Health
Recovered ‘brain dead’ man dancing at sister’s wedding reminds us organ donors are sometimes alive

TJ Hoover and his sister on her wedding day
From LifeSiteNews
Since brain dead people are not dead, it is not surprising that the only multicenter, prospective study of brain death found that the majority of brains from ‘brain dead’ people were not severely damaged at autopsy.
In 2021, a supposedly brain dead man, Anthony Thomas “TJ” Hoover II, opened his eyes and looked around while being wheeled to the operating room to donate his organs. Hospital staff at Baptist Health hospital in Richmond, Kentucky assured his family that these were just “reflexes.”
But organ preservationist Natasha Miller also thought Hoover looked alive. “He was moving around – kind of thrashing. Like, moving, thrashing around on the bed,” said Miller in an NPR interview. “And then when we went over there, you could see he had tears coming down. He was visibly crying.” Thankfully, the procedure was called off, and Hoover was able to recover and even dance at his sister’s wedding this past summer.
Last month, this case was brought before a U.S. House subcommittee investigating organ procurement organizations. Whistleblowers claimed that even after two doctors refused to remove Hoover’s organs, Kentucky Organ Donor Affiliates ordered their staff to find another doctor to perform the surgery.
Because brain death is a social construct and not death itself, I can tell you exactly how many “brain dead” patients are still alive: all of them. When brain death was first proposed by an ad hoc committee at Harvard Medical School in 1968, the committee admitted that these people are not dead, but rather “desperately injured.” They thought that these neurologically injured people were a burden to themselves and others, and that society would be better served if we redefined them as being “dead.” They described their reasoning this way:
Our primary purpose is to define irreversible coma as a new criterion for death. There are two reasons why there is need for a definition: (1) Improvements in resuscitative and supportive measures have led to increased efforts to save those who are desperately injured. Sometimes these efforts have only partial success so that the result is an individual whose heart continues to beat but whose brain is irreversibly damaged. The burden is great on patients who suffer permanent loss of intellect, on their families, on the hospitals, and on those in need of hospital beds already occupied by these comatose patients. (2) Obsolete criteria for the definition of death can lead to controversy in obtaining organs for transplantation.
Since brain dead people are not dead, it is not surprising that the only multicenter, prospective study of brain death found that the majority of brains from “brain dead” people were not severely damaged at autopsy – and 10 actually looked normal. Dr. Gaetano Molinari, one of the study’s principal investigators, wrote:
[D]oes a fatal prognosis permit the physician to pronounce death? It is highly doubtful whether such glib euphemisms as “he’s practically dead,” … “he can’t survive,” … “he has no chance of recovery anyway,” will ever be acceptable legally or morally as a pronouncement that death has occurred.
But history shows that despite Dr. Molinari’s doubts, “brain death,” a prognosis of possible death, went on to be widely accepted as death per se. Brain death was enshrined into US law in 1981 under the Uniform Determination of Death Act. Acceptance of this law has allowed neurologically disabled people to be redefined as “dead” and used as organ donors. Unfortunately, most of these people do not, like TJ Hoover, wake up in time. They suffer death through the harvesting of their organs, a procedure often performed without the benefit of anesthesia.
Happily, some do manage to avoid becoming organ donors and go on to receive proper medical treatment. In 1985, Jennifer Hamann was thrown into a coma after being given a prescription that was incompatible with her epilepsy medication. She could not move or sign that she was awake and aware when she overheard doctors saying that her husband was being “completely unreasonable” because he would not donate her organs. She went on to made a complete recovery and became a registered nurse.
Zack Dunlap was declared brain dead in 2007 following an ATV accident. Even though his cousin demonstrated that Zack reacted to pain, hospital staff told his family that it was just “reflexes.” But as Zack’s reactions became more vigorous, the staff took more notice and called off the organ harvesting team that was just landing via helicopter to take Zack’s organs. Today, Zack leads a fully recovered life.
Colleen Burns was diagnosed “brain dead” after a drug overdose in 2009, but wasn’t given adequate testing and awoke on the operating table just minutes before her organ harvesting surgery. Because the Burns family declined to sue, the hospital only received a slap on the wrist: the State Health Department fined St. Joseph’s Hospital Health Center in Syracuse, New York, just $6,000.
In 2015, George Pickering III was declared brain dead, but his father thought doctors were moving too fast. Armed and dangerous, he held off a SWAT team for three hours, during which time his son began to squeeze his hand on command. “There was a law broken, but it was broken for all the right reasons. I’m here now because of it,” said George III.
Trenton McKinley, a 13-year-old boy, suffered a head injury in 2018 but regained consciousness after his parents signed paperwork to donate his organs. His mother told CBS News that signing the consent to donate allowed doctors to continue Trenton’s intensive care treatment, ultimately giving him time to wake up.
Doctors often say that cases like these prove nothing, and that they are obviously the result of misdiagnosis and medical mistakes. But since all these people were about to become organ donors regardless of whether their diagnoses were correct, I doubt they find the “mistake” excuse comforting.
However, Jahi McMath was indisputably diagnosed as being “brain dead” correctly. She was declared brain dead by three different doctors, she failed three apnea tests, and she had four flat-line EEGs, as well as a cerebral perfusion scan showing “no flow.” But because her parents refused to make her an organ donor and insisted on continuing her medical care, McMath recovered to the point of being able to follow commands. Two neurologists later testified that she was no longer brain dead, but a in minimally conscious state. Her case shows that people correctly declared “brain dead” can still recover.
READ: Woman with no brainwave activity wakes up after hearing her daughter’s voice
Brain death is not death because the brain death concept does not reflect the reality of the phenomenon of death. Therefore, any guideline for its diagnosis will have no basis in scientific facts. People declared brain dead are neurologically disabled, but they are still alive. “Brain dead” organ donation is a concealed form of euthanasia.
Heidi Klessig MD is a retired anesthesiologist and pain management specialist who writes and speaks on the ethics of organ harvesting and transplantation. She is the author of “The Brain Death Fallacy” and her work may be found at respectforhumanlife.com.
Alberta
Province says Alberta family doctors will be the best-paid and most patient-focused in the country

Dr. Shelley Duggan, president, Alberta Medical Association
New pay model, better access to family doctors |
Alberta’s government is implementing a new primary care physician compensation model to improve access to family physicians across the province.
Alberta’s government recognizes that family physicians are fundamental to strengthening the health care system. Unfortunately, too many Albertans do not currently have access to regular primary care from a family physician. This is why, last year, the government entered into a memorandum of understanding with the Alberta Medical Association (AMA) and committed to developing a new primary care physician compensation model.
Alberta’s government will now be implementing a new compensation model for family doctors to ensure they continue practising in the province and to attract more doctors to choose Alberta, which will also alleviate pressures in other areas of the health care system.
This new model will make Alberta’s family doctors the strongest-paid and most patient-focused in the country.
“Albertans must be able to access a primary care provider. We’ve been working hard with our partners at the Alberta Medical Association to develop a compensation model that will not only support Alberta’s doctors but also improve Albertans’ access to physicians. Ultimately, our deal will make Alberta an even more attractive place to practise family medicine.”
“We have worked with the Alberta Medical Association to address the challenges that primary care physicians are facing. This model will provide the supports physicians need and improve patient access to the care they need.”
The new model is structured to encourage physicians to grow the number of patients they care for and encourage full-time practice. Incentives include increases for:
- Maintaining high panel numbers (minimum of 500 patients), which will incentivize panel growth and improve access to primary care for patients.
- Providing after-hours care to relieve pressure on emergency departments and urgent care centres.
- Improving technology to encourage using tools that help streamline work and enhance patient care.
- Enhancing team-based care, which will encourage developing integrated teams that may include family physicians, nurse practitioners, registered nurses, dietitians and pharmacists to provide patients with the best care possible.
- Adding efficiencies in clinical operations to simplify processes for both patients and health care providers.
As a market and evidence-based model, it recognizes and pays for the critically important work of physicians, including the number of patients seen and patient complexity, as well as time spent providing direct and indirect care.
“Family medicine is the foundation of our health care system. This model recognizes the extensive training, experience and leadership of primary care physicians, and we hope it will help Alberta to attract and retain more family medicine specialists who provide comprehensive care.”
Additionally, family physicians who are not compensated through the traditional fee-for-service model will now receive higher pay rates under their payment model, known as the alternative relationship plan. This includes those who provide inpatient care in hospitals and rural generalists. Alberta’s government is increasing this to ensure hospital-based family physicians and rural generalists also receive fair, competitive pay that reflects the importance of these roles.
“This new compensation model will make Alberta more attractive for physicians and will make sure more Albertans can have improved access to a primary care provider no matter where they live. It will also help support efforts to strengthen primary care in Alberta as the foundation of the health care system.”
“Family physicians have been anxiously awaiting this announcement about the new compensation model. We anticipate this model will allow many primary care physicians to continue to deliver comprehensive, lifelong care to their patients while keeping their community clinics viable.”
Quick facts
- Enrolment in the primary care physician compensation model will begin in January with full implementation in spring 2025, provided there are at least 500 physicians enrolled.
- The alternative relationship plan rate has not been updated since it was initially calculated in 2002.
- The new compensation model for family doctors is the latest primary health care improvement following actions that include:
- A $42-million investment to recruit more health providers and expand essential services.
- A new rural and remote bursary program for family medicine resident physicians.
- Additional funding of $257 million to stabilize primary care delivery and improve access to family physicians.
- Implementing the Nurse Practitioner Primary Care Program, which expands the role of nurse practitioners by allowing them to practise comprehensive patient care autonomously, either by operating their own practices or working independently within existing primary care settings.
Related information
Health
Trump doubles down on using RFK Jr. to study possible link between vaccines and autism

From LifeSiteNews
By Stephen Kokx
During a free-flowing press conference at Mar-a-Lago Monday, Donald Trump mentioned the sharp rise in autism in recent decades, adding that he has experts ‘looking to find out’ if vaccines may be the cause.
Donald Trump is doubling down on his intention to study a possible link between vaccines and autism in children.
During a free-flowing press conference at Mar-a-Lago Monday, the incoming president said there are “problems” with the massive increase in autism cases in America over the past several decades and that he intends to get to the bottom of it.
“30 years ago, we had, I’ve heard numbers like 1 in 200,000, 1 in 100,000. Now I’m hearing numbers like 1 in 100. So, something’s wrong … and we’re going to find out about it,” he said.
Trump’s remarks come just days after he told MSNBC anchor Kristen Welker that his choice to lead the Heath and Human Services Department, Robert F. Kennedy Jr., will be tasked with investigating the matter.
“Certain vaccines are incredible but maybe some aren’t, and if they aren’t, we have to find out … the drug companies are going to be working with RFK Jr,” he said.
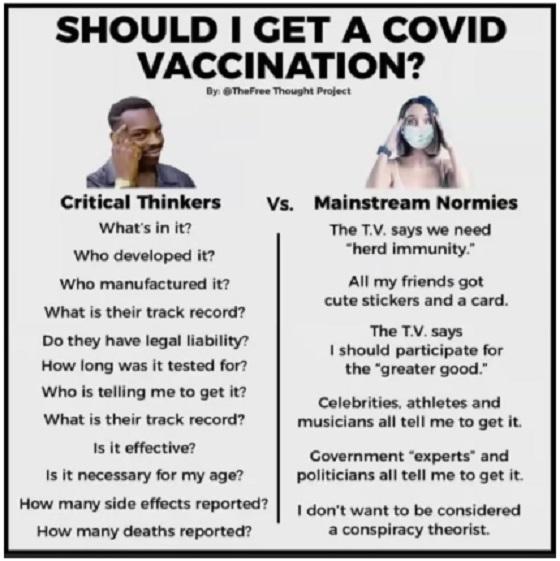
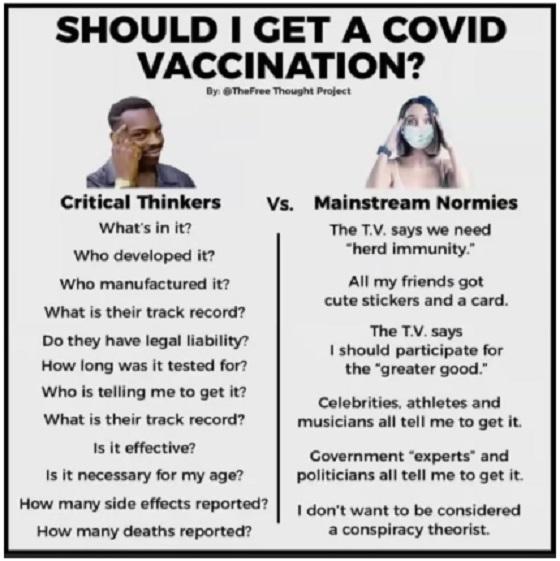
During COVID-19, Dr. Sherri Tenpenny joined a LifeSiteNews panel discussion on the science regarding the COVID shots. She warned that the experimental injections do not even qualify for the term “vaccine.”
“I refuse to call it a vaccine because it doesn’t meet any of the standards by which a vaccine is supposed to work,” she said.
In October 2022, the U.S. Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) unanimously voted 15-0 to add COVID-19 shots to the U.S. childhood, adolescent and adult vaccine schedules.
Dr. Tenpenny warned about the dangers of the current vaccination schedule while attending the world premier of The Great Awakening documentary in June 2023.
“If a child gets all of the vaccines in the entire schedule, they get almost 13,000 micrograms of aluminum, and they get almost 600 micrograms of mercury, plus over 200 different chemicals,” she said. “So that’s why they’ve never been proven to be safe.”
The upcoming 2025 Immunization Schedule approved by the CDC now recommends 36 vaccinations for children from the time they are in their mother’s womb until they are two years old (four doses are given to the pregnant mother while 32 doses are injected in the child from birth to 24 months).
Dr. Simone Gold has called for an investigation into the current vaccination schedule.
“In the 1960’s children received 5 vaccine shots in total. Today, the CDC says that children should receive 72 vaccine shots, a majority of them before the age of 6. The CDC is known for corruptly advancing Big Pharma interests. This schedule needs to be investigated further,” she said on X in September.
The CDC currently advises children to receive 70 doses before they turn 18. This is a massive increase from the 1980s, when they received 24 doses. Many medical freedom activists blame the explosion in shots on the 1986 National Childhood Vaccine Injury Act which gave vaccine makers legal protection from any harm their products inflict on those who receive them.
Doctors and medical freedom activists, including RFK Jr., have long maintained that the massive uptick in autism in recent decades is likely due to the increases in vaccines for children.
-

 Alberta1 day ago
Alberta1 day agoProposed $70 billion AI data centre in MD of Greenview could launch an incredible new chapter for western Canadian energy
-
 Brownstone Institute4 hours ago
Brownstone Institute4 hours agoA Potpourri of the World’s Unexposed Scandals
-

 Alberta1 day ago
Alberta1 day agoYour towing rights! AMA unveils measures to help fight predatory towing
-

 Economy2 hours ago
Economy2 hours agoThe White Pill: Big Government Can Be Defeated (Just Ask the Soviet Union)
-

 conflict1 hour ago
conflict1 hour agoTrump has started negotiations to end the war in Ukraine
-

 COVID-1912 mins ago
COVID-1912 mins agoEsteemed UK Doctor pleads with governments to cancel COVID-19 vaccines
-

 COVID-195 hours ago
COVID-195 hours agoBiden HHS extends immunity for COVID shot manufacturers through 2029
-

 Bruce Dowbiggin3 hours ago
Bruce Dowbiggin3 hours agoMLB’s Exploding Chequebook: Parity Is Now For Suckers




