Addictions
Leading addiction doctor warns of Canada’s ‘safer supply’ disaster

A man considers using a prescription opioid. Credit: Dreamstime
By Liam Hunt
Addiction physician Dr. Sharon Koivu has seen the effects of safer supply programs in her clinical practice and personal life — and is sounding the alarm
Dr. Sharon Koivu, an addiction physician and parent, believes her son might not have survived to adulthood if Canada’s “safer supply” programs had been in effect during his adolescence.
Having worked on the front lines of Ontario’s opioid crisis, she views these programs as a catastrophic failure.
In an extended interview, Koivu explained the unintended consequences of these programs, which offer free tablets of hydromorphone — an opioid about as strong as heroin – to vulnerable patients with a history of addiction. While advocates of safer supply claim it mitigates the use of more dangerous illicit substances, there is evidence that most users divert — that is, sell or trade — their hydromorphone to acquire stronger substances.
Safer supply was first piloted in London, Ont., in 2016, before being widely expanded across Canada in 2020 with the help of generous federal grants. While the program looked good on paper, Koivu, who provides comprehensive addiction consultation services at a London-based hospital, saw a different reality: her patients were destabilizing, relapsing and fatally overdosing because of safer supply.
Koivu says that “one hundred percent” of her colleagues working in addiction medicine have noticed safer supply diversion. Some patients have told her they have been threatened with violence if they do not procure and divert these drugs. She estimates that, because of safer supply, tens of thousands of diverted hydromorphone pills — also known as “Dilaudid,” “dillies” or “D8s” — are flooding into Canadian streets every day.
For context, just two or three of these pills, if snorted, are enough to induce an overdose in a new user.
This influx has caused the drug’s street price to crash by as much as 95 per cent. While 8-milligram hydromorphone pills used to sell for $20 each several years ago, they can now be bought for as little as a dollar or two. These rock-bottom prices have ignited a new wave of addictions and relapses, and lured opioid-naive individuals into experimenting with what is essentially pharmaceutical heroin.
Koivu estimates that 80 per cent of her opioid-using patients now take diverted hydromorphone.
“The biggest harm is that we’ve turned on the tap and we’ve made everything cheap, which is leading to a large increase in the number of people becoming addicted and suffering,” she said.
“It is the most serious issue that I’ve seen in my lifetime.”
Safer supply programs seem to regularly overprescribe opioids without considering patients’ actual needs, Koivu says. Patients have come into her hospital with prescriptions that provide 40 eight-milligram hydromorphone pills a day, even though they can only tolerate 10 pills.
Subscribe to our newsletter to get our latest news and analysis – or donate to our investigative journalism fund.
‘That attraction is horrific’
Throughout the first few decades of Koivu’s career, almost “everyone” in her patient pool developed addictions due to childhood traumas or from mishandling opioids prescribed for chronic pain.
Since the advent of safer supply, the origins of new opioid addictions have shifted toward social or recreational exposure. Concerningly, this exposure often occurs in patients’ adolescent years.
“I’m seeing an increase in youth becoming addicted,” said Koivu, who has had patients as young as 15 tell her their addictions began through diverted hydromorphone.
“Almost everyone I see who’s started since 2018 started recreationally. It started as something that was at a party. It’s now a recreational drug at the youth level.”
Parents often seem completely unaware of the problem. Some have told Koivu they overheard their children discussing the availability of “D8s” at their highschools, only to later realize — when it was too late — they were referring to opioids.
“You can’t walk into your house with a six-pack of beer. If you’re smoking weed, people can smell it. But you can walk into your house with a lot of [tablets] in your pocket. So, it’s cheap, really easy to hide, and is even called ‘safe’ by the government. I think that attraction is horrific.”
“Our youth are dying at a higher rate … and we have a lot more hydromorphone found in [their bodies] at the time of death.”
While safer supply programs claim to make communities safer, Koivu’s lived experiences suggest the opposite. She used to reside in London’s Old East Village, where the city’s first safer supply program opened in 2016, but moved away after watching her neighbourhood deteriorate from widespread crime, overdoses and drug trafficking.
“I moved there to support a supervised injection site,” said Koivu. “Then I watched that community drastically change when safer supply was implemented. … I would go for walks and directly see diversion taking place. Homelessness is very complicated, but this has absolutely fueled it in ways that are unconscionable.”
Koivu characterizes the evidentiary standards used by advocates of safer supply as “deeply problematic.” She says many of the studies supporting safer supply are qualitative — meaning they rely on interviews — and use anecdotal data from patients who have a vested interest in perpetuating the program.
While Koivu has been blowing the whistle on safer supply programs for years, her concerns largely went unnoticed until recently. She has faced years of harassment and denigration for her views.
“When I came to say I’m concerned about what I’m seeing: the infections, the suffering, the encampments … I was literally told that I was lying,” she said.
Last month, the London Police Service provided the National Post with data showing that annual hydromorphone seizures increased by 3,000 per cent after access to safer supply was significantly expanded in 2020. The newspaper has since raised questions about why this data was not released earlier and whether the police stonewalled attempts to investigate the issue.
Koivu considers herself a lifelong progressive and has historically supported the New Democratic Party. But she is concerned many left-leaning politicians have ignored criticism of safer supply. Many seemingly believe that opposition to it is inherently conservative.
“I went to a hearing in Ottawa of a standing committee to talk about addiction,” she said. “We had five minutes to give a talk, and then two hours to answer questions, [but] I didn’t receive any questions from the NDP or the Liberals.”
Although Koivu believes safe supply can play a role in the continuum of care for opioid addiction, she says it must be executed in a meticulous manner that prevents diversion and emphasizes pathways to recovery.
“It needs to be part of a comprehensive strategy to help people get their lives back. And right now, it’s not.”
Above all, it is Koivu’s experience as a mother that drives her to criticize safer supply. One of her sons struggled with opioid addiction as a young adult. Although he eventually recovered, the experience could have killed him.
“Had this program been around … my family could have been another statistic from an opioid death. That drives me. Because it’s very real, and it’s very personal.”
|
|
A guest post by
|
Subscribe to Break The Needle. Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
2025 Federal Election
Poilievre to invest in recovery, cut off federal funding for opioids and defund drug dens

From Conservative Party Communications
Poilievre will Make Recovery a Reality for 50,000 Canadians
Conservative Leader Pierre Poilievre pledged he will bring the hope that our vulnerable Canadians need by expanding drug recovery programs, creating 50,000 new opportunities for Canadians seeking freedom from addiction. At the same time, he will stop federal funding for opioids, defund federal drug dens, and ensure that any remaining sites do not operate within 500 meters of schools, daycares, playgrounds, parks and seniors’ homes, and comply with strict new oversight rules that focus on pathways to treatment.
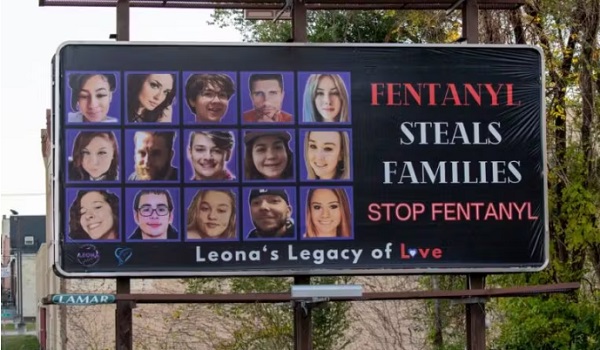
More than 50,000 people have lost their lives to fentanyl since 2015—more Canadians than died in the Second World War. Poilievre pledged to open a path to recovery while cracking down on the radical Liberal experiment with free access to illegal drugs that has made the crisis worse and brought disorder to local communities.
Specifically, Poilievre will:
- Fund treatment for 50,000 Canadians. A new Conservative government will fund treatment for 50,000 Canadians in treatment centres with a proven record of success at getting people off drugs. This includes successful models like the Bruce Oake Recovery Centre, which helps people recover and reunite with their families, communities, and culture. To ensure the best outcomes, funding will follow results. Where spaces in good treatment programs exist, we will use them, and where they need to expand, these funds will allow that.
- Ban drug dens from being located within 500 metres of schools, daycares, playgrounds, parks, and seniors’ homes and impose strict new oversight rules. Poilievre also pledged to crack down on the Liberals’ reckless experiments with free access to illegal drugs that allow provinces to operate drug sites with no oversight, while pausing any new federal exemptions until evidence justifies they support recovery. Existing federal sites will be required to operate away from residential communities and places where families and children frequent and will now also have to focus on connecting users with treatment, meet stricter regulatory standards or be shut down. He will also end the exemption for fly-by-night provincially-regulated sites.
“After the Lost Liberal Decade, Canada’s addiction crisis has spiralled out of control,” said Poilievre. “Families have been torn apart while children have to witness open drug use and walk through dangerous encampments to get to school. Canadians deserve better than the endless Liberal cycle of crime, despair, and death.”
Since the Liberals were first elected in 2015, our once-safe communities have become sordid and disordered, while more and more Canadians have been lost to the dangerous drugs the Liberals have flooded into our streets. In British Columbia, where the Liberals decriminalized dangerous drugs like fentanyl and meth, drug overdose deaths increased by 200 percent.
The Liberals also pursued a radical experiment of taxpayer-funded hard drugs, which are often diverted and resold to children and other vulnerable Canadians. The Vancouver Police Department has said that roughly half of all hydromorphone seizures were diverted from this hard drugs program, while the Waterloo Regional Police Service and Niagara Regional Police Service said that hydromorphone seizures had exploded by 1,090% and 1,577%, respectively.
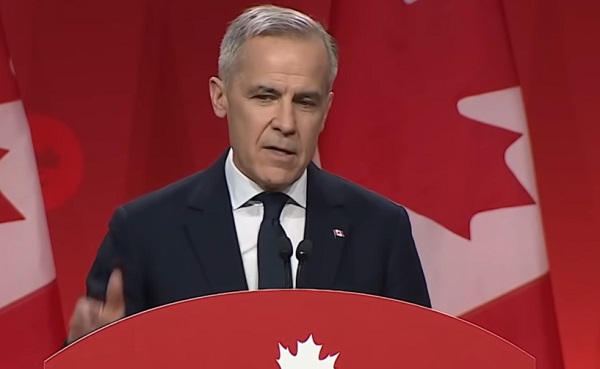
Despite the death and despair that is now common on our streets, bizarrely Mark Carney told a room of Liberal supporters that 50,000 fentanyl deaths in Canada is not “a crisis.” He also hand-picked a Liberal candidate who said the Liberals “would be smart to lean into drug decriminalization” and another who said “legalizing all drugs would be good for Canada.”
Carney’s star candidate Gregor Robertson, an early advocate of decriminalization and so-called safe supply, wanted drug dens imposed on communities without any consultation or public safety considerations. During his disastrous tenure as Vancouver Mayor, overdoses increased by 600%.
Alberta has pioneered an approach that offers real hope by adopting a recovery-focused model of care, leading to a nearly 40 percent reduction in drug-poisoning deaths since 2023—three times the decrease seen in British Columbia. However, we must also end the Liberal drug policies that have worsened the crisis and harmed countless lives and families.
To fund this policy, a Conservative government will stop federal funding for opioids, defund federal drug dens, and sue the opioid manufacturers and consulting companies who created this crisis in the first place.
“Canadians deserve better than the Liberal cycle of crime, despair, and death,” said Poilievre. “We will treat addiction with compassion and accountability—not with more taxpayer-funded poison. We will turn hurt into hope by shutting down drug dens, restoring order in our communities, funding real recovery, and bringing our loved ones home drug-free.”
Addictions
There’s No Such Thing as a “Safer Supply” of Drugs

By Adam Zivo
Sweden, the U.K., and Canada all experimented with providing opioids to addicts. The results were disastrous.
[This article was originally published in City Journal, a public policy magazine and website published by the Manhattan Institute for Policy Research. We encourage our readers to subscribe to them for high-quality analysis on urban issues]
Last August, Denver’s city council passed a proclamation endorsing radical “harm reduction” strategies to address the drug crisis. Among these was “safer supply,” the idea that the government should give drug users their drug of choice, for free. Safer supply is a popular idea among drug-reform activists. But other countries have already tested this experiment and seen disastrous results, including more addiction, crime, and overdose deaths. It would be foolish to follow their example.
The safer-supply movement maintains that drug-related overdoses, infections, and deaths are driven by the unpredictability of the black market, where drugs are inconsistently dosed and often adulterated with other toxic substances. With ultra-potent opioids like fentanyl, even minor dosing errors can prove fatal. Drug contaminants, which dealers use to provide a stronger high at a lower cost, can be just as deadly and potentially disfiguring.
Because of this, harm-reduction activists sometimes argue that governments should provide a free supply of unadulterated, “safe” drugs to get users to abandon the dangerous street supply. Or they say that such drugs should be sold in a controlled manner, like alcohol or cannabis—an endorsement of partial or total drug legalization.
But “safe” is a relative term: the drugs championed by these activists include pharmaceutical-grade fentanyl, hydromorphone (an opioid as potent as heroin), and prescription meth. Though less risky than their illicit alternatives, these drugs are still profoundly dangerous.
The theory behind safer supply is not entirely unreasonable, but in every country that has tried it, implementation has led to increased suffering and addiction. In Europe, only Sweden and the U.K. have tested safer supply, both in the 1960s. The Swedish model gave more than 100 addicts nearly unlimited access through their doctors to prescriptions for morphine and amphetamines, with no expectations of supervised consumption. Recipients mostly sold their free drugs on the black market, often through a network of “satellite patients” (addicts who purchased prescribed drugs). This led to an explosion of addiction and public disorder.
Most doctors quickly abandoned the experiment, and it was shut down after just two years and several high-profile overdose deaths, including that of a 17-year-old girl. Media coverage portrayed safer supply as a generational medical scandal and noted that the British, after experiencing similar problems, also abandoned their experiment.
While the U.S. has never formally adopted a safer-supply policy, it experienced something functionally similar during the OxyContin crisis of the 2000s. At the time, access to the powerful opioid was virtually unrestricted in many parts of North America. Addicts turned to pharmacies for an easy fix and often sold or traded their extra pills for a quick buck. Unscrupulous “pill mills” handed out prescriptions like candy, flooding communities with OxyContin and similar narcotics. The result was a devastating opioid epidemic—one that rages to this day, at a cumulative cost of hundreds of thousands of American lives. Canada was similarly affected.
The OxyContin crisis explains why many experienced addiction experts were aghast when Canada greatly expanded access to safer supply in 2020, following a four-year pilot project. They worried that the mistakes of the recent past were being made all over again, and that the recently vanquished pill mills had returned under the cloak of “harm reduction.”
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Most Canadian safer-supply prescribers dispense large quantities of hydromorphone with little to no supervised consumption. Patients can receive up to 40 eight-milligram pills per day—despite the fact that just two or three are enough to cause an overdose in someone without opioid tolerance. Some prescribers also provide supplementary fentanyl, oxycodone, or stimulants.
Unfortunately, many safer-supply patients sell or trade a significant portion of these drugs—primarily hydromorphone—in order to purchase more potent illicit substances, such as street fentanyl.
The problems with safer supply entered Canada’s consciousness in mid-2023, through an investigative report I wrote for the National Post. I interviewed 14 addiction physicians from across the country, who testified that safer-supply diversion is ubiquitous; that the street price of hydromorphone collapsed by up to 95 percent in communities where safer supply is available; that youth are consuming and becoming addicted to diverted safer-supply drugs; and that organized crime traffics these drugs.
Facing pushback, I interviewed former drug users, who estimated that roughly 80 percent of the safer-supply drugs flowing through their social circles was getting diverted. I documented dozens of examples of safer-supply trafficking online, representing tens of thousands of pills. I spoke with youth who had developed addictions from diverted safer supply and adults who had purchased thousands of such pills.
After months of public queries, the police department of London, Ontario—where safer supply was first piloted—revealed last summer that annual hydromorphone seizures rose over 3,000 percent between 2019 and 2023. The department later held a press conference warning that gangs clearly traffic safer supply. The police departments of two nearby midsize cities also saw their post-2019 hydromorphone seizures increase more than 1,000 percent.
The Canadian government quietly dropped its support for safer supply last year, cutting funding for many of its pilot programs. The province of British Columbia (the nexus of the harm-reduction movement) finally pulled back support last month, after a leaked presentation confirmed that safer-supply drugs are getting sold internationally and that the government is investigating 60 pharmacies for paying kickbacks to safer-supply patients. For now, all safer-supply drugs dispensed within the province must be consumed under supervision.
Harm-reduction activists have insisted that no hard evidence exists of widespread diversion of safer-supply drugs, but this is only because they refuse to study the issue. Most “studies” supporting safer supply are produced by ideologically driven activist-scholars, who tend to interview a small number of program enrollees. These activists also reject attempts to track diversion as “stigmatizing.”
The experiences of Sweden, the United Kingdom, and Canada offer a clear warning: safer supply is a reliably harmful policy. The outcomes speak for themselves—rising addiction, diversion, and little evidence of long-term benefit.
As the debate unfolds in the United States, policymakers would do well to learn from these failures. Americans should not be made to endure the consequences of a policy already discredited abroad simply because progressive leaders choose to ignore the record. The question now is whether we will repeat others’ mistakes—or chart a more responsible course.
Our content is always free –
but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
-

 Also Interesting1 day ago
Also Interesting1 day agoMortgage Mayhem: How Rising Interest Rates Are Squeezing Alberta Homeowners
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoConservative Party urges investigation into Carney plan to spend $1 billion on heat pumps
-

 Alberta2 days ago
Alberta2 days agoAlberta’s embrace of activity-based funding is great news for patients
-
 2025 Federal Election2 days ago
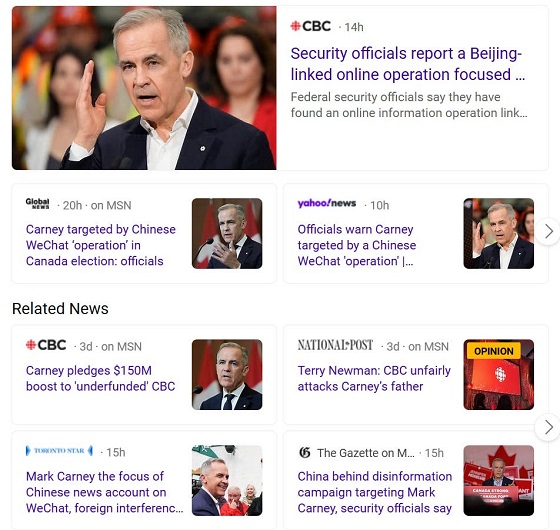
2025 Federal Election2 days agoCommunist China helped boost Mark Carney’s image on social media, election watchdog reports
-

 Also Interesting2 days ago
Also Interesting2 days agoExploring Wildrobin Technological Advancements in Live Dealer Games
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoCorporate Media Isn’t Reporting on Foreign Interference—It’s Covering for It
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoFifty Shades of Mark Carney
-

 Justice1 day ago
Justice1 day agoCanadian government sued for forcing women to share spaces with ‘transgender’ male prisoners