Health
Larger Heliport Now Open At Rocky Health Centre

Residents in the Rocky Mountain House Region now have improved access to critical care, thanks to the new, larger heliport now being operational. Officials with Alberta Health Services have shared the following news release outlining those details:
The new and bigger heliport at the Rocky Mountain House Health Centre is now operational.
Transport Canada has issued a flight certificate confirming air ambulance helicopters, including STARS, can now land at the Alberta Health Services (AHS) facility.
“We are pleased to announce the heliport is operational in time for the August long weekend,” says Kerry Bales, Chief Zone Officer of AHS Central Zone. “It has been a lengthy process but we have very much appreciated the collaboration with the town and community.”
The new heliport can accommodate both models of STARS helicopters: the BK 117 and the AW139. A town-owned water tower near the flight path had to be removed or painted before Transport Canada could give approval to land at the heliport. The tower was dismantled this spring; the Transport Canada inspection occurred July 26.
“A super job well done,” says Rocky Mountain House Mayor Fred Nash. “It’s been a pleasure working with the professionalism of Alberta Health Services for the betterment of the town of Rocky Mountain House, the county and the many visitors who come here.”
Until now, all STARS helicopters were landing at the Rocky Mountain House airport, located about eight kilometres from the health centre. Ground ambulances were used to transport patients to and from the health centre and airport.
“The ability to have all sizes of medevac helicopters land right here at the Rocky Mountain House Health Centre will improve access for patients who need critical care transport,” says Bales.
STARS helicopters are more than an ambulance in the air; they are sophisticated medical environments brought directly to the patient. This can mean the difference in the health outcome of a patient when time is of the essence.
On board, a full array of medications and equipment is at the disposal of the air medical crew. STARS personnel are able to administer life-saving drugs, defibrillate a patient’s heart, transfuse blood, and peer inside a patient using portable ultrasound.
“Many lives have been saved because of our ability to provide transport and medical expertise to critically ill and injured patients via air ambulance,” says Mike Lamacchia, Vice President of Alberta and Saskatchewan Operations at STARS.
AHS’ Emergency Medical Services (EMS) team, including dispatch services, ground ambulances and fixed-wing air ambulances, work with STARS as a key partner to provide an integrated emergency medical response service. STARS physicians, nurses, paramedics and pilots work with a team of dedicated support staff and community partners to be there for Albertans and to save lives 24/7.
AHS spent $430,000 to pay for the tower demolition and the relocation of the town, county and regional fire communication antennas that were located on top of the tower.
Alberta Health Services is the provincial health authority responsible for planning and delivering health supports and services for more than four million adults and children living in Alberta. Its mission is to provide a patient-focused, quality health system that is accessible and sustainable for all Albertans.
Alberta
Alberta takes big step towards shorter wait times and higher quality health care

From the Fraser Institute
On Monday, the Smith government announced that beginning next year it will change the way it funds surgeries in Alberta. This is a big step towards unlocking the ability of Alberta’s health-care system to provide more, better and faster services for the same or possibly fewer dollars.
To understand the significance of this change, you must understand the consequences of the current (and outdated) approach.
Currently, the Alberta government pays a lump sum of money to hospitals each year. Consequently, hospitals perceive patients as a drain on their budgets. From the hospital’s perspective, there’s little financial incentive to serve more patients, operate more efficiently and provide superior quality services.
Consider what would happen if your local grocery store received a giant bag of money each year to feed people. The number of items would quickly decline to whatever was most convenient for the store to provide. (Have a favourite cereal? Too bad.) Store hours would become less convenient for customers, alongside a general decline in overall service. This type of grocery store, like an Alberta hospital, is actually financially better off (that is, it saves money) if you go elsewhere.
The Smith government plans to flip this entire system on its head, to the benefit of patients and taxpayers. Instead of handing out bags of money each year to providers, the new system—known as “activity-based funding”—will pay health-care providers for each patient they treat, based on the patient’s particular condition and important factors that may add complexity or cost to their care.
This turns patients from a drain on budgets into a source of additional revenue. The result, as has been demonstrated in other universal health-care systems worldwide, is more services delivered using existing health-care infrastructure, lower wait times, improved quality of care, improved access to medical technologies, and less waste.
In other words, Albertans will receive far better value from their health-care system, which is currently among the most expensive in the world. And relief can’t come soon enough—for example, last year in Alberta the median wait time for orthopedic surgeries including hip and knee replacements was 66.8 weeks.
The naysayers argue this approach will undermine the province’s universal system and hurt patients. But by allowing a spectrum of providers to compete for the delivery of quality care, Alberta will follow the lead of other more successful universal health-care systems in countries such as Australia, Germany, the Netherlands and Switzerland and create greater accountability for hospitals and other health-care providers. Taxpayers will get a much better picture of what they’re paying for and how much they pay.
Again, Alberta is not exploring an untested policy. Almost every other developed country with universal health care uses some form of “activity-based funding” for hospital and surgical care. And remember, we already spend more on health care than our counterparts in nearly all of these countries yet endure longer wait times and poorer access to services generally, in part because of how we pay for surgical care.
While the devil is always in the details, and while it’s still possible for the Alberta government to get this wrong, Monday’s announcement is a big step in the right direction. A funding model that puts patients first will get Albertans more of the high-quality health care they already pay for in a timelier fashion. And provide to other provinces an example of bold health-care reform.
Alberta
Alberta’s embrace of activity-based funding is great news for patients

 From the Montreal Economic Institute
From the Montreal Economic Institute
Alberta’s move to fund acute care services through activity-based funding follows best practices internationally, points out an MEI researcher following an announcement made by Premier Danielle Smith earlier today.
“For too long, the way hospitals were funded in Alberta incentivized treating fewer patients, contributing to our long wait times,” explains Krystle Wittevrongel, director of research at the MEI. “International experience has shown that, with the proper funding models in place, health systems become more efficient to the benefit of patients.”
Currently, Alberta’s hospitals are financed under a system called “global budgeting.” This involves allocating a pre-set amount of funding to pay for a specific number of services based on previous years’ budgets.
Under the government’s newly proposed funding system, hospitals receive a fixed payment for each treatment delivered.
An Economic Note published by the MEI last year showed that Quebec’s gradual adoption of activity-based funding led to higher productivity and lower costs in the province’s health system.
Notably, the province observed that the per-procedure cost of MRIs fell by four per cent as the number of procedures performed increased by 22 per cent.
In the radiology and oncology sector, it observed productivity increases of 26 per cent while procedure costs decreased by seven per cent.
“Being able to perform more surgeries, at lower costs, and within shorter timelines is exactly what Alberta’s patients need, and Premier Smith understands that,” continued Mrs. Wittevrongel. “Today’s announcement is a good first step, and we look forward to seeing a successful roll-out once appropriate funding levels per procedure are set.”
The governments expects to roll-out this new funding model for select procedures starting in 2026.
* * *
The MEI is an independent public policy think tank with offices in Montreal, Ottawa, and Calgary. Through its publications, media appearances, and advisory services to policymakers, the MEI stimulates public policy debate and reforms based on sound economics and entrepreneurship.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoHarper Endorses Poilievre at Historic Edmonton Rally: “This Crisis Was Made in Canada”
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoMark Carney’s radical left-wing, globalist record proves he is Justin Trudeau 2.0
-
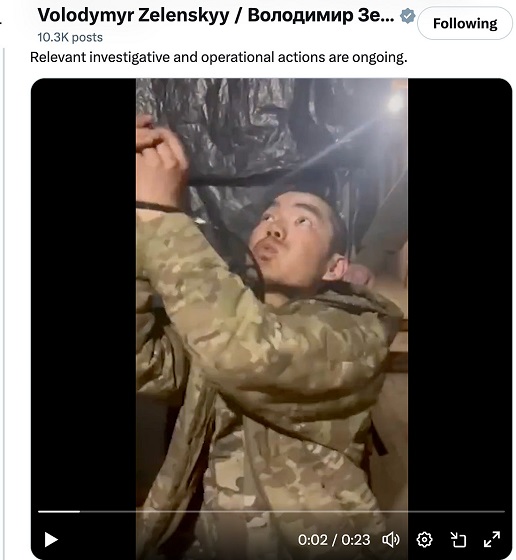 conflict2 days ago
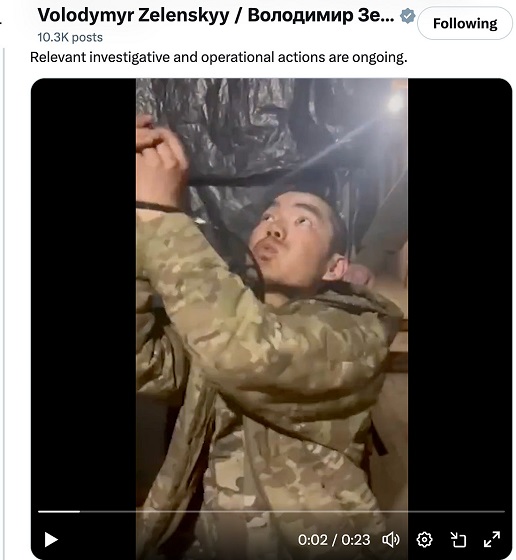
conflict2 days agoZelensky Alleges Chinese Nationals Fighting for Russia, Calls for Global Response
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoAn In-Depth Campaign Trail “Interview” With Pierre Poilievre
-

 2025 Federal Election20 hours ago
2025 Federal Election20 hours agoConservative Party urges investigation into Carney plan to spend $1 billion on heat pumps
-

 Business2 days ago
Business2 days agoTrump’s tariff plan replaces free trade with balanced trade. Globalists hate that.
-

 Censorship Industrial Complex2 days ago
Censorship Industrial Complex2 days agoScott Atlas: COVID lockdowns, censorship have left a ‘permanent black mark on America’
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoDon’t double-down on net zero again