Health
National pharmacare – might it be a pig in a poke?

From the Macdonald Laurier Institute
By Nigel Rawson and John Adams for Inside Policy
No Canadian should have to choose between paying for medicines and paying for rent or food. National pharmacare has been proposed as a remedy to this situation.
“When will Canada have national pharmacare?” asks the author of a recent article in the British Medical Journal (BMJ). Better questions are: will Canadian pharmacare be the system many Canadians hope for? Or, might it turn out to be skimpy coverage akin to minimum wage laws?
In its 2024 budget document, the federal government proposed providing $1.5 billion over five years to support the launch of national pharmacare for “universal, single-payer coverage for a number of contraception and diabetes medications.” This has been hailed as a “big day for pharmacare” by some labour unions, patients and others, including the author of the BMJ article who said that national pharmacare should be expanded to cover all medication needs beginning with the most commonly-prescribed, clinically-important “essential medicines.”
In its budget, the government stated “coverage of contraceptives will mean that nine million women in Canada will have better access to contraception” and “improving access to diabetes medications will help improve the health of 3.7 million Canadians with diabetes.” Why not salute such affable, motherhood and apple pie, sentiments? The devil is in the details.
The plan does not cover new drugs for diabetes, such as Ozempic, Rybelsus, Wegovy, Mounjaro or Zepbound, all based on innovative GLP-1 agonists, where evidence is building for cardiovascular and weight loss benefits. This limited rollout seems based on cheap, older medicines, which can be less effective for some with diabetes.
The federal government has also consistently under-estimated the cost of national proposals such as pharmacare – not to mention other promises. In their 2019 election platform, the Liberals promised $6 billion for national pharmacare (the NDP promised $10 billion). Keen analysis shows that even these expansive amounts would be woefully inadequate to fund a full national pharmacare plan. This makes the $300 million a year actually proposed by the Liberals’ look like the skimpy window-dressing that it is.
National pharmacare, based on the most comprehensive existing public drug plan (Quebec’s), would cost much more. In 2017, using optimistic assumptions, the Parliamentary Budget Officer (PBO) estimated the cost for a national plan based on Quebec’s experience to be $19.3 billion a year. With more appropriate assumptions, the Canadian Health Policy Institute estimated $26.2 billion. In June 2019, the federal government’s own Advisory Council on the Implementation of National Pharmacare put the cost at $40 billion, while a few months later, the tax consulting company RSM Canada projected $48.3 to $52.5 billion per year. Five years later, costs no doubt have soared.
Even with these staggering cost a program based on matching Quebec’s drug plan at the national level would fail to provide anywhere near the level of coverage already provided to the almost two-thirds of Canadians who have private drug insurance, including many in unionized jobs. Are they willing to sacrifice their superior coverage, especially of innovative brand-name medicines, for a program covering only “essential medicines”? Put another way, are Canadians and their unions prepared to settle for the equivalent of a minimum wage or minimum benefits?
The PBO has estimated the cost of coverage of a range of contraceptives and diabetes medicines as $1.9 billion over five years, which is more than the $1.5 billion provided in the budget. However, this figure is based on an assumption that the new program would only cover Canadians who currently do not have public or private drug plan insurance, those who currently do not fill their prescriptions due to cost related reasons, and the out-of-pocket part of prescription costs for Canadians who have public or private drug plan coverage. This is major guesswork because existing public and private drug plans may see the new federal program as an opportunity to reduce their costs by requiring their beneficiaries to use the new program. If this occurs, the national pharmacare costs to the federal government, even for the limited role out of diabetes and contraceptives, would soar to an estimated $5.7 billion, according to the PBO.
Our governments are not known for accurate estimates of the costs of new programs. One has only to remember the Phoenix pay system and the ArriveCAN costs. In 2017, the Government of Ontario estimated $465 million per year to extend drug coverage to every resident under the age of 25 years. What happened? Introduced in 2018, prescriptions rose by 290% and drug expenditure increased to $839 million – almost double the guesstimate. In 2019, the provincial government back peddled and modified the program to cover only people not already insured by a private plan.
Although we believe governments should facilitate access to necessary medicines for Canadians who cannot afford their medicines, this does not require national pharmacare and a growing bureaucracy. Exempting lower-income Canadians from copayments and premiums required by provincial programs, as British Columbia has done, and removing the requirement to pay for all drugs up to a deductible would allow these Canadians access sooner, more simply, and more effectively.
Moreover, it isn’t just lower-income Canadians who want help with unmet medicine needs. Canadians who need access to drugs for diseases that are difficult to treat and can cost hundreds of thousands of dollars per year also require assistance. Few Canadians whether they have low, medium or high incomes can afford these prices without government or private insurance. Private insurers often refuse to cover these drugs.
The Liberals provided a separate $1.5 billion over three years for drugs for rare disorders, but no province or territory has signed a bilateral agreement with the federal government for these drugs and no patient has received benefit through this program. Even if they did, the $500 million per year would not go far towards the actual costs. There is at least a zero missing in the federal contribution, as the projected cost of public spending on rare disease medicines by 2025 is more than threefold what Ottawa has budgeted.
Expensive drugs for cancer and rare disorders are just as essential as basic medicines for cardiovascular diseases, diabetes, birth control, and many other common conditions. If a costly medicine will allow a person with a life-shortening disease to live longer or one with a disorder that will be severely disabling left untreated to have an improved quality of life and be a productive taxpayer, it too should be regarded as essential.
The Liberals and NDP are working to stampede the bill to introduce the pharmacare program (Bill C-64) through the legislative process. This includes inviting witnesses over the first long weekend of summer, when many Canadians are away, to appear before the parliamentary Standing Committee on Health three days later.
Too much is unknown about what will be covered (will newer drugs be covered or only older, cheaper medicines?), who will be eligible for coverage (all appropriate Canadians regardless of existing coverage or only those with no present coverage?), and what the real cost will be, including whether a new program focusing on older, cheaper drugs will deter drug developers from launching novel medicines for unmet needs in Canada.
This Bill as it stands is such a power grab that, if passed, the federal Health Minister never has to come back to Parliament for review, oversight or another tranche of legal authority, it would empower the Cabinet to make rules and regulations without parliamentary scrutiny.
A lot is at stake for Canadians, especially for patients and their doctors. Prescription medicines are of critical importance to treating many diseases. National pharmacare must not only allow low-income residents to access purported “essential medicines” but also ensure that patients who need specialized drugs, especially higher-cost innovative cell and genetic therapies that may be the only effective treatment for their disorder, are not ignored. Canadians should be careful what they wish for. They may receive less than they anticipate, and, in fact, many Canadians may be worse off despite the increase in public spending. Time to look under the hood and kick the tires.
Nigel Rawson is a senior fellow with the Macdonald-Laurier Institute.
John Adams is co-founder and CEO of Canadian PKU and Allied Disorders Inc., a senior fellow with the Macdonald-Laurier Institute and volunteer board chair of Best Medicines Coalition.
Alberta
MAiD In Alberta: Province surveying Albertans about assisted suicide policies

Alberta’s government is launching a public engagement to gather input about legislation and policies around assisted suicide, also referred to as medical assistance in dying (MAID).
Medical assistance in dying is a process that allows an eligible person to receive assistance from a medical practitioner in ending their life. To be found eligible, a person must be suffering from a serious and permanent medical condition.
Alberta’s government is reviewing how MAID is regulated to ensure there is a consistent process as well as oversight that protects vulnerable Albertans, specifically those living with disabilities or suffering from mental health challenges. An online survey is now open for Albertans to share their views and experiences with MAID until Dec. 20.
“We recognize that medical assistance in dying is a very complex and often personal issue and is an important, sensitive and emotional matter for patients and their families. It is important to ensure this process has the necessary supports to protect the most vulnerable. I encourage Albertans who have experience with and opinions on MAID to take this survey.”
In addition to the online survey, Alberta’s government will also be engaging directly with academics, medical associations, public bodies, religious organizations, regulatory bodies, advocacy groups and others that have an interest in and/or working relationship to the MAID process, health care, disabilities and mental health care.
Feedback gathered through this process will help inform the Alberta government’s planning and policy decision making, including potential legislative changes regarding MAID in Alberta.
“Our government has been clear that we do not support the provision of medically assisted suicide for vulnerable Albertans facing mental illness as their primary purpose for seeking their own death. Instead, our goal is to build a continuum of care where vulnerable Albertans can live in long-term health and fulfilment. We look forward to the feedback of Albertans as we proceed with this important issue.”
“As MAID is a federally legislated and regulated program that touches the lives of many Albertans, our priority is to ensure we have robust safeguards to protect vulnerable individuals. Albertans’ insights will be essential in developing thoughtful policies on this complex issue.”
The federal Criminal Code sets out the MAID eligibility criteria, procedural safeguards and reporting obligations. The federal government has paused MAID eligibility for individuals with a mental illness as their sole underlying medical condition until March 2027 to ensure the provincial health care systems have processes and supports in place. Alberta’s government does not support expanding MAID eligibility to include those facing depression or mental illness and continues to call on the federal government to end this policy altogether.
Related information
Alberta
On gender, Alberta is following the science
Despite falling into disrepute in recent years, “follow the science” remains our best shot at getting at the truth of the physical sciences.
But science, if we are to place our trust in it, must be properly defined and understood; it is at its essence an ever-changing process, a relentless pursuit of truth that is never “settled,” and one that is unafraid to discard old hypotheses in the face of new evidence.
And it is in this light—in the unforgiving glare of honest science—that Alberta Premier Danielle Smith’s three new legislative initiatives around gender policy are properly understood, notwithstanding the opprobrium they’ve attracted from critics.
Bill 26, the Health Statutes Amendment Act, proposes to prohibit the prescription of puberty blockers and cross-gender hormones for the treatment of gender dysphoria to youth aged 15 and under. It would allow minors aged 16 and 17 to begin puberty blockers and hormone therapies for gender “reassignment” and “affirmation” purposes only with parental, physician, and psychologist approval. The bill also prohibits health professionals from performing sex reassignment surgeries on minors.
Bill 27, the Education Amendment Act, seeks to enshrine parents’ rights to be notified if their kids change their names/pronouns at school, and it gives parents the right to “opt in” to what sort of gender and sex education their kids are exposed to in school.
And Bill 29, the Fairness and Safety in Sports Act, is designed to protect females in sports by ensuring that women and girls can compete in biological female-only divisions, while supporting the formation of co-ed opportunities to support transgender athletes.
Each of these initiatives is entirely reasonable, given what we know of the science underpinning “gender care,” and of the undeniable advantages that a male physique confers upon biological males competing in sports.
The notion that the trifecta of puberty blockers, cross-gender hormones, and revisionist surgery is a pathway to good health was a hypothesis initially devised by Dutch researchers, who were looking to ease the discomfort of transgender adults struggling with incongruence between their physical appearance and their gender identities. As a hypothesis, it was perhaps reasonable.
But as the UK’s Cass Review exposed in withering detail last spring, its premises were wholly unsupported by evidence, and its implementation has caused grievous harm for youth. As Finnish psychiatrist Riittakerttu Kaltiala, one of the architects of that country’s gender program, put it last year, “Gender affirming care is dangerous. I know, because I helped pioneer it.”
It’s no accident, then, that numerous European jurisdictions have pulled back from the “gender affirming care” pathway for youth, such as Sweden, Finland, Belgium, the Netherlands, and the United Kingdom.
It makes perfect sense that Canadians should be cautious as well, and that parents should be apprised if their children are being exposed to these theories at school and informed if their kids are caught up in their premises.
Yet the Canadian medical establishment has remained curiously intransigent on this issue, continuing to insist that the drug-and-surgery-based gender-affirming care model is rooted in evidence.
Premier Smith was asked by a reporter last month whether decisions on these matters aren’t best left to discussions between doctors and their patients; to which she replied:
“I would say doctors aren’t always right.”
Which is rather an understatement, as anyone familiar with the opioid drug crisis can attest, or as anyone acquainted with the darker corners of medical history knows: the frontal lobotomy saga, the thalidomide catastrophe, and the “recovered memories of sexual abuse” scandal are just a few examples of where doctors didn’t “get it right.”
As physicians, we advocate strongly for self-regulation and for the principle that medical decisions are private matters between physicians and patients. But self-regulation isn’t infallible, and when it fails it can be very much in the interests of the public—and especially of patients—for others to intervene, whether they be journalists, lawyers, or political leaders.
The trans discussion shouldn’t be a partisan issue, although it certainly has become one in Canada. It’s worth noting that Britain’s freshly elected Labour Party chose to carry on with the cautious approach adopted by the preceding administration in light of the Cass Review.
Premier Smith’s new polices are eminently sensible and in line with the stance taken by our European colleagues. None of her initiatives are “anti-trans.” Instead, they are pro-child, pro-women, and pro-athlete, and it’s difficult to see how anyone can quibble with that.
Dr. J. Edward Les, MD, is a pediatrician in Calgary, senior fellow at the Aristotle Foundation for Public Policy, and co-author of Teenagers, Children, and Gender Transition Policy: A Comparison of Transgender Medical Policy for Minors in Canada, the United States, and Europe.
-

 Brownstone Institute10 hours ago
Brownstone Institute10 hours agoThe Most Devastating Report So Far
-
 Economy22 hours ago
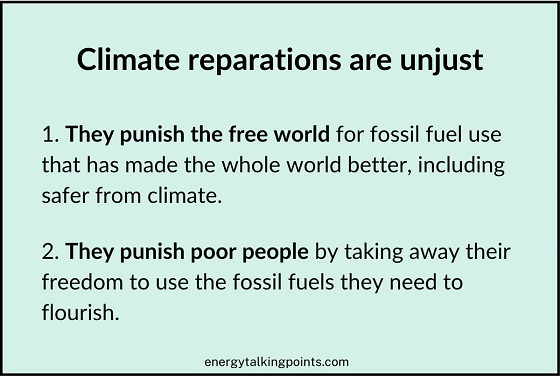
Economy22 hours agoCOP 29 leaders demand over a $1 trillion a year in climate reparations from ‘wealthy’ nations. They don’t deserve a nickel.
-
 Censorship Industrial Complex14 hours ago
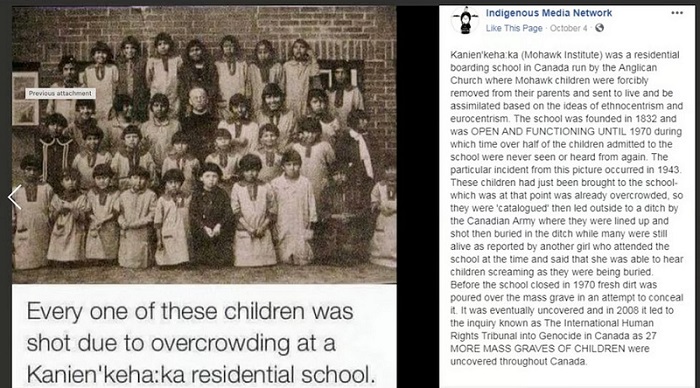
Censorship Industrial Complex14 hours agoAnother Mass Grave?
-

 Alberta13 hours ago
Alberta13 hours agoMAiD In Alberta: Province surveying Albertans about assisted suicide policies
-
 Alberta20 hours ago
Alberta20 hours agoOn gender, Alberta is following the science
-

 Energy21 hours ago
Energy21 hours agoOttawa’s proposed emission cap lacks any solid scientific or economic rationale
-

 Bruce Dowbiggin9 hours ago
Bruce Dowbiggin9 hours agoCHL Vs NCAA: Finally Some Sanity For Hockey Families
-

 Brownstone Institute2 days ago
Brownstone Institute2 days agoFirst Amendment Blues



