Opinion
Why treating the Homesless as victims only makes the problem worse

This article is from Substack
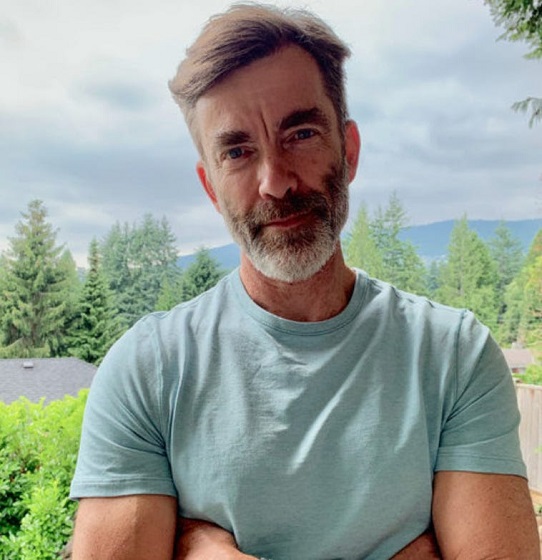
Bestselling author Michael Shellenberger has just published a new book, “San Fransicko” about the homeless crisis in San Francisco. Shellenberger has lived in San Fransisco for 30 years. In “San Fransicko” Shellenberger argues one of the root causes of the homeless crisis sweeping cities all over America (and Canada) is the victimization of homeless people. In this article, Michael Shellenberger talks about the prevalent theory that homeless people are all victims as portrayed by TV Host John Oliver.
Why John Oliver Is Wrong About Homelessness
HBO TV Comedian Repeats Myth that the Homeless Are Just Poor People in Need of Subsidized Housing
The intelligent and hilarious HBO comedian John Oliver last night aired a 25-minute segment on homelessness. In it, he attributed homelessness to poverty, high rents, and NIMBY neighborhood activists who block new housing developments. Oliver showed interviews with homeless people who say they would like to work full-time but are unable to do so because they have to live in homeless shelters.
Unfortunately, Oliver’s segment repeated many myths that are easy to debunk. The vast majority of people we call “homeless” are suffering from serious mental illness, addiction, or both. We do a great job of helping mothers and others who don’t suffer from addiction or untreated mental illness to benefit from subsidized housing, but don’t mandate the psychiatric and addiction care that many “homeless” require. And the best-available, peer-reviewed science shows that “Housing First” agenda Oliver promotes fails on its own terms, worsens addiction, and is one of the main reasons homelessness has grown so much worse.
It’s true that we need more housing and voluntary addiction and psychiatric care, including what is called “permanent supportive housing” for people suffering from mental illness. In my new book, San Fransicko, I advocate for universal psychiatric care, drug treatment on demand, and building of more shelter space for the homeless. And Oliver is right that the U.S. lacks the social safety net that European and other developed nations have.
But Oliver badly misdescribes the problem. For example, he notes that some cities lack sufficient homeless shelter. But he doesn’t acknowledge that it has been “Housing First” homelessness advocates who caused the lack of shelter by demanding that funding be diverted to apartments often costing $750,000 each.
And Oliver promotes policies that have made addiction, mental illness, and homelessness worse. He claims homelessness causes addiction when it is far more often the other way around. And Oliver completely ignores the overwhelming body of scientific research showing that using housing as a reward for abstinence, rather than giving it away as a right, is essential to reducing homelessness by reducing addiction.
Oliver was wrong to encourage more of the same policies that caused homelessness to increase in the U.S. over the last decade, but also wrong for suggesting that anyone who disagreed with him were racist and NIMBY “dicks” who cause violence against homeless people. Oliver closes his segment by ridiculing a white woman who expresses concern about subsidized housing bringing the homeless into her neighborhood.
Why is that? Why does such an intelligent, thoughtful, and compassionate journalist repeat easily-debunked myths about homelessness?
Part of it is just ignorance. Oliver appears to have relied entirely on Housing First advocates and not read anything that questions their narrative. As I document in San Fransicko, homeless advocates are not just small service providers but major academics at top universities including Columbia University and University of California, San Francisco. Those “Housing First” advocates have received hundreds of millions in grants from Marc Benioff, John Arnold, George Soros, and other donors to promote the notion that Housing First works.
Another part of it is ideological. Housing First advocates believe that housing, not shelter, is a right, and that governments have a moral obligation to provide it. They have spent 20 years trying to prove that giving away housing to addicts and the mentally ill works, but the studies show that it fails to address addiction and thus even keep people in apartments at higher rates than other methods. The only thing proven to work is to make housing a reward for good behavior, mostly abstinence but also things like taking one’s psychiatric medicines, and going to work.
The dominant view among progressives of homelessness, drugs, and mental illness stems from victim ideology, which was born in the 1960s. Starting in the late 1960s, progressives attacked any effort to hold people who receive welfare or subsidized accountable as “blaming the victim.” Today, many progressives even view drug dealers as victims.
Victim ideology categorizes people as victims or oppressors, and argues that nothing should be demanded of people categorized as victims. This is terrible for the mentally ill, who often need to be coerced into taking their medicines, so they don’t end up breaking the law, hurting people or themselves, and winding up in prison. And this is terrible for addicts, who need to be arrested, when breaking laws related to their addiction, such as public drug use, shoplifting, and public defecation.
In the end, Oliver’s 25 minute segment on homelessness is a perfect encapsulation of victim ideology and why it is so wrong on both the facts and on ethics. On the facts, Oliver misdescribes a homeless woman who is likely suffering from mental illness and/or drug addiction as merely down on her luck. And Oliver mixes together apparently sober and sane homeless families, temporarily down on their luck, with people are on the street because of addiction and untreated mental illness. Doing so is wrong, analytically, but also wrong, morally, since most addicts and the mentally ill need something very different from just a subsidized apartment unit.
If we are to solve homelessness rather than make it worse, we need intelligent and thoughtful comedians and influencers like Oliver to do their homework, rather than to repeat myths. I researched and wrote San Fransicko, in part, to make it easier for people to get the facts, rather than repeat what we were told, and to see that there’s a better way to help the homeless, whether addicted to drugs, mentally ill, or not.
The good news is that the conversation around drugs and homelessness is changing rapidly because the situation on the ground has grown so much worse. Environmental Progress and the California Peace Coalition are at the very beginning of our efforts to educate journalists, policymakers, and the public. And San Fransicko was published just three weeks ago.
As time passes, many Americans will see the consequence of treating what is fundamentally a problem of untreated mental illness and addiction as a problem of poverty, high rents, and NIMBYs. And some of them, perhaps even comedians like John Oliver, will come to find humor, and humility, from the fact that so many of us got it so wrong.
Addictions
Ontario to restrict Canadian government’s supervised drug sites, shift focus to helping addicts

From LifeSiteNews
Doug Ford’s Progressive Conservative government tabled the Safer Streets, Stronger Communities Act that will place into law specific bans on where such drug consumption sites are located.
Ontario Premier Doug Ford is making good on a promise to close so-called drug “supervision” sites in his province and says his government will focus on helping addicts get better instead of giving them free drugs.
Ford’s Progressive Conservative government on Monday tabled the Safer Streets, Stronger Communities Act that will place into law specific bans on where such drug consumption sites are located.
Specifically, the new bill will ban “supervised” drug consumption sites from being close to schools or childcare centers. Ten sites will close for now, including five in Toronto.
The new law would prohibit the “establishment and operation of a supervised consumption site at a location that is less than 200 meters from certain types of schools, private schools, childcare centers, Early child and family centers and such other premises as may be prescribed by the regulations.”
It would also in effect ban municipalities and local boards from applying for an “exemption from the Controlled Drugs and Substances Act (Canada) for the purpose of decriminalizing the personal possession of a controlled substance or precursor.”
Lastly, the new law would put strict “limits” on the power municipalities and local boards have concerning “applications respecting supervised consumption sites and safer supply services.”
“Municipalities and local boards may only make such applications or support such applications if they have obtained the approval of the provincial Minister of Health,” the bill reads.
The new bill is part of a larger omnibus bill that makes changes relating to sex offenders as well as auto theft, which has exploded in the province in recent months.
In September, Ford had called the federal government’s lax drug policies tantamount to being the “biggest drug dealer in the entire country” and had vowed to act.
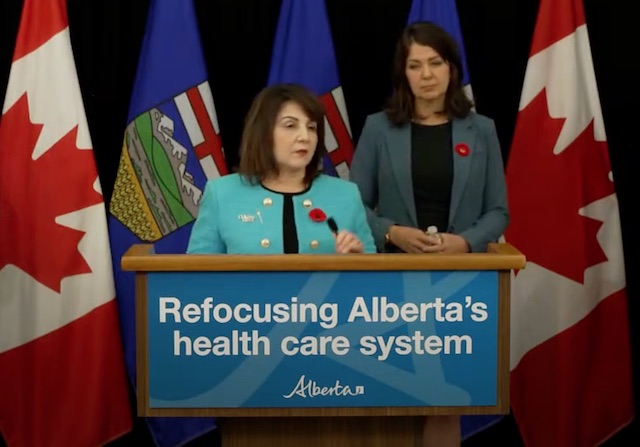
‘No’ new drug sites in Ontario, vows Health Minister
In speaking about the new bill, Ontario Minister of Health Sylvia Jones said the Ford government does not plan to allow municipal requests to the government regarding supervised consumption sites.
“Municipalities and organizations like public health units have to first come to the province because we don’t want them bypassing and getting any federal approval for something that we vehemently disagree with,” Jones told the media on Monday.
She also clarified that “there will be no further safe injection sites in the province of Ontario under our government.”
Ontario will instead create 19 new intensive addiction recovery to help those addicted to deadly drugs.
Alberta and other provinces have had success helping addicts instead of giving them free drugs.
As reported by LifeSiteNews, deaths related to opioid and other drug overdoses in Alberta fell to their lowest levels in years after the Conservative government began to focus on helping addicts via a recovery-based approach instead of the Liberal-minded, so-called “safe-supply” method.
Despite public backlash with respect to supervised drug consumption sites, Health Canada recently approved 16 more drug consumption sites in Ontario. Ford mentioned in the press conference that each day he gets “endless phone calls about needles being in the parks, needles being by the schools and the daycares,” calling the situation “unacceptable.”
The Liberals claim their “safer supply” program is good because it is “providing prescribed medications as a safer alternative to the toxic illegal drug supply to people who are at high risk of overdose.”
However, studies have shown that these programs often lead an excess of deaths from overdose in areas where they are allowed.
While many of the government’s lax drug policies continue, they have been forced to backpedal on some of their most extreme actions.
After the federal government allowed British Columbia to decriminalize the possession of hard drugs including heroin, cocaine, fentanyl, meth and MDMA beginning January 1, 2023, reports of overdoses and chaos began skyrocketing, leading the province to request that Trudeau re-criminalize drugs in public spaces.
A week later, the federal government relented and accepted British Columbia’s request.
Alberta
Alberta’s fiscal update projects budget surplus, but fiscal fortunes could quickly turn

From the Fraser Institute
By Tegan Hill
According to the recent mid-year update tabled Thursday, the Smith government projects a $4.6 billion surplus in 2024/25, up from the $2.9 billion surplus projected just a few months ago. Despite the good news, Premier Smith must reduce spending to avoid budget deficits.
The fiscal update projects resource revenue of $20.3 billion in 2024/25. Today’s relatively high—but very volatile—resource revenue (including oil and gas royalties) is helping finance today’s spending and maintain a balanced budget. But it will not last forever.
For perspective, in just the last decade the Alberta government’s annual resource revenue has been as low as $2.8 billion (2015/16) and as high as $25.2 billion (2022/23).
And while the resource revenue rollercoaster is currently in Alberta’s favor, Finance Minister Nate Horner acknowledges that “risks are on the rise” as oil prices have dropped considerably and forecasters are projecting downward pressure on prices—all of which impacts resource revenue.
In fact, the government’s own estimates show a $1 change in oil prices results in an estimated $630 million revenue swing. So while the Smith government plans to maintain a surplus in 2024/25, a small change in oil prices could quickly plunge Alberta back into deficit. Premier Smith has warned that her government may fall into a budget deficit this fiscal year.
This should come as no surprise. Alberta’s been on the resource revenue rollercoaster for decades. Successive governments have increased spending during the good times of high resource revenue, but failed to rein in spending when resource revenues fell.
Previous research has shown that, in Alberta, a $1 increase in resource revenue is associated with an estimated 56-cent increase in program spending the following fiscal year (on a per-person, inflation-adjusted basis). However, a decline in resource revenue is not similarly associated with a reduction in program spending. This pattern has led to historically high levels of government spending—and budget deficits—even in more recent years.
Consider this: If this fiscal year the Smith government received an average level of resource revenue (based on levels over the last 10 years), it would receive approximately $13,000 per Albertan. Yet the government plans to spend nearly $15,000 per Albertan this fiscal year (after adjusting for inflation). That’s a huge gap of roughly $2,000—and it means the government is continuing to take big risks with the provincial budget.
Of course, if the government falls back into deficit there are implications for everyday Albertans.
When the government runs a deficit, it accumulates debt, which Albertans must pay to service. In 2024/25, the government’s debt interest payments will cost each Albertan nearly $650. That’s largely because, despite running surpluses over the last few years, Albertans are still paying for debt accumulated during the most recent string of deficits from 2008/09 to 2020/21 (excluding 2014/15), which only ended when the government enjoyed an unexpected windfall in resource revenue in 2021/22.
According to Thursday’s mid-year fiscal update, Alberta’s finances continue to be at risk. To avoid deficits, the Smith government should meaningfully reduce spending so that it’s aligned with more reliable, stable levels of revenue.
Author:
-

 Brownstone Institute2 days ago
Brownstone Institute2 days agoThe Most Devastating Report So Far
-

 Business2 days ago
Business2 days agoCarbon tax bureaucracy costs taxpayers $800 million
-

 ESG2 days ago
ESG2 days agoCan’t afford Rent? Groceries for your kids? Trudeau says suck it up and pay the tax!
-

 John Stossel2 days ago
John Stossel2 days agoGreen Energy Needs Minerals, Yet America Blocks New Mines
-

 Daily Caller2 days ago
Daily Caller2 days agoLos Angeles Passes ‘Sanctuary City’ Ordinance In Wake Of Trump’s Deportation Plan
-

 Alberta2 days ago
Alberta2 days agoProvince considering new Red Deer River reservoir east of Red Deer
-
 Addictions2 days ago
Addictions2 days agoBC Addictions Expert Questions Ties Between Safer Supply Advocates and For-Profit Companies
-

 Aristotle Foundation1 day ago
Aristotle Foundation1 day agoToronto cancels history, again: The irony and injustice of renaming Yonge-Dundas Square to Sankofa Square