the decriminalization of drug possession appeared to mitigate the opioid crisis, and both were associated with an increase in opioid overdose hospitalizations,” the study says.
The study has sparked debate, with some pointing to it as proof that B.C.’s drug policies failed. Others have questioned the study’s methodology and conclusions.
“The question we want to know the answer to [but cannot] is how many opioid hospitalizations would have occurred had the policy not have been implemented,” said Michael Wallace, a biostatistician and associate professor at the University of Waterloo.
“We can never come up with truly definitive conclusions in cases such as this, no matter what data we have, short of being able to magically duplicate B.C.”
Jumping to conclusions
B.C.’s controversial safer supply policies provide drug users with prescription opioids as an alternative to toxic street drugs. Its decriminalization policy permitted drug users to possess otherwise illegal substances for personal use.
The peer-reviewed study was led by health economist Hai Nguyen and conducted by researchers from Memorial University in Newfoundland, the University of Manitoba and Weill Cornell Medicine, a medical school in New York City. It was published in the medical journal JAMA Health Forum on March 21.
The researchers used a statistical method to create a “synthetic” comparison group, since there is no ideal control group. The researchers then compared B.C. to other provinces to assess the impact of certain drug policies.
Examining data from 2016 to 2023, the study links B.C.’s safer supply policies to a 33 per cent rise in opioid hospitalizations.
The study says the province’s decriminalization policies further drove up hospitalizations by 58 per cent.
“Neither the safer supply policy nor the subsequent decriminalization of drug possession appeared to alleviate the opioid crisis,” the study concludes. “Instead, both were associated with an increase in opioid overdose hospitalizations.”
The B.C. government rolled back decriminalization in April 2024 in response to widespread concerns over public drug use. This February, the province also officially acknowledged that diversion of safer supply drugs does occur.
The study did not conclusively determine whether the increase in hospital visits was due to diverted safer supply opioids, the toxic illicit supply, or other factors.
“There was insufficient evidence to conclusively attribute an increase in opioid overdose deaths to these policy changes,” the study says.
Nguyen’s team had published an earlier, 2024 study in JAMA Internal Medicine that also linked safer supply to increased hospitalizations. However, it failed to control for key confounders such as employment rates and naloxone access. Their 2025 study better accounts for these variables using the synthetic comparison group method.
The study’s authors did not respond to Canadian Affairs’ requests for comment.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Correlation vs. causation
Chris Perlman, a health data and addiction expert at the University of Waterloo, says more studies are needed.
He believes the findings are weak, as they show correlation but not causation.
“The study provides a small signal that the rates of hospitalization have changed, but I wouldn’t conclude that it can be solely attributed to the safer supply and decrim[inalization] policy decisions,” said Perlman.
He also noted the rise in hospitalizations doesn’t necessarily mean more overdoses. Rather, more people may be reaching hospitals in time for treatment.
“Given that the [overdose] rate may have gone down, I wonder if we’re simply seeing an effect where more persons survive an overdose and actually receive treatment in hospital where they would have died in the pre-policy time period,” he said.
The Nguyen study acknowledges this possibility.
“The observed increase in opioid hospitalizations, without a corresponding increase in opioid deaths, may reflect greater willingness to seek medical assistance because decriminalization could reduce the stigma associated with drug use,” it says.
“However, it is also possible that reduced stigma and removal of criminal penalties facilitated the diversion of safer opioids, contributing to increased hospitalizations.”
Karen Urbanoski, an associate professor in the Public Health and Social Policy department at the University of Victoria, is more critical.
“The [study’s] findings do not warrant the conclusion that these policies are causally associated with increased hospitalization or overdose,” said Urbanoski, who also holds the Canada Research Chair in Substance Use, Addictions and Health Services.
Her team published a study in November 2023 that measured safer supply’s impact on mortality and acute care visits. It found safer supply opioids did reduce overdose deaths.
Critics, however, raised concerns that her study misrepresented its underlying data and showed no statistically significant reduction in deaths after accounting for confounding factors.
The Nguyen study differs from Urbanoski’s. While Urbanoski’s team focused on individual-level outcomes, the Nguyen study analyzed broader, population-level effects, including diversion.
Wallace, the biostatistician, agrees more individual-level data could strengthen analysis, but does not believe it undermines the study’s conclusions. Wallace thinks the researchers did their best with the available data they had.
“We do not have a ‘copy’ of B.C. where the policies weren’t implemented to compare with,” said Wallace.
B.C.’s overdose rate of 775 per 100,000 is well above the national average of 533.
Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, has been a vocal critic of B.C.’s decriminalization and safer supply policies.
“If the government doesn’t want to believe this study, well then I invite them to do a similar study,” she told reporters on March 27.
“Show us the evidence that they have failed to show us since 2020,” she added, referring to the year B.C. implemented safer supply.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Our content is always free – but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
Addictions
Addiction experts demand witnessed dosing guidelines after pharmacy scam exposed

By Alexandra Keeler
The move follows explosive revelations that more than 60 B.C. pharmacies were allegedly participating in a scheme to overbill the government under its safer supply program. The scheme involved pharmacies incentivizing clients to fill prescriptions they did not require by offering them cash or rewards. Some of those clients then sold the drugs on the black market.
An addiction medicine advocacy group is urging B.C. to promptly issue new guidelines for witnessed dosing of drugs dispensed under the province’s controversial safer supply program.
In a March 24 letter to B.C.’s health minister, Addiction Medicine Canada criticized the BC Centre on Substance Use for dragging its feet on delivering the guidelines and downplaying the harms of prescription opioids.
The centre, a government-funded research hub, was tasked by the B.C. government with developing the guidelines after B.C. pledged in February to return to witnessed dosing. The government’s promise followed revelations that many B.C. pharmacies were exploiting rules permitting patients to take safer supply opioids home with them, leading to abuse of the program.
“I think this is just a delay,” said Dr. Jenny Melamed, a Surrey-based family physician and addiction specialist who signed the Addiction Medicine Canada letter. But she urged the centre to act promptly to release new guidelines.
“We’re doing harm and we cannot just leave people where they are.”
Addiction Medicine Canada’s letter also includes recommendations for moving clients off addictive opioids altogether.
“We should go back to evidence-based medicine, where we have medications that work for people in addiction,” said Melamed.
‘Best for patients’
On Feb. 19, the B.C. government said it would return to a witnessed dosing model. This model — which had been in place prior to the pandemic — will require safer supply participants to take prescribed opioids under the supervision of health-care professionals.
The move follows explosive revelations that more than 60 B.C. pharmacies were allegedly participating in a scheme to overbill the government under its safer supply program. The scheme involved pharmacies incentivizing clients to fill prescriptions they did not require by offering them cash or rewards. Some of those clients then sold the drugs on the black market.
In its Feb. 19 announcement, the province said new participants in the safer supply program would immediately be subject to the witnessed dosing requirement. For existing clients of the program, new guidelines would be forthcoming.
“The Ministry will work with the BC Centre on Substance Use to rapidly develop clinical guidelines to support prescribers that also takes into account what’s best for patients and their safety,” Kendra Wong, a spokesperson for B.C.’s health ministry, told Canadian Affairs in an emailed statement on Feb. 27.
More than a month later, addiction specialists are still waiting.
According to Addiction Medicine Canada’s letter, the BC Centre on Substance Use posed “fundamental questions” to the B.C. government, potentially causing the delay.
“We’re stuck in a place where the government publicly has said it’s told BCCSU to make guidance, and BCCSU has said it’s waiting for government to tell them what to do,” Melamed told Canadian Affairs.
This lag has frustrated addiction specialists, who argue the lack of clear guidance is impeding the transition to witnessed dosing and jeopardizing patient care. They warn that permitting take-home drugs leads to more diversion onto the streets, putting individuals at greater risk.
“Diversion of prescribed alternatives expands the number of people using opioids, and dying from hydromorphone and fentanyl use,” reads the letter, which was also co-signed by Dr. Robert Cooper and Dr. Michael Lester. The doctors are founding board members of Addiction Medicine Canada, a nonprofit that advises on addiction medicine and advocates for research-based treatment options.
“We have had people come in [to our clinic] and say they’ve accessed hydromorphone on the street and now they would like us to continue [prescribing] it,” Melamed told Canadian Affairs.
A spokesperson for the BC Centre on Substance Use declined to comment, referring Canadian Affairs to the Ministry of Health. The ministry was unable to provide comment by the publication deadline.
Big challenges
Under the witnessed dosing model, doctors, nurses and pharmacists will oversee consumption of opioids such as hydromorphone, methadone and morphine in clinics or pharmacies.
The shift back to witnessed dosing will place significant demands on pharmacists and patients. In April 2024, an estimated 4,400 people participated in B.C.’s safer supply program.
Chris Chiew, vice president of pharmacy and health-care innovation at the pharmacy chain London Drugs, told Canadian Affairs that the chain’s pharmacists will supervise consumption in semi-private booths.
Nathan Wong, a B.C.-based pharmacist who left the profession in 2024, fears witnessed dosing will overwhelm already overburdened pharmacists, creating new barriers to care.
“One of the biggest challenges of the retail pharmacy model is that there is a tension between making commercial profit, and being able to spend the necessary time with the patient to do a good and thorough job,” he said.
“Pharmacists often feel rushed to check prescriptions, and may not have the time to perform detailed patient counselling.”
Others say the return to witnessed dosing could create serious challenges for individuals who do not live close to health-care providers.
Shelley Singer, a resident of Cowichan Bay, B.C., on Vancouver Island, says it was difficult to make multiple, daily visits to a pharmacy each day when her daughter was placed on witnessed dosing years ago.
“It was ridiculous,” said Singer, whose local pharmacy is a 15-minute drive from her home. As a retiree, she was able to drive her daughter to the pharmacy twice a day for her doses. But she worries about patients who do not have that kind of support.
“I don’t believe witnessed supply is the way to go,” said Singer, who credits safer supply with saving her daughter’s life.
Melamed notes that not all safer supply medications require witnessed dosing.
“Methadone is under witness dosing because you start low and go slow, and then it’s based on a contingency management program,” she said. “When the urine shows evidence of no other drug, when the person is stable, [they can] take it at home.”
She also noted that Suboxone, a daily medication that prevents opioid highs, reduces cravings and alleviates withdrawal, does not require strict supervision.
Kendra Wong, of the B.C. health ministry, told Canadian Affairs that long-acting medications such as methadone and buprenorphine could be reintroduced to help reduce the strain on health-care professionals and patients.
“There are medications available through the [safer supply] program that have to be taken less often than others — some as far apart as every two to three days,” said Wong.
“Clinicians may choose to transition patients to those medications so that they have to come in less regularly.”
Such an approach would align with Addiction Medicine Canada’s recommendations to the ministry.
The group says it supports supervised dosing of hydromorphone as a short-term solution to prevent diversion. But Melamed said the long-term goal of any addiction treatment program should be to reduce users’ reliance on opioids.
The group recommends combining safer supply hydromorphone with opioid agonist therapies. These therapies use controlled medications to reduce withdrawal symptoms, cravings and some of the risks associated with addiction.
They also recommend limiting unsupervised hydromorphone to a maximum of five 8 mg tablets a day — down from the 30 tablets currently permitted with take-home supplies. And they recommend that doses be tapered over time.
“This protocol is being used with success by clinicians in B.C. and elsewhere,” the letter says.
“Please ensure that the administrative delay of the implementation of your new policy is not used to continue to harm the public.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoTrump Has Driven Canadians Crazy. This Is How Crazy.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoThe Anhui Convergence: Chinese United Front Network Surfaces in Australian and Canadian Elections
-

 Automotive1 day ago
Automotive1 day agoHyundai moves SUV production to U.S.
-

 Entertainment2 days ago
Entertainment2 days agoPedro Pascal launches attack on J.K. Rowling over biological sex views
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoAs PM Poilievre would cancel summer holidays for MP’s so Ottawa can finally get back to work
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoPoilievre Campaigning To Build A Canadian Economic Fortress
-

 armed forces15 hours ago
armed forces15 hours agoYet another struggling soldier says Veteran Affairs Canada offered him euthanasia
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoCarney Liberals pledge to follow ‘gender-based goals analysis’ in all government policy