Addictions
The new drug agency tasked with improving Canada’s medication practices

By Alexandra Keeler
A recent report calls on the newly-created Canada’s Drug Agency to implement a strategy to improve prescription medication practices
As Canada moves toward establishing a national drug agency, a new report has outlined recommendations for a prescription medications strategy that the agency should be tasked with implementing.
The report, released July 26 by the Canadian Drug Agency Transition Office, calls on the newly established Canada’s Drug Agency to implement a nation-wide strategy for the appropriate use of prescription medications. The transition office is a temporary government initiative responsible for developing the drug agency’s mandate and plan.
“Part of the opioid crisis has been linked to prescribing particular medications, and the dependency that people can develop with respect to certain medications,” said Stephen Samis, chair of the Appropriate Use Advisory Committee, which helped guide the development of the medications strategy outlined in the report.
“If there’s a way to help get people off of those medications in a safe and effective way, and by the use of alternatives to the medication, that’s really important,” said Samis, who formerly served as deputy health minister in the Yukon.
Canada’s Drug Agency, which was first announced by Health Minister Mark Holland in December 2023, is tasked with managing and coordinating Canada’s pharmaceutical system across the provinces and territories. It has begun establishing advisory bodies, building partnerships and conducting research.
Under Canada’s proposed pharmacare legislation, the drug agency will also be responsible for identifying the essential prescription drugs to which Canadians should have access under pharmacare.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Primary care crisis
The report proposes six guiding principles for improving Canada’s prescription and medication use practices. These include providing more personalized primary care to patients, ensuring careful oversight of prescription medications and improving coordination between health-care providers.
Currently, more than one in five Canadian adults — about 6.5 million people — lack access to primary care, according to a May 2024 study in the Canadian Medical Association Journal. Primary care refers to health care that is regular and ongoing, such as doctor check-ups or management of chronic conditions.
“The crisis in primary care right now is really one of those potential barriers to people receiving appropriate medication with a provider that they have a relationship with,” said Samis.
The lack of access to primary care can lead to problems such as inconsistent prescribing, inadequate follow-up and insufficient patient education on prescription medications, the report says.
About 1.9 million Canadian seniors use at least one prescription medication inappropriately. This costs them and the health-care system an estimated $1.4 billion in direct and indirect costs, the report says.
“Benzodiazepines, sleeping pills … even things like medications that control heartburn. If people are on them for too long, [it] can have other kinds of side effects,” said Samis.
“Same thing with opioid related medications. It’s really important that people have medications they need so that they don’t develop dependencies.”
The report also notes that fragmented information systems and poor coordination between service providers complicate medication management — resulting in duplicate prescriptions, contradictory treatment plans and gaps in care.
“What happens often is that somebody is in primary care, and their data is over here,” said Samis. “They go into long-term care, and that information doesn’t follow them. They get prescribed new things in long-term care, they go into the hospital, then the long-term care information system might not be speaking to the hospital information system.”
‘Neutral space’
Samis says he is optimistic that Canada’s Drug Agency will be able to address some of the problematic medication practices identified in the report.
Samis will co-chair a new committee responsible for assisting with the implementation of the report’s recommendations.
“We have a diverse and knowledgeable group joining our newly established Appropriate Use Advisory Committee, with the inaugural meeting to take place on September 13,” a media relations spokesperson for Canada’s Drug Agency’s told Canadian Affairs in a written statement.
Samis envisions the agency as a “neutral space” to address health-care issues and resolve conflicts between governments and health-care providers.
“This approach avoids the conflicts that often arise between jurisdictions, levels of government, or between government and [health-care] providers,” he said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Break The Needle. Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
Addictions
There’s No Such Thing as a “Safer Supply” of Drugs

By Adam Zivo
Sweden, the U.K., and Canada all experimented with providing opioids to addicts. The results were disastrous.
[This article was originally published in City Journal, a public policy magazine and website published by the Manhattan Institute for Policy Research. We encourage our readers to subscribe to them for high-quality analysis on urban issues]
Last August, Denver’s city council passed a proclamation endorsing radical “harm reduction” strategies to address the drug crisis. Among these was “safer supply,” the idea that the government should give drug users their drug of choice, for free. Safer supply is a popular idea among drug-reform activists. But other countries have already tested this experiment and seen disastrous results, including more addiction, crime, and overdose deaths. It would be foolish to follow their example.
The safer-supply movement maintains that drug-related overdoses, infections, and deaths are driven by the unpredictability of the black market, where drugs are inconsistently dosed and often adulterated with other toxic substances. With ultra-potent opioids like fentanyl, even minor dosing errors can prove fatal. Drug contaminants, which dealers use to provide a stronger high at a lower cost, can be just as deadly and potentially disfiguring.
Because of this, harm-reduction activists sometimes argue that governments should provide a free supply of unadulterated, “safe” drugs to get users to abandon the dangerous street supply. Or they say that such drugs should be sold in a controlled manner, like alcohol or cannabis—an endorsement of partial or total drug legalization.
But “safe” is a relative term: the drugs championed by these activists include pharmaceutical-grade fentanyl, hydromorphone (an opioid as potent as heroin), and prescription meth. Though less risky than their illicit alternatives, these drugs are still profoundly dangerous.
The theory behind safer supply is not entirely unreasonable, but in every country that has tried it, implementation has led to increased suffering and addiction. In Europe, only Sweden and the U.K. have tested safer supply, both in the 1960s. The Swedish model gave more than 100 addicts nearly unlimited access through their doctors to prescriptions for morphine and amphetamines, with no expectations of supervised consumption. Recipients mostly sold their free drugs on the black market, often through a network of “satellite patients” (addicts who purchased prescribed drugs). This led to an explosion of addiction and public disorder.
Most doctors quickly abandoned the experiment, and it was shut down after just two years and several high-profile overdose deaths, including that of a 17-year-old girl. Media coverage portrayed safer supply as a generational medical scandal and noted that the British, after experiencing similar problems, also abandoned their experiment.
While the U.S. has never formally adopted a safer-supply policy, it experienced something functionally similar during the OxyContin crisis of the 2000s. At the time, access to the powerful opioid was virtually unrestricted in many parts of North America. Addicts turned to pharmacies for an easy fix and often sold or traded their extra pills for a quick buck. Unscrupulous “pill mills” handed out prescriptions like candy, flooding communities with OxyContin and similar narcotics. The result was a devastating opioid epidemic—one that rages to this day, at a cumulative cost of hundreds of thousands of American lives. Canada was similarly affected.
The OxyContin crisis explains why many experienced addiction experts were aghast when Canada greatly expanded access to safer supply in 2020, following a four-year pilot project. They worried that the mistakes of the recent past were being made all over again, and that the recently vanquished pill mills had returned under the cloak of “harm reduction.”
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Most Canadian safer-supply prescribers dispense large quantities of hydromorphone with little to no supervised consumption. Patients can receive up to 40 eight-milligram pills per day—despite the fact that just two or three are enough to cause an overdose in someone without opioid tolerance. Some prescribers also provide supplementary fentanyl, oxycodone, or stimulants.
Unfortunately, many safer-supply patients sell or trade a significant portion of these drugs—primarily hydromorphone—in order to purchase more potent illicit substances, such as street fentanyl.
The problems with safer supply entered Canada’s consciousness in mid-2023, through an investigative report I wrote for the National Post. I interviewed 14 addiction physicians from across the country, who testified that safer-supply diversion is ubiquitous; that the street price of hydromorphone collapsed by up to 95 percent in communities where safer supply is available; that youth are consuming and becoming addicted to diverted safer-supply drugs; and that organized crime traffics these drugs.
Facing pushback, I interviewed former drug users, who estimated that roughly 80 percent of the safer-supply drugs flowing through their social circles was getting diverted. I documented dozens of examples of safer-supply trafficking online, representing tens of thousands of pills. I spoke with youth who had developed addictions from diverted safer supply and adults who had purchased thousands of such pills.
After months of public queries, the police department of London, Ontario—where safer supply was first piloted—revealed last summer that annual hydromorphone seizures rose over 3,000 percent between 2019 and 2023. The department later held a press conference warning that gangs clearly traffic safer supply. The police departments of two nearby midsize cities also saw their post-2019 hydromorphone seizures increase more than 1,000 percent.
The Canadian government quietly dropped its support for safer supply last year, cutting funding for many of its pilot programs. The province of British Columbia (the nexus of the harm-reduction movement) finally pulled back support last month, after a leaked presentation confirmed that safer-supply drugs are getting sold internationally and that the government is investigating 60 pharmacies for paying kickbacks to safer-supply patients. For now, all safer-supply drugs dispensed within the province must be consumed under supervision.
Harm-reduction activists have insisted that no hard evidence exists of widespread diversion of safer-supply drugs, but this is only because they refuse to study the issue. Most “studies” supporting safer supply are produced by ideologically driven activist-scholars, who tend to interview a small number of program enrollees. These activists also reject attempts to track diversion as “stigmatizing.”
The experiences of Sweden, the United Kingdom, and Canada offer a clear warning: safer supply is a reliably harmful policy. The outcomes speak for themselves—rising addiction, diversion, and little evidence of long-term benefit.
As the debate unfolds in the United States, policymakers would do well to learn from these failures. Americans should not be made to endure the consequences of a policy already discredited abroad simply because progressive leaders choose to ignore the record. The question now is whether we will repeat others’ mistakes—or chart a more responsible course.
Our content is always free –
but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
Addictions
Should fentanyl dealers face manslaughter charges for fatal overdoses?

Tyler Ginn prior to his death from a fentanyl overdose in 2021. [Photo credit: Gayle Fowlie]
By Alexandra Keeler
Police are charging more drug dealers with manslaughter in fentanyl overdose deaths. But the shift is not satisfying everyone
Four years ago, Tyler Ginn died of a fentanyl overdose at the age of 18. Tyler’s father found his son unresponsive in the bedroom of their Brooklin, Ont., home.
For Tyler’s mother, Gayle Fowlie, the pain of his loss remains raw.
“He was my kid that rode his bike to the store to buy me a chocolate bar on my birthday, you know?” she told Canadian Affairs in an interview.
Police charged Jacob Norn, the drug dealer who sold Tyler his final, fatal dose, with manslaughter. More than three years after Tyler’s death, Norn was convicted and sentenced to six years in prison.
“I don’t think you can grasp how difficult going through a trial is,” Fowlie said. “On TV, it’s a less than an hour process. But the pain of it, and going over every detail and then going over every detail again … it provides details you wish you didn’t know.”
But Fowlie is glad Norn was convicted. If anything, she would have liked him to serve a longer sentence. Lawyers have told her Norn is likely to serve only two to four years of his sentence in prison.
“My son’s never coming back [and] his whole family has a life sentence of missing him the rest of our lives,” she said. “So do I think four years is fair? No.”
Norn’s case reflects a growing trend of drug dealers being charged with manslaughter when their drug sales lead to fatal overdoses.
But this shift has not satisfied everyone. Some would like to see drug dealers face harsher or different penalties.
“If we say that it was 50 per cent Tyler’s fault for buying it and 50 per cent Jacob’s fault for selling it … then I think he should have a half-a-life sentence,” said Fowlie.
Others say the legal system’s focus on prosecuting low-level drug dealers misses the broader issues at play.
“[Police] decided, in the Jacob Norn case, they were going to go one stage back,” said Peter Thorning, who was Norn’s defence lawyer.
“What about the person who gave Jacob that substance? What about the person who supplied the substance to [that person]? There was no investigation into where it came from and who was ultimately responsible for the death of that young man.”
Manslaughter charge
At least 50,000 Canadians have died from drug overdoses since 2016. Last year, an average of 21 individuals died each day, with fentanyl accounting for nearly 80 per cent of those deaths.
Fentanyl, a synthetic opioid, is up to 50 times stronger than heroin and 100 times stronger than morphine. A dose as small as a few grains of salt can be lethal.
Given its potency, police and prosecutors have increasingly turned to manslaughter charges when a dealer’s product results in a fatal overdose.
A recent study in the Canadian Journal of Law and Society found that the number of manslaughter charges laid for drug-related deaths in Canada surged from three cases in 2016 to 135 in 2021.
Individuals can be convicted of manslaughter for committing unlawful, reckless or negligent acts that result in death but where there was no intention to kill. Sentences can range from probation (in rare cases) to life.
Murder charges, by contrast, require an intent to kill or cause fatal harm. Drug dealers typically face manslaughter charges in overdose cases, as their intent is to distribute drugs, not to kill those who purchase them.
Joanne Bortoluss, a spokesperson for the Durham Regional Police, which charged Norn, said that each of their investigations follows the same fundamental process.
“Investigators consider the strength of the evidence, the dealer’s level of involvement, and applicable laws when determining whether to pursue charges like manslaughter,” she said.
The Canadian Journal of Law and Society study also found that prosecutions often target low-level dealers, many of whom are drug users themselves and have personal connections to the deceased.
Norn’s case fits this pattern. He struggled with substance abuse, including addiction to fentanyl, Xanax and Percocet. Tyler and Norn were friends, the judge said in the court ruling, although Fowlie disputes this claim.
“[Those words] are repulsive to me,” she said.
The Crown argued Norn demonstrated “a high degree of moral blameworthiness” by warning Ginn of the fentanyl’s potency while still selling it to him. In a call to Ginn, he warned him “not to do a lot of the stuff” because he “didn’t want to be responsible for anything that happened.”
Fowlie’s outrage over Norn’s lenient sentencing is compounded by the fact that Norn was found trafficking fentanyl again after her son’s death.
“So we’ve killed somebody, and we’re still … trafficking? We’re not worried who else we kill?” Fowlie said.

Trafficking
Some legal sources noted that manslaughter charges do not necessarily lead to harsh sentences or deterrence.
“If you look at how diverse and … lenient some sentences are for manslaughter, I don’t think it really pushes things in the direction that [victims’ families] want,” said Kevin Westell, a Vancouver-based trial lawyer and former chair of the Canadian Bar Association.
Westell noted that the term “manslaughter” is misleading. “Manslaughter is a brutal-sounding title, but it encapsulates a very broad span of criminal offences,” he said.
In Westell’s view, consistently charging dealers with drug trafficking could be more effective for deterring the practice.
“What really matters is how long the sentence is, and you’re better off saying, ‘We know fentanyl is dangerous, so we’re setting the sentence quite high,’ rather than making it harder to prove with a manslaughter charge,” he said.
Trafficking is a distinct charge from manslaughter that involves the distribution, sale or delivery of illicit drugs. The sentencing range for fentanyl trafficking is eight to 15 years, Kwame Bonsu, a media relations representative for the Department of Justice, told Canadian Affairs.
“Courts must impose sentences that are proportionate to the gravity of the offence and the degree of responsibility of the offender,” Bonsu said, referencing a 2021 Supreme Court of Canada decision. Bonsu noted that aggravating factors such as lack of remorse or trafficking large quantities can lead to harsher sentences.
‘Head of the snake’
Some legal experts noted the justice system often fails to target those higher up in the drug supply chain.
“We don’t know how many hands that drug goes through,” said Thorning, the defence lawyer.
“Are the police going to prosecute every single person who provides fentanyl to another person? Jacob [Norn] was himself an addict trafficker — what about the person who supplied the substance to him?”
Thorning also questioned whether government agencies bear some responsibility. “Is some government agency’s failure to investigate how that drug came into the country partly responsible for the young man’s death?”
Westell, who has served as both a Crown prosecutor and criminal defence lawyer, acknowledged the difficulty of targeting higher-level traffickers.
“Cutting off the head of the snake does not align very well with the limitations of the international borders,” he said.
“Yes, there are transnational justice measures, but a lot gets lost, and as soon as you cross an international border of any kind, it becomes incredibly difficult to follow the chain in a linear way.”
Bortoluss, of the Durham police, said even prosecuting what appear to be obvious fentanyl-related deaths — such as Tyler Ginn’s — can be challenging. Witnesses can be reluctant to cooperate, fearing legal consequences. It can also be difficult to identify the source of drugs, as “transactions often involve multiple intermediaries and anonymous online sales.”
Another challenge in deterring fentanyl trafficking is the strong financial incentives of the trade.
“Even if [Norn] serves two to four years for killing somebody, but he could make a hundred thousand off of selling drugs, is it worth it?” Fowlie said.
Thorning agreed that the profit incentive can be incredibly powerful, outweighing the risk of a potential sentence.
“The more risky you make the behaviour, the greater the profit for a person who’s willing to break our laws, and the profit is the thing that generates the conduct,” he said.
A blunt instrument
Legal experts also noted the criminal justice system alone cannot solve the fentanyl crisis.
“Most people who have [lost] a loved one [to drug overdose] want to see a direct consequence to the person that’s responsible,” said Westell. “But I think they would also like to see something on a more macro level that helps eliminate the problem more holistically, and that can’t be [achieved through] crime and punishment alone.”
Thorning agrees.
“These are mental health .. [and] medical issues,” he said. “Criminal law is a blunt instrument [that is] not going to deal with these things effectively.”
Even Fowlie sees the problem as bigger than sentencing. Her son struggled with the stigma associated with therapy and medication, which made it difficult for him to seek help.
“We need to normalize seeing a therapist, like we normalize getting your eyes checked every year,” she said.
“Pot isn’t the gateway drug, trauma is a gateway drug.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle – or donate to our investigative journalism fund.
-

 2025 Federal Election2 days ago
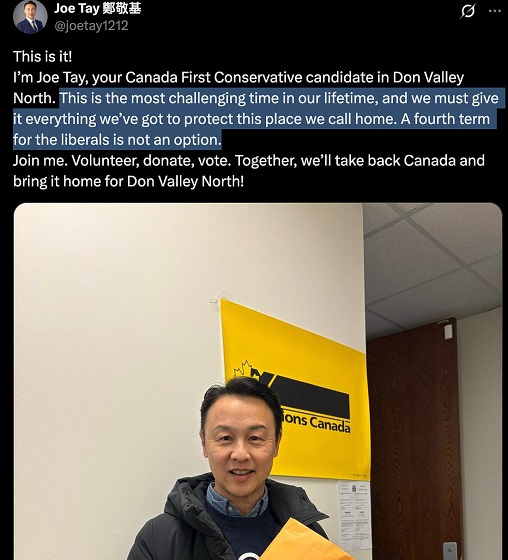
2025 Federal Election2 days agoJoe Tay Says He Contacted RCMP for Protection, Demands Carney Fire MP Over “Bounty” Remark
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoHong Kong-Canadian Groups Demand PM Carney Drop Liberal Candidate Over “Bounty” Remark Supporting CCP Repression
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPoilievre To Create ‘Canada First’ National Energy Corridor
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoAlcohol tax and MP pay hike tomorrow (April 1)
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoChina Election Interference – Parties Received Security Briefing Days Ago as SITE Monitors Threats to Conservative Candidate Joe Tay
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoFixing Canada’s immigration system should be next government’s top priority
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoPoilievre, Conservatives receive election endorsement from large Canadian trade union
-

 Bruce Dowbiggin2 days ago
Bruce Dowbiggin2 days agoAre the Jays Signing Or Declining? Only Vladdy & Bo Know For Sure