Alberta
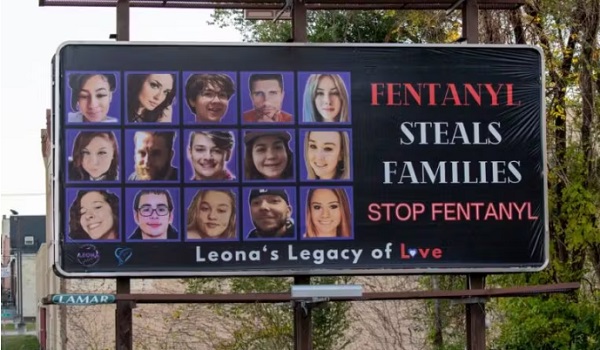
The Good Samaritan Drug Overdose Act could help save lives

From Alberta RCMP
Alberta RCMP remind citizens of the Good Samaritan Drug Overdose Act
From January 2016 to December 2018, 1,971 deaths in the province of Alberta have been attributed to apparent opioid-related overdoses. Alberta RCMP were dispatched to several of those incidents and determined that, in some cases, it is believed that bystanders, friends or family members were hesitant to call emergency services for assistance due to concerns of potential legal repercussions. Every overdose death is tragic, and many of these potential tragedies can be avoided if people who witness overdose situations seek emergency help promptly.
To encourage people to seek potentially life-saving emergency help in an overdose situation, the RCMP, in collaboration with Heath Canada and the Chief Medical Officer of Health of Alberta, want to remind residents of the Good Samaritan Drug Overdose Act, which provides some legal protections for people who experience or witness an overdose and call 911 or their local emergency number for help.
Legal protection granted by the Act
The Act is meant to encourage people to seek emergency help during an overdose by helping to reduce fear of seeking police or medical assistance. It applies to anyone seeking emergency assistance during an overdose, including the person experiencing an overdose. The Act protects the person who seeks help, whether they stay or leave from the overdose scene, as well as anyone else who is at the scene when help arrives.
The Act can protect you from:
- Charges for possession of a controlled substance (i.e. drugs) under section 4(1) of the Controlled Drugs and Substances Act
- Consequences of breach of conditions regarding simple possession of controlled substances (i.e. drugs) in: pre-trial release, probation orders, conditional sentences and parole.
It is important to note that the Act does not provide legal protection against more serious offences, such as: production and trafficking of controlled substances, and all other crimes not outlined within the Act.
How to help save a life
Drug overdoses could happen to someone close to you – a friend, a family member, or someone nearby. Staying at the scene is important to help save the life of the person experiencing an overdose.
Witnesses should call for emergency help and render whatever assistance they can, including administering naloxone – a fast-acting drug that temporarily reverses the effects of opioid overdoses – if it is available, providing first aid, including rescue breathing (CPR) if necessary until help arrives, and staying calm and reassuring the person that help is on the way.
The Good Samaritan Drug Overdose Act is part of the Government of Canada’s comprehensive approach to addressing the opioid crisis.
You can learn more at Canada.ca/Opioids.
Alberta
Alberta takes big step towards shorter wait times and higher quality health care

From the Fraser Institute
On Monday, the Smith government announced that beginning next year it will change the way it funds surgeries in Alberta. This is a big step towards unlocking the ability of Alberta’s health-care system to provide more, better and faster services for the same or possibly fewer dollars.
To understand the significance of this change, you must understand the consequences of the current (and outdated) approach.
Currently, the Alberta government pays a lump sum of money to hospitals each year. Consequently, hospitals perceive patients as a drain on their budgets. From the hospital’s perspective, there’s little financial incentive to serve more patients, operate more efficiently and provide superior quality services.
Consider what would happen if your local grocery store received a giant bag of money each year to feed people. The number of items would quickly decline to whatever was most convenient for the store to provide. (Have a favourite cereal? Too bad.) Store hours would become less convenient for customers, alongside a general decline in overall service. This type of grocery store, like an Alberta hospital, is actually financially better off (that is, it saves money) if you go elsewhere.
The Smith government plans to flip this entire system on its head, to the benefit of patients and taxpayers. Instead of handing out bags of money each year to providers, the new system—known as “activity-based funding”—will pay health-care providers for each patient they treat, based on the patient’s particular condition and important factors that may add complexity or cost to their care.
This turns patients from a drain on budgets into a source of additional revenue. The result, as has been demonstrated in other universal health-care systems worldwide, is more services delivered using existing health-care infrastructure, lower wait times, improved quality of care, improved access to medical technologies, and less waste.
In other words, Albertans will receive far better value from their health-care system, which is currently among the most expensive in the world. And relief can’t come soon enough—for example, last year in Alberta the median wait time for orthopedic surgeries including hip and knee replacements was 66.8 weeks.
The naysayers argue this approach will undermine the province’s universal system and hurt patients. But by allowing a spectrum of providers to compete for the delivery of quality care, Alberta will follow the lead of other more successful universal health-care systems in countries such as Australia, Germany, the Netherlands and Switzerland and create greater accountability for hospitals and other health-care providers. Taxpayers will get a much better picture of what they’re paying for and how much they pay.
Again, Alberta is not exploring an untested policy. Almost every other developed country with universal health care uses some form of “activity-based funding” for hospital and surgical care. And remember, we already spend more on health care than our counterparts in nearly all of these countries yet endure longer wait times and poorer access to services generally, in part because of how we pay for surgical care.
While the devil is always in the details, and while it’s still possible for the Alberta government to get this wrong, Monday’s announcement is a big step in the right direction. A funding model that puts patients first will get Albertans more of the high-quality health care they already pay for in a timelier fashion. And provide to other provinces an example of bold health-care reform.
Alberta
Alberta’s embrace of activity-based funding is great news for patients

 From the Montreal Economic Institute
From the Montreal Economic Institute
Alberta’s move to fund acute care services through activity-based funding follows best practices internationally, points out an MEI researcher following an announcement made by Premier Danielle Smith earlier today.
“For too long, the way hospitals were funded in Alberta incentivized treating fewer patients, contributing to our long wait times,” explains Krystle Wittevrongel, director of research at the MEI. “International experience has shown that, with the proper funding models in place, health systems become more efficient to the benefit of patients.”
Currently, Alberta’s hospitals are financed under a system called “global budgeting.” This involves allocating a pre-set amount of funding to pay for a specific number of services based on previous years’ budgets.
Under the government’s newly proposed funding system, hospitals receive a fixed payment for each treatment delivered.
An Economic Note published by the MEI last year showed that Quebec’s gradual adoption of activity-based funding led to higher productivity and lower costs in the province’s health system.
Notably, the province observed that the per-procedure cost of MRIs fell by four per cent as the number of procedures performed increased by 22 per cent.
In the radiology and oncology sector, it observed productivity increases of 26 per cent while procedure costs decreased by seven per cent.
“Being able to perform more surgeries, at lower costs, and within shorter timelines is exactly what Alberta’s patients need, and Premier Smith understands that,” continued Mrs. Wittevrongel. “Today’s announcement is a good first step, and we look forward to seeing a successful roll-out once appropriate funding levels per procedure are set.”
The governments expects to roll-out this new funding model for select procedures starting in 2026.
* * *
The MEI is an independent public policy think tank with offices in Montreal, Ottawa, and Calgary. Through its publications, media appearances, and advisory services to policymakers, the MEI stimulates public policy debate and reforms based on sound economics and entrepreneurship.
-

 Also Interesting1 day ago
Also Interesting1 day agoMortgage Mayhem: How Rising Interest Rates Are Squeezing Alberta Homeowners
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoConservative Party urges investigation into Carney plan to spend $1 billion on heat pumps
-

 Alberta2 days ago
Alberta2 days agoAlberta’s embrace of activity-based funding is great news for patients
-
 2025 Federal Election2 days ago
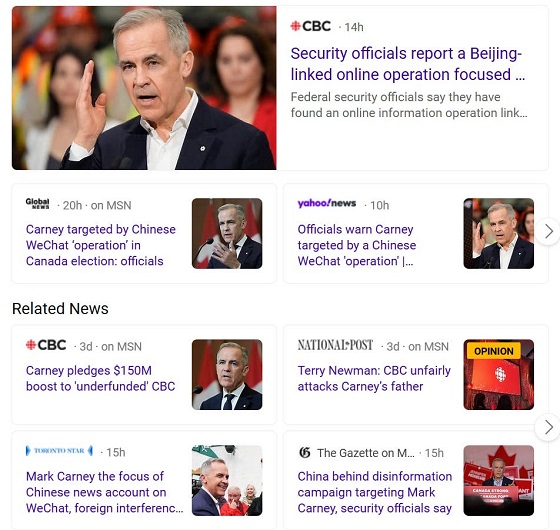
2025 Federal Election2 days agoCommunist China helped boost Mark Carney’s image on social media, election watchdog reports
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoCorporate Media Isn’t Reporting on Foreign Interference—It’s Covering for It
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoFifty Shades of Mark Carney
-

 Also Interesting2 days ago
Also Interesting2 days agoExploring Wildrobin Technological Advancements in Live Dealer Games
-

 Justice1 day ago
Justice1 day agoCanadian government sued for forcing women to share spaces with ‘transgender’ male prisoners