Alberta
Dozens of liquor violations and other infractions – Sylvan Lake RCMP step up presence at beach and parks

News Release from Sylvan Lake RCMP
Sylvan Lake RCMP advise of increased presence due to concerning behaviours and infractions
The recent hot weather and removal of COVID restrictions lead to Albertans flocking to recreational areas over the Canada Day weekend. Although Albertans are encouraged to take full advantage of the beautiful landscapes and everything this amazing province has to offer, the Sylvan Lake RCMP would like to remind recreational enthusiasts that Alberta’s Provincial liquor and cannabis laws apply in public areas.
Sylvan Lake RCMP, in partnership with Town of Sylvan Lake Peace Officers, continue to provide an increased presence in and around the parks and beaches of Sylvan Lake and area due to an increase in concerning behaviors.
In recent weeks, RCMP have charged dozens of liquor related infractions under the Gaming and Liquor Act over the long weekend. 49 liquor tickets were handed out among other infractions. Several complaints have been received in regards to underage drinking and assaults.
Under the GLA, it is an offence to have open liquor in public places that are not temporary residences (such as campsites and motorhomes), or designated picnic areas. Open liquor is prohibited in all other public places, and can result in fines of $120.
“Our priority is to ensure everyone has a safe and enjoyable summer in our beautiful town,” says Staff Sergeant Jeff McBeth, Detachment Commander of Sylvan Lake RCMP. “Together, we can make this happen.”
Sylvan Lake RCMP are asking for the public’s assistance in reporting suspicious activity in these areas. Please contact the Sylvan Lake RCMP at 403-858-7200. If you wish to remain anonymous, you can contact Crime Stoppers at 1-800-222-8477 (TIPS), online at www.P3Tips.com or by using the “P3 Tips” app available through the Apple App or Google Play Store.
Alberta
Made in Alberta! Province makes it easier to support local products with Buy Local program

Show your Alberta side. Buy Local. |
When the going gets tough, Albertans stick together. That’s why Alberta’s government is launching a new campaign to benefit hard-working Albertans.
Global uncertainty is threatening the livelihoods of hard-working Alberta farmers, ranchers, processors and their families. The ‘Buy Local’ campaign, recently launched by Alberta’s government, encourages consumers to eat, drink and buy local to show our unified support for the province’s agriculture and food industry.
The government’s ‘Buy Local’ campaign encourages consumers to buy products from Alberta’s hard-working farmers, ranchers and food processors that produce safe, nutritious food for Albertans, Canadians and the world.
“It’s time to let these hard-working Albertans know we have their back. Now, more than ever, we need to shop local and buy made-in-Alberta products. The next time you are grocery shopping or go out for dinner or a drink with your friends or family, support local to demonstrate your Alberta pride. We are pleased tariffs don’t impact the ag industry right now and will keep advocating for our ag industry.”
Alberta’s government supports consumer choice. We are providing tools to help folks easily identify Alberta- and Canadian-made foods and products. Choosing local products keeps Albertans’ hard-earned dollars in our province. Whether it is farm-fresh vegetables, potatoes, honey, craft beer, frozen food or our world-renowned beef, Alberta has an abundance of fresh foods produced right on our doorstep.
Quick facts
- This summer, Albertans can support local at more than 150 farmers’ markets across the province and meet the folks who make, bake and grow our food.
- In March 2023, the Alberta government launched the ‘Made in Alberta’ voluntary food and beverage labelling program to support local agriculture and food sectors.
- Through direct connections with processors, the program has created the momentum to continue expanding consumer awareness about the ‘Made in Alberta’ label to help shoppers quickly identify foods and beverages produced in our province.
- Made in Alberta product catalogue website
Related information
Alberta
Province to expand services provided by Alberta Sheriffs: New policing option for municipalities

Expanding municipal police service options |
Proposed amendments would help ensure Alberta’s evolving public safety needs are met while also giving municipalities more options for local policing.
As first announced with the introduction of the Public Safety Statutes Amendment Act, 2024, Alberta’s government is considering creating a new independent agency police service to assume the police-like duties currently performed by Alberta Sheriffs. If passed, Bill 49 would lay additional groundwork for the new police service.
Proposed amendments to the Police Act recognize the unique challenges faced by different communities and seek to empower local governments to adopt strategies that effectively respond to their specific safety concerns, enhancing overall public safety across the province.
If passed, Bill 49 would specify that the new agency would be a Crown corporation with an independent board of directors to oversee its day-to-day operations. The new agency would be operationally independent from the government, consistent with all police services in Alberta. Unlike the Alberta Sheriffs, officers in the new police service would be directly employed by the police service rather than by the government.
“With this bill, we are taking the necessary steps to address the unique public safety concerns in communities across Alberta. As we work towards creating an independent agency police service, we are providing an essential component of Alberta’s police framework for years to come. Our aim is for the new agency is to ensure that Albertans are safe in their communities and receive the best possible service when they need it most.”
Additional amendments would allow municipalities to select the new agency as their local police service once it becomes fully operational and the necessary standards, capacity and frameworks are in place. Alberta’s government is committed to ensuring the new agency works collaboratively with all police services to meet the province’s evolving public safety needs and improve law enforcement response times, particularly in rural communities. While the RCMP would remain the official provincial police service, municipalities would have a new option for their local policing needs.
Once established, the agency would strengthen Alberta’s existing policing model and complement the province’s current police services, which include the RCMP, Indigenous police services and municipal police. It would help fill gaps and ensure law enforcement resources are deployed efficiently across the province.
Related information
-

 Bruce Dowbiggin2 days ago
Bruce Dowbiggin2 days agoIs HNIC Ready For The Winnipeg Jets To Be Canada’s Heroes?
-

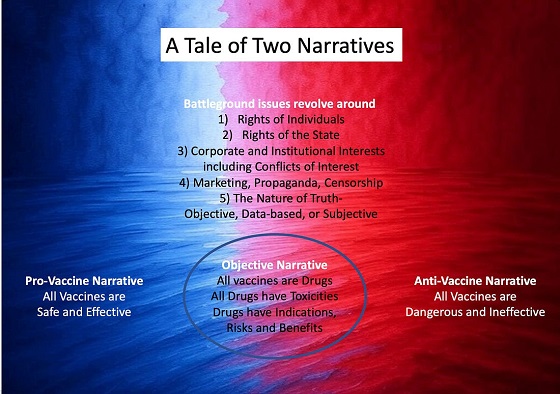
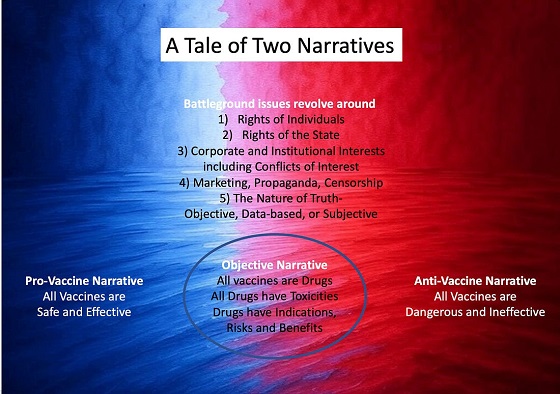
 COVID-192 days ago
COVID-192 days agoCOVID virus, vaccines are driving explosion in cancer, billionaire scientist tells Tucker Carlson
-
 Dr. Robert Malone2 days ago
Dr. Robert Malone2 days agoThe West Texas Measles Outbreak as a Societal and Political Mirror
-

 illegal immigration1 day ago
illegal immigration1 day agoDespite court rulings, the Trump Administration shows no interest in helping Abrego Garcia return to the U.S.
-

 Health2 days ago
Health2 days agoHorrific and Deadly Effects of Antidepressants
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoConservative MP Leslyn Lewis warns Canadian voters of Liberal plan to penalize religious charities
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoEuthanasia is out of control in Canada, but nobody is talking about it on the campaign trail
-

 Education1 day ago
Education1 day agoSchools should focus on falling math and reading grades—not environmental activism