Brownstone Institute
Big Pharma’s Rap Sheet

From the Brownstone Institute
By
It was one of those conversations you never forget. We were discussing – of all things – the Covid injections, and I was questioning the early ‘safe and effective’ claims put forward by the pharmaceutical industry. I felt suspicious of how quickly we had arrived at that point of seeming consensus despite a lack of long-term safety data. I do not trust the pharmaceutical industry. My colleague did not agree, and I felt my eyes widen as he said, “I don’t think they would do anything dodgy.” Clearly, my colleague had not read the medical history books. This conversation slapped me out of my own ignorance that Big Pharma’s rap sheet was well-known in the profession. It isn’t.
With this in mind, let’s take a look at the history of illegal and fraudulent dealings by players in the pharmaceutical industry; an industry that has way more power and influence than we give them credit for.
Before I continue, a word (not from our sponsor). There are many people working in this industry who have good intentions towards improving healthcare for patients, dedicating their lives to finding a cure or treatment for disease. Some therapeutic pharmaceuticals are truly life-saving. I probably wouldn’t be here today were it not for a couple of life-saving drugs (that’s a story for another time). But we must be very clear in our understanding. The pharmaceutical industry, as a whole and by its nature, is conflicted and significantly driven by the mighty dollar, rather than altruism.
There are many players and different games being played by the industry. We ignore these at our peril. The rap sheet of illegal activities is alarming. It seems that barely a month goes by without some pharmaceutical company in court, somewhere. Criminal convictions are common and fines tally into the billions. Civil cases, with their million-dollar settlements, are abundant too.
A 2020 peer-reviewed article published in the Journal of the American Medical Association outlines the extent of the problem. The group studied both the type of illegal activity and financial penalties imposed on pharma companies between the years 2003 and 2016. Of the companies studied, 85 percent (22 of 26) had received financial penalties for illegal activities with a total combined dollar value of $33 billion. The illegal activities included manufacturing and distributing adulterated drugs, misleading marketing, failure to disclose negative information about a product (i.e. significant side effects including death), bribery to foreign officials, fraudulently delaying market entry of competitors, pricing and financial violations, and kickbacks.
When expressed as a percentage of revenue, the highest penalties were awarded to Schering-Plough, GlaxoSmithKline (GSK), Allergan, and Wyeth. The biggest overall fines have been paid by GSK (almost $10 billion), Pfizer ($2.9 billion), Johnson & Johnson ($2.6 billion), and other familiar names including AstraZeneca, Novartis, Merck, Eli Lilly, Schering-Plough, Sanofi Aventis, and Wyeth. It’s quite a list, and many of the Big Pharma players are repeat offenders.
Prosecuting these companies is no mean feat. Cases often drag for years, making the avenue of justice and resolution inaccessible to all but the well-funded, persistent, and steadfast. If a case is won, pharma’s usual response is to appeal to a higher court and start the process again. One thing is clear; taking these giants to court requires nerves of steel, a willingness to surrender years of life to the task, and very deep pockets.
For every conviction, there are countless settlements, the company agreeing to pay out, but making no admission of guilt. A notable example is the S35 million settlement made, after 15 years of legal maneuvering, by Pfizer in a Nigerian case that alleged the company had experimented on 200 children without their parent’s knowledge or consent.
Reading through the case reports, the pattern of behavior is reminiscent of the movie Groundhog Day with the same games being played by different companies as if they are following some kind of unwritten playbook.
Occasionally there is a case that lifts the lid on these playbook strategies, revealing the influence of the pharma industry and the lengths they are willing to go to, to turn a profit. The Australian Federal Court case Peterson v Merck Sharpe and Dohme, involving the manufacturer of the drug Vioxx, is a perfect example.
By way of background, Vioxx (the anti-arthritis drug Rofecoxib) was alleged to have caused an increased risk of cardiovascular conditions including heart attack and stroke. It was launched in 1999 and, at peak popularity, was used by up to 80 million people worldwide, marketed as a safer alternative to traditional anti-inflammatory drugs with their troublesome gastrointestinal side effects.
In Peterson v Merck Sharpe and Dohme, the applicant – Graeme Robert Peterson – alleged the drug had caused the heart attack he suffered in 2003, leaving him significantly incapacitated. Peterson argued that the Merck companies were negligent in not having withdrawn the drug from the market earlier than they did in 2004 and, by not warning of the risks and making promotional representations to doctors, were guilty of misleading and deceptive conduct under the Commonwealth Trade Practices Act 1974.
In November 2004 Dr David Graham, then Associate Director for Science and Medicine in FDA’s Office of Drug Safety provided powerful testimony to the US Senate regarding Vioxx. According to Graham, prior to the approval of the drug, a Merck-funded study showed a seven-fold increase in heart attacks. Despite this, the drug was approved by regulatory agencies, including the FDA and the TGA.
This finding was later supported by another Merck-funded study, VIGOR – which showed a five-fold increase, the results of which were published in the high-impact New England Journal of Medicine. It was later revealed by subpoena during litigation that three heart attacks were not included in the original data submitted to the journal, a fact that at least two of the authors knew at the time. This resulted in a ‘misleading conclusion’ regarding the risk of heart attack associated with the drug.
By the time Peterson v Merck Sharpe and Dohme, an associated class action involving 1,660 people, was heard in Australia in 2009, the international parent of MSD, Merck, had already paid $4.83 billion to settle thousands of lawsuits in the US over adverse effects of Vioxx. Predictably, Merck made no admission of guilt. The Australian legal battle was a long, drawn-out affair, taking several years with more twists and turns than a cheap garden hose (you can read more about it here and here).
Long story short, a March 2010 Federal Court finding in favor of Peterson was later overturned by a full bench of the Federal Court in Oct 2011. In 2013, a settlement was reached with class action participants which resulted in a mere maximum payment of $4,629.36 per claimant. MSD generously waived their claim for legal costs against Peterson.
What’s notable in this battle was the headline-grabbing courtroom evidence detailing the extent of alleged pharmaceutical misdeeds in marketing the drug. The pharma giant went to the lengths of producing sponsored journals with renowned scientific publisher Elsevier, including a publication called The Australasian Journal of Bone and Joint Medicine. These fake ‘journals’ were made to look like independent scientific journals, but contained articles attributed to doctors that were ghostwritten by Merck employees. Some doctors listed as honorary Journal board members said they had no idea they were listed in the journal and had never been given any articles to review.
But wait, there’s more.
The trove of internal emails presented in evidence revealed a more sinister level of operation. One of the emails circulated at the pharma giant’s US headquarters contained a list of ‘problem physicians’ that the company sought to ‘neutralize’ or ‘discredit.’ The recommendations to achieve these ends included payment for presentations, research and education, financial support of private practice, and ‘strong recommendation(s) to discredit.’ Such was the extent of intimidation, that one professor wrote to the head of Merck to complain about the treatment of some of his researchers critical of the drug. The court heard how Merck had been ‘systematically playing down the side effects of Vioxx’ and their behavior ‘seriously impinge(d) on academic freedom.’
This alleged systematic intimidation was as extensive as it was effective. Result? Merck made over $2 billion per year in sales before Vioxx was finally pulled from pharmacy shelves in 2004. In his testimony, Dr Graham estimated that between 88,000 and 139,000 excess cases of heart attack or sudden cardiac death were caused by Vioxx in the US alone before it was withdrawn.
These systems of influence, manipulation, and tactics were largely operative when Covid arrived. Add to that the ‘warp speed’ development of novel ‘vaccines,’ government green lights, pharmaceutical indemnity, and confidential contracts. Now you have the makings of a pharmaceutical payday the likes of which we have never seen before.
It should come as no surprise then, the recent announcement that five US states – Texas, Kansas, Mississippi, Louisiana, and Utah – are taking Pfizer to court for withholding information, and misleading and deceiving the public through statements made in marketing its Covid-19 injection. That these cases are filed as civil suits under consumer protection laws is likely just the tip of the pharmaceutical playbook iceberg. No doubt the discovery process will hold further lessons for us all.
Brownstone Institute
The Unmasking of Vaccine Science

From the Brownstone Institute
By
I recently purchased Aaron Siri’s new book Vaccines, Amen. As I flipped though the pages, I noticed a section devoted to his now-famous deposition of Dr Stanley Plotkin, the “godfather” of vaccines.
I’d seen viral clips circulating on social media, but I had never taken the time to read the full transcript — until now.
Siri’s interrogation was methodical and unflinching…a masterclass in extracting uncomfortable truths.
A Legal Showdown
In January 2018, Dr Stanley Plotkin, a towering figure in immunology and co-developer of the rubella vaccine, was deposed under oath in Pennsylvania by attorney Aaron Siri.
The case stemmed from a custody dispute in Michigan, where divorced parents disagreed over whether their daughter should be vaccinated. Plotkin had agreed to testify in support of vaccination on behalf of the father.
What followed over the next nine hours, captured in a 400-page transcript, was extraordinary.
Plotkin’s testimony revealed ethical blind spots, scientific hubris, and a troubling indifference to vaccine safety data.
He mocked religious objectors, defended experiments on mentally disabled children, and dismissed glaring weaknesses in vaccine surveillance systems.
A System Built on Conflicts
From the outset, Plotkin admitted to a web of industry entanglements.
He confirmed receiving payments from Merck, Sanofi, GSK, Pfizer, and several biotech firms. These were not occasional consultancies but long-standing financial relationships with the very manufacturers of the vaccines he promoted.
Plotkin appeared taken aback when Siri questioned his financial windfall from royalties on products like RotaTeq, and expressed surprise at the “tone” of the deposition.
Siri pressed on: “You didn’t anticipate that your financial dealings with those companies would be relevant?”
Plotkin replied: “I guess, no, I did not perceive that that was relevant to my opinion as to whether a child should receive vaccines.”
The man entrusted with shaping national vaccine policy had a direct financial stake in its expansion, yet he brushed it aside as irrelevant.
Contempt for Religious Dissent
Siri questioned Plotkin on his past statements, including one in which he described vaccine critics as “religious zealots who believe that the will of God includes death and disease.”
Siri asked whether he stood by that statement. Plotkin replied emphatically, “I absolutely do.”
Plotkin was not interested in ethical pluralism or accommodating divergent moral frameworks. For him, public health was a war, and religious objectors were the enemy.
He also admitted to using human foetal cells in vaccine production — specifically WI-38, a cell line derived from an aborted foetus at three months’ gestation.
Siri asked if Plotkin had authored papers involving dozens of abortions for tissue collection. Plotkin shrugged: “I don’t remember the exact number…but quite a few.”
Plotkin regarded this as a scientific necessity, though for many people — including Catholics and Orthodox Jews — it remains a profound moral concern.
Rather than acknowledging such sensitivities, Plotkin dismissed them outright, rejecting the idea that faith-based values should influence public health policy.
That kind of absolutism, where scientific aims override moral boundaries, has since drawn criticism from ethicists and public health leaders alike.
As NIH director Jay Bhattacharya later observed during his 2025 Senate confirmation hearing, such absolutism erodes trust.
“In public health, we need to make sure the products of science are ethically acceptable to everybody,” he said. “Having alternatives that are not ethically conflicted with foetal cell lines is not just an ethical issue — it’s a public health issue.”
Safety Assumed, Not Proven
When the discussion turned to safety, Siri asked, “Are you aware of any study that compares vaccinated children to completely unvaccinated children?”
Plotkin replied that he was “not aware of well-controlled studies.”
Asked why no placebo-controlled trials had been conducted on routine childhood vaccines such as hepatitis B, Plotkin said such trials would be “ethically difficult.”
That rationale, Siri noted, creates a scientific blind spot. If trials are deemed too unethical to conduct, then gold-standard safety data — the kind required for other pharmaceuticals — simply do not exist for the full childhood vaccine schedule.
Siri pointed to one example: Merck’s hepatitis B vaccine, administered to newborns. The company had only monitored participants for adverse events for five days after injection.
Plotkin didn’t dispute it. “Five days is certainly short for follow-up,” he admitted, but claimed that “most serious events” would occur within that time frame.
Siri challenged the idea that such a narrow window could capture meaningful safety data — especially when autoimmune or neurodevelopmental effects could take weeks or months to emerge.
Siri pushed on. He asked Plotkin if the DTaP and Tdap vaccines — for diphtheria, tetanus and pertussis — could cause autism.
“I feel confident they do not,” Plotkin replied.
But when shown the Institute of Medicine’s 2011 report, which found the evidence “inadequate to accept or reject” a causal link between DTaP and autism, Plotkin countered, “Yes, but the point is that there were no studies showing that it does cause autism.”
In that moment, Plotkin embraced a fallacy: treating the absence of evidence as evidence of absence.
“You’re making assumptions, Dr Plotkin,” Siri challenged. “It would be a bit premature to make the unequivocal, sweeping statement that vaccines do not cause autism, correct?”
Plotkin relented. “As a scientist, I would say that I do not have evidence one way or the other.”
The MMR
The deposition also exposed the fragile foundations of the measles, mumps, and rubella (MMR) vaccine.
When Siri asked for evidence of randomised, placebo-controlled trials conducted before MMR’s licensing, Plotkin pushed back: “To say that it hasn’t been tested is absolute nonsense,” he said, claiming it had been studied “extensively.”
Pressed to cite a specific trial, Plotkin couldn’t name one. Instead, he gestured to his own 1,800-page textbook: “You can find them in this book, if you wish.”
Siri replied that he wanted an actual peer-reviewed study, not a reference to Plotkin’s own book. “So you’re not willing to provide them?” he asked. “You want us to just take your word for it?”
Plotkin became visibly frustrated.
Eventually, he conceded there wasn’t a single randomised, placebo-controlled trial. “I don’t remember there being a control group for the studies, I’m recalling,” he said.
The exchange foreshadowed a broader shift in public discourse, highlighting long-standing concerns that some combination vaccines were effectively grandfathered into the schedule without adequate safety testing.
In September this year, President Trump called for the MMR vaccine to be broken up into three separate injections.
The proposal echoed a view that Andrew Wakefield had voiced decades earlier — namely, that combining all three viruses into a single shot might pose greater risk than spacing them out.
Wakefield was vilified and struck from the medical register. But now, that same question — once branded as dangerous misinformation — is set to be re-examined by the CDC’s new vaccine advisory committee, chaired by Martin Kulldorff.
The Aluminium Adjuvant Blind Spot
Siri next turned to aluminium adjuvants — the immune-activating agents used in many childhood vaccines.
When asked whether studies had compared animals injected with aluminium to those given saline, Plotkin conceded that research on their safety was limited.
Siri pressed further, asking if aluminium injected into the body could travel to the brain. Plotkin replied, “I have not seen such studies, no, or not read such studies.”
When presented with a series of papers showing that aluminium can migrate to the brain, Plotkin admitted he had not studied the issue himself, acknowledging that there were experiments “suggesting that that is possible.”
Asked whether aluminium might disrupt neurological development in children, Plotkin stated, “I’m not aware that there is evidence that aluminum disrupts the developmental processes in susceptible children.”
Taken together, these exchanges revealed a striking gap in the evidence base.
Compounds such as aluminium hydroxide and aluminium phosphate have been injected into babies for decades, yet no rigorous studies have ever evaluated their neurotoxicity against an inert placebo.
This issue returned to the spotlight in September 2025, when President Trump pledged to remove aluminium from vaccines, and world-leading researcher Dr Christopher Exley renewed calls for its complete reassessment.
A Broken Safety Net
Siri then turned to the reliability of the Vaccine Adverse Event Reporting System (VAERS) — the primary mechanism for collecting reports of vaccine-related injuries in the United States.
Did Plotkin believe most adverse events were captured in this database?
“I think…probably most are reported,” he replied.
But Siri showed him a government-commissioned study by Harvard Pilgrim, which found that fewer than 1% of vaccine adverse events are reported to VAERS.
“Yes,” Plotkin said, backtracking. “I don’t really put much faith into the VAERS system…”
Yet this is the same database officials routinely cite to claim that “vaccines are safe.”
Ironically, Plotkin himself recently co-authored a provocative editorial in the New England Journal of Medicine, conceding that vaccine safety monitoring remains grossly “inadequate.”
Experimenting on the Vulnerable
Perhaps the most chilling part of the deposition concerned Plotkin’s history of human experimentation.
“Have you ever used orphans to study an experimental vaccine?” Siri asked.
“Yes,” Plotkin replied.
“Have you ever used the mentally handicapped to study an experimental vaccine?” Siri asked.
“I don’t recollect…I wouldn’t deny that I may have done so,” Plotkin replied.
Siri cited a study conducted by Plotkin in which he had administered experimental rubella vaccines to institutionalised children who were “mentally retarded.”
Plotkin stated flippantly, “Okay well, in that case…that’s what I did.”
There was no apology, no sign of ethical reflection — just matter-of-fact acceptance.
Siri wasn’t done.
He asked if Plotkin had argued that it was better to test on those “who are human in form but not in social potential” rather than on healthy children.
Plotkin admitted to writing it.
Siri established that Plotkin had also conducted vaccine research on the babies of imprisoned mothers, and on colonised African populations.
Plotkin appeared to suggest that the scientific value of such studies outweighed the ethical lapses—an attitude that many would interpret as the classic ‘ends justify the means’ rationale.
But that logic fails the most basic test of informed consent. Siri asked whether consent had been obtained in these cases.
“I don’t remember…but I assume it was,” Plotkin said.
Assume?
This was post-Nuremberg research. And the leading vaccine developer in America couldn’t say for sure whether he had properly informed the people he experimented on.
In any other field of medicine, such lapses would be disqualifying.
A Casual Dismissal of Parental Rights
Plotkin’s indifference to experimenting on disabled children didn’t stop there.
Siri asked whether someone who declined a vaccine due to concerns about missing safety data should be labelled “anti-vax.”
Plotkin replied, “If they refused to be vaccinated themselves or refused to have their children vaccinated, I would call them an anti-vaccination person, yes.”
Plotkin was less concerned about adults making that choice for themselves, but he had no tolerance for parents making those choices for their own children.
“The situation for children is quite different,” said Plotkin, “because one is making a decision for somebody else and also making a decision that has important implications for public health.”
In Plotkin’s view, the state held greater authority than parents over a child’s medical decisions — even when the science was uncertain.
The Enabling of Figures Like Plotkin
The Plotkin deposition stands as a case study in how conflicts of interest, ideology, and deference to authority have corroded the scientific foundations of public health.
Plotkin is no fringe figure. He is celebrated, honoured, and revered. Yet he promotes vaccines that have never undergone true placebo-controlled testing, shrugs off the failures of post-market surveillance, and admits to experimenting on vulnerable populations.
This is not conjecture or conspiracy — it is sworn testimony from the man who helped build the modern vaccine program.
Now, as Health Secretary Robert F. Kennedy, Jr. reopens long-dismissed questions about aluminium adjuvants and the absence of long-term safety studies, Plotkin’s once-untouchable legacy is beginning to fray.
Republished from the author’s Substack
Brownstone Institute
Bizarre Decisions about Nicotine Pouches Lead to the Wrong Products on Shelves

From the Brownstone Institute
A walk through a dozen convenience stores in Montgomery County, Pennsylvania, says a lot about how US nicotine policy actually works. Only about one in eight nicotine-pouch products for sale is legal. The rest are unauthorized—but they’re not all the same. Some are brightly branded, with uncertain ingredients, not approved by any Western regulator, and clearly aimed at impulse buyers. Others—like Sweden’s NOAT—are the opposite: muted, well-made, adult-oriented, and already approved for sale in Europe.
Yet in the United States, NOAT has been told to stop selling. In September 2025, the Food and Drug Administration (FDA) issued the company a warning letter for offering nicotine pouches without marketing authorization. That might make sense if the products were dangerous, but they appear to be among the safest on the market: mild flavors, low nicotine levels, and recyclable paper packaging. In Europe, regulators consider them acceptable. In America, they’re banned. The decision looks, at best, strange—and possibly arbitrary.
What the Market Shows
My October 2025 audit was straightforward. I visited twelve stores and recorded every distinct pouch product visible for sale at the counter. If the item matched one of the twenty ZYN products that the FDA authorized in January, it was counted as legal. Everything else was counted as illegal.
Two of the stores told me they had recently received FDA letters and had already removed most illegal stock. The other ten stores were still dominated by unauthorized products—more than 93 percent of what was on display. Across all twelve locations, about 12 percent of products were legal ZYN, and about 88 percent were not.
The illegal share wasn’t uniform. Many of the unauthorized products were clearly high-nicotine imports with flashy names like Loop, Velo, and Zimo. These products may be fine, but some are probably high in contaminants, and a few often with very high nicotine levels. Others were subdued, plainly meant for adult users. NOAT was a good example of that second group: simple packaging, oat-based filler, restrained flavoring, and branding that makes no effort to look “cool.” It’s the kind of product any regulator serious about harm reduction would welcome.
Enforcement Works
To the FDA’s credit, enforcement does make a difference. The two stores that received official letters quickly pulled their illegal stock. That mirrors the agency’s broader efforts this year: new import alerts to detain unauthorized tobacco products at the border (see also Import Alert 98-06), and hundreds of warning letters to retailers, importers, and distributors.
But effective enforcement can’t solve a supply problem. The list of legal nicotine-pouch products is still extremely short—only a narrow range of ZYN items. Adults who want more variety, or stores that want to meet that demand, inevitably turn to gray-market suppliers. The more limited the legal catalog, the more the illegal market thrives.
Why the NOAT Decision Appears Bizarre
The FDA’s own actions make the situation hard to explain. In January 2025, it authorized twenty ZYN products after finding that they contained far fewer harmful chemicals than cigarettes and could help adult smokers switch. That was progress. But nine months later, the FDA has approved nothing else—while sending a warning letter to NOAT, arguably the least youth-oriented pouch line in the world.
The outcome is bad for legal sellers and public health. ZYN is legal; a handful of clearly risky, high-nicotine imports continue to circulate; and a mild, adult-market brand that meets European safety and labeling rules is banned. Officially, NOAT’s problem is procedural—it lacks a marketing order. But in practical terms, the FDA is punishing the very design choices it claims to value: simplicity, low appeal to minors, and clean ingredients.
This approach also ignores the differences in actual risk. Studies consistently show that nicotine pouches have far fewer toxins than cigarettes and far less variability than many vapes. The biggest pouch concerns are uneven nicotine levels and occasional traces of tobacco-specific nitrosamines, depending on manufacturing quality. The serious contamination issues—heavy metals and inconsistent dosage—belong mostly to disposable vapes, particularly the flood of unregulated imports from China. Treating all “unauthorized” products as equally bad blurs those distinctions and undermines proportional enforcement.
A Better Balance: Enforce Upstream, Widen the Legal Path
My small Montgomery County survey suggests a simple formula for improvement.
First, keep enforcement targeted and focused on suppliers, not just clerks. Warning letters clearly change behavior at the store level, but the biggest impact will come from auditing distributors and importers, and stopping bad shipments before they reach retail shelves.
Second, make compliance easy. A single-page list of authorized nicotine-pouch products—currently the twenty approved ZYN items—should be posted in every store and attached to distributor invoices. Point-of-sale systems can block barcodes for anything not on the list, and retailers could affirm, once a year, that they stock only approved items.
Third, widen the legal lane. The FDA launched a pilot program in September 2025 to speed review of new pouch applications. That program should spell out exactly what evidence is needed—chemical data, toxicology, nicotine release rates, and behavioral studies—and make timely decisions. If products like NOAT meet those standards, they should be authorized quickly. Legal competition among adult-oriented brands will crowd out the sketchy imports far faster than enforcement alone.
The Bottom Line
Enforcement matters, and the data show it works—where it happens. But the legal market is too narrow to protect consumers or encourage innovation. The current regime leaves a few ZYN products as lonely legal islands in a sea of gray-market pouches that range from sensible to reckless.
The FDA’s treatment of NOAT stands out as a case study in inconsistency: a quiet, adult-focused brand approved in Europe yet effectively banned in the US, while flashier and riskier options continue to slip through. That’s not a public-health victory; it’s a missed opportunity.
If the goal is to help adult smokers move to lower-risk products while keeping youth use low, the path forward is clear: enforce smartly, make compliance easy, and give good products a fair shot. Right now, we’re doing the first part well—but failing at the second and third. It’s time to fix that.
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoWayne Gretzky’s Terrible, Awful Week.. And Soccer/ Football.
-

 espionage17 hours ago
espionage17 hours agoWestern Campuses Help Build China’s Digital Dragnet With U.S. Tax Funds, Study Warns
-
 Focal Points8 hours ago
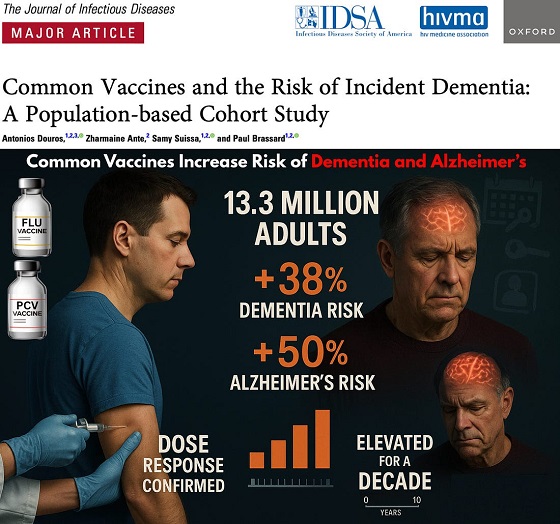
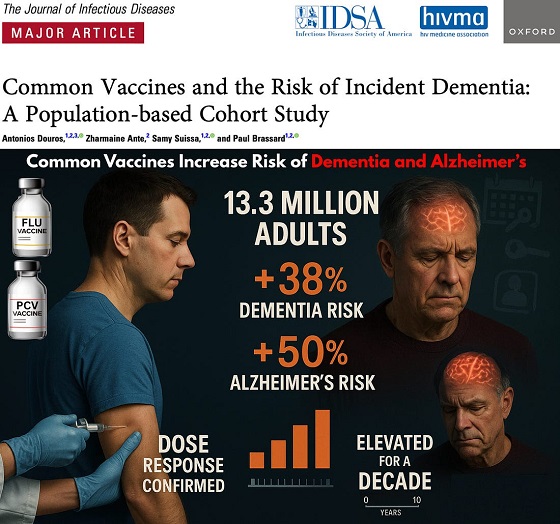
Focal Points8 hours agoCommon Vaccines Linked to 38-50% Increased Risk of Dementia and Alzheimer’s
-
 Opinion1 day ago
Opinion1 day agoThe day the ‘King of rock ‘n’ roll saved the Arizona memorial
-

 Agriculture1 day ago
Agriculture1 day agoCanada’s air quality among the best in the world
-

 Business15 hours ago
Business15 hours agoCanada invests $34 million in Chinese drones now considered to be ‘high security risks’
-

 Health6 hours ago
Health6 hours agoThe Data That Doesn’t Exist
-

 Economy16 hours ago
Economy16 hours agoAffordable housing out of reach everywhere in Canada







