Health
Robert F. Kennedy, Jr. Urges ‘Make America Healthy Again’

From Heartland Daily News
Despite dropping out of the race for president in August, Robert F. Kennedy, Jr. is turning up the volume on reforming national health care and drug policy and attracting attention to what role he might play in an administration depending on the outcome of the November election.
Kennedy has endorsed former president Donald Trump, and Trump has hinted that there could be a role in his second Trump administration.
Kennedy, who founded the safety advocacy group Children’s Health Defense, recently revealed the scope of his health care recommendations through his “Make America Healthy Again” agenda. Trump named Kennedy to his transition team and pledged to establish a panel of experts to work with Kennedy to investigate the increase of chronic health problems and childhood diseases in the United States (see related articles, pages 8,9).
In a September 5 op-ed in The Wall Street Journal, Kennedy laid out his 12-point Make America Healthy Again plan. Some of the ideas include reducing conflicts of interest at federal health agencies, implementing drug price caps, setting chemical and pesticide standards, requiring nutrition classes in medical school, redirecting money toward preventative care, rereleasing a presidential fitness standard, and expanding health savings accounts.
Boundary Crossing
Over the years, Kennedy has not hesitated to express his opinions, many of which have challenged long-held positions of the public health establishment on issues from vaccines and childhood obesity to the role of big pharmaceutical companies.
Kennedy’s stances cross ideological boundaries. His support of a single-payer national health care system conflicts with free-market opinions on the right, and his criticism of big-government bullying alienates the left. The nation’s painful experience with the measures taken to stem the spread of COVID-19 has attracted attention to Kennedy’s health care opinions in the wake of his forceful criticisms of those policies.
In a wide-ranging interview with Preferred Health magazine in June, Kennedy lambasted the lockdowns and the people he says profited from them.
“The people who came into the pandemic with a billion dollars, the Bill Gates, the Mark Zuckerbergs, the Bloombergs, the Jeffery Bezos, increased their wealth on average by 30 percent,” Kennedy told the publication.
“The lockdowns were a gift to them, the super-rich,” said Kennedy. “Jeffery Bezos, the richest or second-richest man in the world, was able to close down all of his competitors, 3.3 million businesses, and then give us a two-year training course about how to never use a retail outlet again in our lives. Forty-one percent of the black-owned businesses will never reopen. And he was instrumental because he was censoring the books that were critical of the lockdowns, including one that I wrote.”
Insider Advantage
Kennedy’s criticisms appeal to Craig Rucker, president of the Committee for a Constructive Tomorrow (CFACT).
“Kennedy, by virtue of his family name, is an insider, but his unorthodox views make him a provocative outsider,” said Rucker. “The public-health establishment, against which he has railed for years, failed miserably during the coronavirus pandemic. The ties between HHS and Big Pharma are far too cozy, and we have good reason to believe public health suffers as a consequence. A free spirit like his could be just what the doctor ordered.”
NIH Reform Call
Echoing his criticisms of the pandemic response, Kennedy says he wants to overhaul federal health care agencies, beginning with the National Institutes of Health (NIH).
The NIH suppressed the use of ivermectin and hydroxychloroquine during the early stages of the pandemic, in favor of, first, remdesivir and later the COVID vaccines through emergency use authorization, Kennedy argues. Saying the NIH “has been transformed into an incubator for the pharmaceutical industry,” Kennedy recommends removing much of the NIH’s funding for virology.
“It has stepped away from rigorous, evidence-based science, evidence-based medicine, into kind of a magical world,” Kennedy told Preferred Health. “It needs to have scientific discipline reimposed on the entire field of virology. We ought to be funding the study of the etiology of chronic diseases in our universities.”
Focus Shift
Kennedy has also spoken widely on chronic childhood diseases, some of which he has attributed to vaccines. Kennedy has called for public health authorities to shift their focus from infectious diseases such as COVID and influenza to devote more attention to diabetes, obesity, environmental toxins, and other longer-term concerns.
Kennedy has also cited large-scale factory farming and processed food as contributing to the nation’s health problems.
Peter Pitts, president and co-founder of the Center for Medicine in the Public Interest, says Kennedy brings a fresh perspective to public health debates.
“RFK Jr.’s penchant for not taking things at face value could go a long way toward forcing government public-health agencies to argue on behalf of their beliefs rather than simply relying on a ‘because I said so’ defense,” said Pitts.
Surprising Endorsements
Texas Agriculture Commissioner Sid Miller, a Republican, praised Kennedy’s efforts in a September 26 op-ed for Fox News.
“The role of Big Food, much like Big Pharma, is to prioritize their profits over our health,” wrote Miller. “I enthusiastically support RFK Jr.’s campaign to hold these industries accountable by reforming our food and medicine approval and patenting systems. In this he is uniquely qualified: the $1.7 trillion pharmaceutical industry has unfairly maligned him for decades, and he’s still standing strong.”
In a move that raised eyebrows, Robert Redfield, who headed the Centers for Disease Control and Prevention (CDC) under Trump from 2018 to 2021, endorsed Kennedy’s reform efforts in a Newsweek op-ed in September.
“If the next president prioritizes the National Institutes of Health (NIH) to identify which exposures are contributing to the spike in chronic disease in children, we will finally find out and end what is slowly destroying our children,” wrote Redfield.
Bonner Russell Cohen, Ph.D., ([email protected]) is a senior fellow at the National Center for Public Policy Research.
Health
The Data That Doesn’t Exist

ACIP voted to un-recommend the Hep B birth dose, but here’s the problem: they still can’t weigh the other side of the ledger
Sunday, something happened that has never happened in the history of American public health: ACIP voted 8-3 to un-recommend the universal birth dose of hepatitis B for babies born to mothers who test negative for the virus. After 34 years of jabbing every American newborn within hours of taking their first breath—regardless of whether their mother had hepatitis B—the committee finally acknowledged what 25 European countries figured out decades ago: it doesn’t make sense.
But watching this vote unfold, I couldn’t help but notice the absurdity of the debate itself. Committee members who opposed the change kept saying variations of the same thing: “We’ve heard ‘do no harm’ as a moral imperative. We are doing harm by changing this wording.” Another said “no rational science has been presented” to support the change.
How to End the Autism Epidemic is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
And therein lies the fundamental problem with ACIP—and with the entire vaccine regulatory apparatus in America. They literally cannot weigh risk versus benefit because they only have data on one side of the scale.
The Missing Side of the Ledger
When ACIP debates adding or removing a vaccine from the schedule, they can produce endless data on disease incidence. They can show you charts demonstrating how hepatitis B cases in infants dropped from thousands to single digits after 1991. They can model projected infections if vaccination rates decline. They have this data at their fingertips because tracking infectious disease is something our public health apparatus actually does.
But ask them to produce equivalent data on vaccine injury, and you’ll get silence. Not “the data shows injuries are rare.” Not “here’s our comprehensive tracking of adverse events.” Just… nothing. A void where information should be.
This is not an accident. This is by design.
The safety trials for Engerix-B and Recombivax HB—the two hepatitis B vaccines given to American newborns—monitored adverse events for four to five days after injection. That’s it. If your baby developed seizures on day six, or regressed into autism over the following months, or developed autoimmune disease in the following year—none of that would appear in the pre-licensure safety data.
And the post-market surveillance? VAERS is a voluntary reporting system that the CDC itself acknowledges captures only a tiny fraction of adverse events. A Harvard-funded study found it captures perhaps 1% of actual vaccine injuries. Vaccine court has paid out over $5 billion in claims while simultaneously being structured to make filing nearly impossible for average families.
So when Dr. Cody Meissner voted against removing the Hep B birth dose and said he saw “clear evidence of the benefits” but “not the harms,” he was accidentally revealing the entire rotten structure. Of course he doesn’t see the harms. Nobody is systematically looking for them.
The Invisibility of Vaccine Injury
Here’s what most people don’t understand about vaccine injury: it’s nothing like a gunshot wound.
If you shoot someone, the cause is obvious. There’s a bullet, a wound, blood, a clear mechanism of action visible to any observer. Even a medical examiner who’s never seen the victim before can determine cause of death.
Vaccine injury doesn’t work that way. When aluminum nanoparticles from a vaccine cross the blood-brain barrier via macrophages, when they lodge in brain tissue and trigger chronic neuroinflammation, when a child slowly regresses over weeks or months—there’s no bullet. There’s no smoking gun. There’s just a before and an after, and a desperate parent trying to explain to doctors that something changed.
This invisibility is the vaccine program’s greatest protection. Because the injury mechanism is complex and delayed, because it doesn’t leave an obvious wound, because it requires actually looking to find—and because no one in authority is looking—the injuries simply don’t exist in the official record.
I watched my own son Jamie regress after his vaccines. A healthy, developing toddler who lost his words, stopped making eye contact, and retreated into a world we couldn’t reach. My wife and I know what happened. Thousands of other parents know the same thing happened to their children. But because this type of injury doesn’t show up on a simple blood test, because there’s no autopsy finding that says “vaccine-induced encephalopathy,” ACIP members can sit in a room and say with straight faces that they don’t see evidence of harm.
They’re not lying. They literally can’t see it. Because no one is measuring it.
The Chicken Pox Conundrum
Here’s an example that illustrates the insanity of our current approach.
The varicella (chicken pox) vaccine was added to the schedule in 1995. It definitely reduces chicken pox cases. The data is clear on that front. Mission accomplished, right?
But what about the other side of the ledger?
Emerging research suggests that wild chicken pox infection provides some protective effect against brain cancers—particularly glioma, the most common type of primary brain tumor. Multiple studies have found that people who had chicken pox as children have significantly lower rates of brain cancer later in life. The hypothesis is that the immune response to wild varicella provides lasting immunological benefits that extend far beyond preventing itchy spots.
Meanwhile, the vaccine itself has been associated with increased rates of autoimmune conditions. Studies have linked varicella vaccination to higher rates of herpes zoster (shingles) outbreaks in younger age groups, to autoimmune disorders, to various adverse events that weren’t captured in the original short-term safety trials.
So what’s the true risk-benefit of the chicken pox vaccine? Does preventing a week of itchy discomfort in childhood justify potentially increased rates of brain cancer and autoimmune disease later in life?
ACIP can’t answer this question. They literally don’t have the data. They can show you chicken pox cases going down. They cannot show you a comprehensive analysis of long-term neurological and immunological outcomes in vaccinated versus unvaccinated populations, because that study has never been done.
And so they keep recommending the vaccine based on the only data they have—the disease prevention data—while remaining willfully blind to consequences they’ve never bothered to measure.
The ACIP Paradox
Sunday’s vote was historic, but it also revealed the fundamental paradox of vaccine regulation in America.
The committee members who voted to remove the universal Hep B birth dose recommendation did so largely based on comparative evidence from Europe, parental concerns, and the basic logic that vaccinating a 12-hour-old baby for a sexually transmitted disease their mother doesn’t have makes no medical sense. They were right to do so.
But the committee members who voted against the change weren’t wrong either, from their perspective. They looked at the only data they have—disease prevention data—and concluded that removing the recommendation could lead to more hepatitis B cases. And within their limited framework, they’re correct.
The problem is the framework itself.
True risk-benefit analysis requires data on both risks AND benefits. ACIP has comprehensive data on benefits (disease prevention) and virtually no data on risks (vaccine injury). So every decision they make is fundamentally flawed from the start.
When Dr. Joseph Hibbeln complained that “no rational science has been presented” to support changing the recommendations, he was inadvertently indicting the entire system. Of course no comprehensive vaccine injury data was presented—such data doesn’t exist because no one has been willing to collect it.
This is like asking someone to make an informed financial decision while only showing them potential profits and hiding all possible losses. Of course the decision will be skewed. Of course you’ll end up with a bloated portfolio of high-risk investments that look great on paper.
The Real Reform
If RFK Jr. and the new HHS leadership want to actually fix the vaccine program, they need to understand that removing individual vaccines or making them “optional” is just rearranging deck chairs on the Titanic.
The real reform is creating the data infrastructure that should have existed from the beginning.
We need a comprehensive, long-term, vaccinated-versus-unvaccinated health outcomes study. Not a five-day safety trial. A multi-decade tracking of neurological, immunological, and developmental outcomes across populations with varying vaccination status. Florida just eliminated all vaccine mandates—that state alone could provide the data we need within ten years if someone had the courage to actually collect it.
We need a vaccine injury surveillance system that actually captures adverse events. Not a voluntary reporting system that misses 99% of injuries. An active surveillance system with trained clinicians looking for the kinds of delayed, complex injuries that vaccines actually cause.
We need accountability for manufacturers. The 1986 National Childhood Vaccine Injury Act removed all liability from vaccine makers—and predictably, the vaccine schedule exploded afterward while safety research stagnated. Why would any company invest in safety when they can’t be sued for injuries?
Without this data, every ACIP meeting will be the same performance we watched this week: members confidently citing disease prevention data while admitting they can’t see evidence of harm—not because harm doesn’t exist, but because no one is looking for it.
What Comes Next
Sunday’s vote was a crack in the wall. For the first time, an American regulatory body acknowledged that perhaps vaccinating every newborn within hours of birth for a disease primarily transmitted through sex and IV drug use doesn’t make sense when the mother has already tested negative.
But the forces of institutional inertia are already mobilizing. The American Academy of Pediatrics is “disappointed.” The American Medical Association is calling for the CDC to reject the recommendation. The pharmaceutical industry—which collects over $225 million annually from Hep B birth doses alone—will fight to restore the universal recommendation.
They will cite the same data they always cite: disease prevention data. Cases prevented. Infections avoided. Lives saved—theoretically.
They will not cite vaccine injury data, because that data doesn’t exist in any comprehensive form. They will not present long-term health outcomes in vaccinated versus unvaccinated children, because those studies have been actively avoided for decades. They will not acknowledge the thousands of families who have watched their children regress after vaccination, because those injuries aren’t captured in any official database.
And this is why ACIP will always be hamstrung. Until we build the data infrastructure to actually measure vaccine injury—to put real numbers on the other side of the ledger—every vaccine decision will be based on incomplete information. Every “risk-benefit analysis” will be a fraud, because we’re only measuring half the equation.
The hepatitis B birth dose vote was a small victory. But the larger battle—for actual science, for complete data, for true informed consent—that battle is just beginning.
And until we win it, ACIP will continue making decisions in the dark, confidently citing evidence of benefits while remaining deliberately blind to the harms they’ve never bothered to measure.
About the author
J.B. Handley is the proud father of a child with Autism. He spent his career in the private equity industry and received his undergraduate degree with honors from Stanford University. His first book, How to End the Autism Epidemic, was published in September 2018. The book has sold more than 75,000 copies, was an NPD Bookscan and Publisher’s Weekly Bestseller, broke the Top 40 on Amazon, and has more than 1,000 Five-star reviews. Mr. Handley and his nonspeaking son are also the authors of Underestimated: An Autism Miracle and co-produced the film SPELLERS, available now on YouTube.
How to End the Autism Epidemic is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Focal Points
Common Vaccines Linked to 38-50% Increased Risk of Dementia and Alzheimer’s
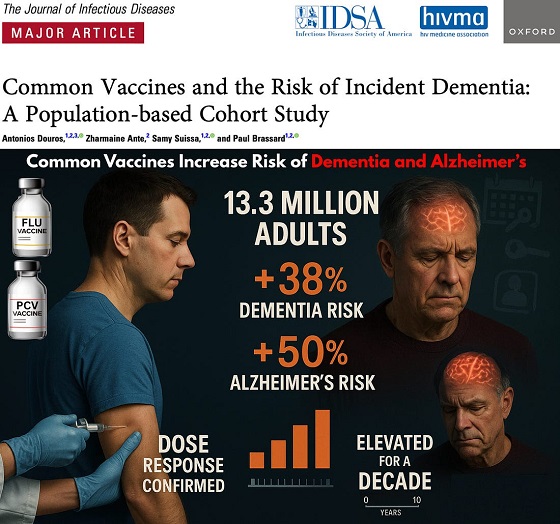
The single largest vaccine–dementia study ever conducted (n=13.3 million) finds risk intensifies with more doses, remains elevated for a full decade, and is strongest after flu and pneumococcal shots.
The single largest and most rigorous study ever conducted on vaccines and dementia — spanning 13.3 million UK adults — has uncovered a deeply troubling pattern: those who received common adult vaccines faced a significantly higher risk of both dementia and Alzheimer’s disease.
The risk intensifies with more doses, remains elevated for a full decade, and is strongest after influenza and pneumococcal vaccination. With each layer of statistical adjustment, the signal doesn’t fade — it becomes sharper, more consistent, and increasingly difficult to explain away.
And critically, these associations persisted even after adjusting for an unusually wide range of potential confounders, including age, sex, socioeconomic status, BMI, smoking, alcohol-related disorders, hypertension, atrial fibrillation, heart failure, coronary artery disease, stroke/TIA, peripheral vascular disease, diabetes, chronic kidney and liver disease, depression, epilepsy, Parkinson’s disease, cancer, traumatic brain injury, hypothyroidism, osteoporosis, and dozens of medications ranging from NSAIDs and opioids to statins, antiplatelets, immunosuppressants, and antidepressants.
Even after controlling for this extensive list, the elevated risks remained strong and remarkably stable.
Vaccinated Adults Had a 38% Higher Risk of Dementia
The primary adjusted model showed that adults receiving common adult vaccines (influenza, pneumococcal, shingles, tetanus, diphtheria, pertussis) had a:
38% increased risk of developing dementia (OR 1.38)
This alone dismantles the narrative of “vaccines protect the brain,” but the deeper findings are far worse.
Alzheimer’s Disease Risk Is Even Higher — 50% Increased Risk
Buried in the supplemental tables is a more shocking result: when the authors restricted analyses to Alzheimer’s disease specifically, the association grew even stronger.
50% increased risk of Alzheimer’s (Adjusted OR 1.50)
This indicates the effect is not random. The association intensifies for the most devastating subtype of dementia.
Clear Dose–Response Pattern: More Vaccines = Higher Risk
The authors ran multiple dose–response models, and every one of them shows the same pattern:
Dementia (all types)
From eTable 2:
- 1 vaccine dose → Adjusted OR 1.26 (26% higher risk)
- 2–3 doses → Adjusted OR 1.32 (32% higher risk)
- 4–7 doses → Adjusted OR 1.42 (42% higher risk)
- 8–12 doses → Adjusted OR 1.50 (50% higher risk)
- ≥13 doses → Adjusted OR 1.55 (55% higher risk)
Alzheimer’s Disease (AD) Shows the Same—and Even Stronger—Trend
From eTable 7:
- 1 dose → Adjusted OR 1.32 (32% higher risk)
- 2–3 doses → Adjusted OR 1.41 (41% higher risk)
- ≥4 doses → Adjusted OR 1.61 (61% higher risk)
This is one of the most powerful and unmistakable signals in epidemiology.
Time–Response Curve: Risk Peaks Soon After Vaccination and Remains Elevated for Years
Another signal strongly inconsistent with mere bias: a time-response relationship.
The highest dementia risk occurs 2–4.9 years after vaccination (Adjusted OR 1.56). The risk then slowly attenuates but never returns to baseline, remaining elevated across all time windows.
After 12.5 years, the risk is still meaningfully elevated (Adjusted OR 1.28) — a persistence incompatible with short-term “detection bias” and suggestive of a long-lasting biological impact.
This pattern is what you expect from a biological trigger with long-latency neuroinflammatory or neurodegenerative consequences.
Even After a 10-Year Lag, the Increased Risk Does Not Disappear
When the authors apply a long 10-year lag — meant to eliminate early detection bias — the elevated risk persists:
- Dementia: OR 1.20
- Alzheimer’s: OR 1.26
If this were simply “people who see doctors more often get diagnosed earlier,” the association should disappear under long lag correction.
Influenza and Pneumococcal Vaccines Drive the Signal
Two vaccines show particularly strong associations:
Influenza vaccine
- Dementia: OR 1.39 → 39% higher risk
- Alzheimer’s: OR 1.49 → 49% higher risk
Pneumococcal vaccine
- Dementia: OR 1.12 → 12% higher risk
- Alzheimer’s: OR 1.15 → 15% higher risk
And again, both exhibit dose–response escalation — the hallmark pattern of a genuine exposure–outcome relationship.
Taken together, the findings across primary, supplemental, dose–response, time–response, stratified, and sensitivity analyses paint the same picture:
• A consistent association between cumulative vaccination and increased dementia risk
• A stronger association for Alzheimer’s than for general dementia
• A dose–response effect — more vaccines, higher risk
• A time–response effect — risk peaks after exposure and persists long-term
• Influenza and pneumococcal vaccines strongly drive the signal
• The association remains after 10-year lag correction and active comparator controls
This is what a robust epidemiologic signal looks like.
In the largest single study ever conducted on vaccines and dementia, common adult vaccinations were associated with a 38% higher risk of dementia and a 50% higher risk of Alzheimer’s disease. The risk increases with more doses, persists for a decade, and is strongest for influenza and pneumococcal vaccines.
Epidemiologist and Foundation Administrator, McCullough Foundation
Support our mission: mcculloughfnd.org
Please consider following both the McCullough Foundation and my personal account on X (formerly Twitter) for further content.
FOCAL POINTS (Courageous Discourse) is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
-

 COVID-192 days ago
COVID-192 days agoTrump DOJ seeks to quash Pfizer whistleblower’s lawsuit over COVID shots
-

 Alberta2 days ago
Alberta2 days agoAlberta introducing three “all-season resort areas” to provide more summer activities in Alberta’s mountain parks
-

 Agriculture2 days ago
Agriculture2 days agoGrowing Alberta’s fresh food future
-

 International2 days ago
International2 days agoTrump admin wants to help Canadian woman rethink euthanasia, Glenn Beck says
-

 Alberta2 days ago
Alberta2 days agoThe case for expanding Canada’s energy exports
-
 Censorship Industrial Complex1 day ago
Censorship Industrial Complex1 day agoOttawa’s New Hate Law Goes Too Far
-

 Business1 day ago
Business1 day agoFuelled by federalism—America’s economically freest states come out on top
-

 Automotive1 day ago
Automotive1 day agoPoliticians should be honest about environmental pros and cons of electric vehicles










