Health
UK pediatrician who led review of child ‘transitions’ says US medical groups ‘misleading the public’

Dr. Hilary Cass, author of the Cass Review
From LifeSiteNews
The American Academy of Pediatrics’ support for surgically and chemically mutilating gender-confused children ‘is now demonstrated to be out of date by multiple systematic reviews,’ Dr. Hilary Cass told the New York Times.
The typically left-wing New York Times published an interview on Monday with consultant pediatrician Dr. Hilary Cass on her comprehensive review of so-called “gender medicine” in the United Kingdom, indicating that awareness of the damage due to surgical and chemical “transitioning” continues to spread despite the best efforts of LGBT activists.
Released in April, 366-page Cass Review was commissioned by National Health Service (NHS) England following ongoing scandals about the practices of British “gender clinics” such as the Gender Identity Development Service (GIDS), operated by the Tavistock and Portman NHS Foundation Trust. The four-year project consisted of comprehensive reviews of current research and international standards, as well as extensive interviews with gender-confused children and adults, family members, detransitioners, doctors, and activists.
It found that “gender medicine” is “built on shaky foundations” and that while such interventions require a great deal of caution, “quite the reverse happened in the field of [so-called] gender care for children,” and that “[w]hile a considerable amount of research has been published in this field, systematic evidence reviews demonstrated the poor quality of the published studies, meaning there is not a reliable evidence base upon which to make clinical decisions, or for children and their families to make informed choices.” Her findings led NHS to stop prescribing puberty blockers to children with gender confusion earlier this year.
Speaking to the Times, Cass explained that she was planning her retirement when she was first asked to tackle the project and was initially apprehensive about wading into the controversy.
“The most important concern for me is just how poor the evidence base is in this area,” she said. “Some people have questioned, ‘Did we set a higher bar for this group of young people?’ We absolutely didn’t. The real problem is that the evidence is very weak compared to many other areas of pediatric practice.”
The Times acknowledged that her “findings are in line with several European countries that have limited the treatments [sic] after scientific reviews. But in America, where nearly two dozen states have banned the care outright, medical groups have endorsed the treatments as evidence-based and necessary,” including groups the paper contacted for its latest story. Cass described American medical consensus as “out of date” on the issue.
“When I was president of the Royal College of Pediatrics and Child Health, we did some great work with the A.A.P. [American Academy of Pediatrics],” she elaborated. “They are an organization that I have enormous respect for. But I respectfully disagree with them on holding on to a position that is now demonstrated to be out of date by multiple systematic reviews.”
“It wouldn’t be too much of a problem if people were saying ‘This is clinical consensus and we’re not sure,” she added. “But what some organizations are doing is doubling down on saying the evidence is good. And I think that’s where you’re misleading the public. You need to be honest about the strength of the evidence and say what you’re going to do to improve it.”
A significant body of evidence shows that “affirming” gender confusion carries serious harms, especially when done with impressionable children who lack the mental development, emotional maturity, and life experience to consider the long-term ramifications of the decisions being pushed on them.
Studies find that more than 80% of children experiencing gender dysphoria outgrow it on their own by late adolescence, and that even full “reassignment” surgery often fails to resolve gender-confused individuals’ heightened tendency to engage in self-harm and suicide — and may even exacerbate it, including by reinforcing their confusion and neglecting the actual root causes of their mental strife.
Yet while mounting evidence against youth “gender transitions” is prompting European nations such as the United Kingdom and France, which are normally to the left of America, to move away from the practice, in America, the medical establishment and the Biden administration continues to dig in their heels, despite Biden’s own Substance Abuse & Mental Health Services Administration (SAMHSA) releasing a since-deleted report last year acknowledging that “lesbian, gay, and bisexual adults are more likely than straight adults to use substances, experience mental health conditions including major depressive episodes, and experience serious thoughts of suicide.”
The White House’s comprehensive pursuit of the transgender agenda has included reopening the military to recruits afflicted with gender dysphoria, promoting gender ideology within the military (including “diversity” and drag events on military bases), holding White House events to “affirm transgender kids,” condemning state laws against underage “transitions” as “close to sinful,” promoting underage “transitions” (potentially at taxpayer expense) as a “best practice,” and trying to force federally funded schools to let males into female athletic competitions and restrooms.
armed forces
Yet another struggling soldier says Veteran Affairs Canada offered him euthanasia

From LifeSiteNews
‘It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself.’
Yet another Canadian combat veteran has come forward to reveal that when he sought help, he was instead offered euthanasia.
David Baltzer, who served two tours in Afghanistan with the Princess Patricia’s Canadian Light Infantry, revealed to the Toronto Sun that he was offered euthanasia on December 23, 2019—making him, as the Sun noted, “among the first Canadian soldiers offered therapeutic suicide by the federal government.”
Baltzer had been having a disagreement with his existing caseworker, when assisted suicide was brought up in in call with a different agent from Veteran Affairs Canada.
“It made me wonder, were they really there to help us, or slowly groom us to say ‘here’s a solution, just kill yourself,” Baltzer told the Sun.“I was in my lowest down point, it was just before Christmas. He says to me, ‘I would like to make a suggestion for you. Keep an open mind, think about it, you’ve tried all this and nothing seems to be working, but have you thought about medical-assisted suicide?’”
Baltzer was stunned. “It just seems to me that they just want us to be like ‘f–k this, I give up, this sucks, I’d rather just take my own life,’” he said. “That’s how I honestly felt.”
Baltzer, who is from St. Catharines, Ontario, joined up at age 17, and moved to Manitoba to join the Princess Patricia’s Canadian Light Infantry, one of Canada’s elite units. He headed to Afghanistan in 2006. The Sun noted that he “was among Canada’s first troops deployed to Afghanistan as part Operation Athena, where he served two tours and saw plenty of combat.”
“We went out on long-range patrols trying to find the Taliban, and that’s exactly what we did,” Baltzer said. “The best way I can describe it, it was like Black Hawk Down — all of the sudden the s–t hit the fan and I was like ‘wow, we’re fighting, who would have thought? Canada hasn’t fought like this since the Korean War.”
After returning from Afghanistan, Baltzer says he was offered counselling by Veteran Affairs Canada, but it “was of little help,” and he began to self-medicate for his trauma through substance abuse (he noted that he is, thankfully, doing well today). Baltzer’s story is part of a growing scandal. As the Sun reported:
A key figure shedding light on the VAC MAID scandal was CAF veteran Mark Meincke, whose trauma-recovery podcast Operation Tango Romeo broke the story. ‘Veterans, especially combat veterans, usually don’t reach out for help until like a year longer than they should’ve,’ Meincke said, telling the Sun he waited over two decades before seeking help.
‘We’re desperate by the time we put our hands up for help. Offering MAID is like throwing a cinderblock instead of a life preserver.’ Meincke said Baltzer’s story shoots down VAC’s assertions blaming one caseworker for offering MAID to veterans, and suggests the problem is far more serious than some rogue public servant.
‘It had to have been policy. because it’s just too many people in too many provinces,” Meincke told the Sun. “Every province has service agents from that province.’
Veterans Affairs Canada claimed in 2022 that between four and 20 veterans had been offered assisted suicide; Meincke “personally knows of five, and said the actual number’s likely close to 20.” In a previous investigation, VAC claimed that only one caseworker was responsible—at least for the four confirmed cases—and that the person “was lo longer employed with VAC.” Baltzer says VAC should have military vets as caseworkers, rather than civilians who can’t understand what vets have been through.
To date, no federal party leader has referenced Canada’s ongoing euthanasia scandals during the 2025 election campaign.
2025 Federal Election
Study links B.C.’s drug policies to more overdoses, but researchers urge caution
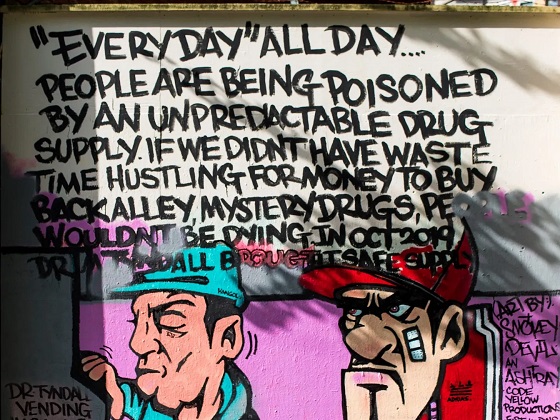
By Alexandra Keeler
A study links B.C.’s safer supply and decriminalization to more opioid hospitalizations, but experts note its limitations
A new study says B.C.’s safer supply and decriminalization policies may have failed to reduce overdoses. Furthermore, the very policies designed to help drug users may have actually increased hospitalizations.
“Neither the safer opioid supply policy nor the decriminalization of drug possession appeared to mitigate the opioid crisis, and both were associated with an increase in opioid overdose hospitalizations,” the study says.
The study has sparked debate, with some pointing to it as proof that B.C.’s drug policies failed. Others have questioned the study’s methodology and conclusions.
“The question we want to know the answer to [but cannot] is how many opioid hospitalizations would have occurred had the policy not have been implemented,” said Michael Wallace, a biostatistician and associate professor at the University of Waterloo.
“We can never come up with truly definitive conclusions in cases such as this, no matter what data we have, short of being able to magically duplicate B.C.”
Jumping to conclusions
B.C.’s controversial safer supply policies provide drug users with prescription opioids as an alternative to toxic street drugs. Its decriminalization policy permitted drug users to possess otherwise illegal substances for personal use.
The peer-reviewed study was led by health economist Hai Nguyen and conducted by researchers from Memorial University in Newfoundland, the University of Manitoba and Weill Cornell Medicine, a medical school in New York City. It was published in the medical journal JAMA Health Forum on March 21.
The researchers used a statistical method to create a “synthetic” comparison group, since there is no ideal control group. The researchers then compared B.C. to other provinces to assess the impact of certain drug policies.
Examining data from 2016 to 2023, the study links B.C.’s safer supply policies to a 33 per cent rise in opioid hospitalizations.
The study says the province’s decriminalization policies further drove up hospitalizations by 58 per cent.
“Neither the safer supply policy nor the subsequent decriminalization of drug possession appeared to alleviate the opioid crisis,” the study concludes. “Instead, both were associated with an increase in opioid overdose hospitalizations.”
The B.C. government rolled back decriminalization in April 2024 in response to widespread concerns over public drug use. This February, the province also officially acknowledged that diversion of safer supply drugs does occur.
The study did not conclusively determine whether the increase in hospital visits was due to diverted safer supply opioids, the toxic illicit supply, or other factors.
“There was insufficient evidence to conclusively attribute an increase in opioid overdose deaths to these policy changes,” the study says.
Nguyen’s team had published an earlier, 2024 study in JAMA Internal Medicine that also linked safer supply to increased hospitalizations. However, it failed to control for key confounders such as employment rates and naloxone access. Their 2025 study better accounts for these variables using the synthetic comparison group method.
The study’s authors did not respond to Canadian Affairs’ requests for comment.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Correlation vs. causation
Chris Perlman, a health data and addiction expert at the University of Waterloo, says more studies are needed.
He believes the findings are weak, as they show correlation but not causation.
“The study provides a small signal that the rates of hospitalization have changed, but I wouldn’t conclude that it can be solely attributed to the safer supply and decrim[inalization] policy decisions,” said Perlman.
He also noted the rise in hospitalizations doesn’t necessarily mean more overdoses. Rather, more people may be reaching hospitals in time for treatment.
“Given that the [overdose] rate may have gone down, I wonder if we’re simply seeing an effect where more persons survive an overdose and actually receive treatment in hospital where they would have died in the pre-policy time period,” he said.
The Nguyen study acknowledges this possibility.
“The observed increase in opioid hospitalizations, without a corresponding increase in opioid deaths, may reflect greater willingness to seek medical assistance because decriminalization could reduce the stigma associated with drug use,” it says.
“However, it is also possible that reduced stigma and removal of criminal penalties facilitated the diversion of safer opioids, contributing to increased hospitalizations.”
Karen Urbanoski, an associate professor in the Public Health and Social Policy department at the University of Victoria, is more critical.
“The [study’s] findings do not warrant the conclusion that these policies are causally associated with increased hospitalization or overdose,” said Urbanoski, who also holds the Canada Research Chair in Substance Use, Addictions and Health Services.
Her team published a study in November 2023 that measured safer supply’s impact on mortality and acute care visits. It found safer supply opioids did reduce overdose deaths.
Critics, however, raised concerns that her study misrepresented its underlying data and showed no statistically significant reduction in deaths after accounting for confounding factors.
The Nguyen study differs from Urbanoski’s. While Urbanoski’s team focused on individual-level outcomes, the Nguyen study analyzed broader, population-level effects, including diversion.
Wallace, the biostatistician, agrees more individual-level data could strengthen analysis, but does not believe it undermines the study’s conclusions. Wallace thinks the researchers did their best with the available data they had.
“We do not have a ‘copy’ of B.C. where the policies weren’t implemented to compare with,” said Wallace.
B.C.’s overdose rate of 775 per 100,000 is well above the national average of 533.
Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, has been a vocal critic of B.C.’s decriminalization and safer supply policies.
“If the government doesn’t want to believe this study, well then I invite them to do a similar study,” she told reporters on March 27.
“Show us the evidence that they have failed to show us since 2020,” she added, referring to the year B.C. implemented safer supply.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Our content is always free – but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
-

 2025 Federal Election16 hours ago
2025 Federal Election16 hours agoThe Federal Brief That Should Sink Carney
-
 2025 Federal Election18 hours ago
2025 Federal Election18 hours agoHow Canada’s Mainstream Media Lost the Public Trust
-

 2025 Federal Election21 hours ago
2025 Federal Election21 hours agoOttawa Confirms China interfering with 2025 federal election: Beijing Seeks to Block Joe Tay’s Election
-
 2025 Federal Election20 hours ago
2025 Federal Election20 hours agoReal Homes vs. Modular Shoeboxes: The Housing Battle Between Poilievre and Carney
-
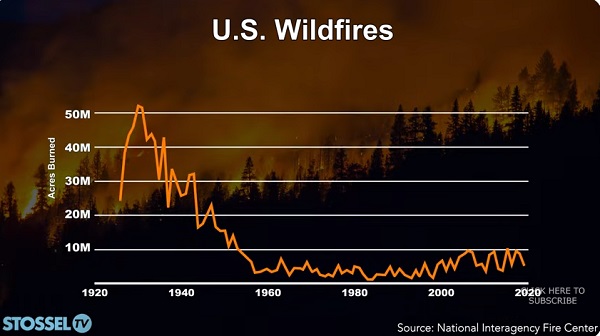
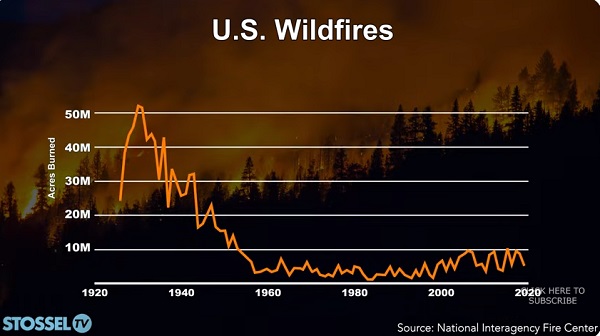 John Stossel17 hours ago
John Stossel17 hours agoClimate Change Myths Part 2: Wildfires, Drought, Rising Sea Level, and Coral Reefs
-

 COVID-1919 hours ago
COVID-1919 hours agoNearly Half of “COVID-19 Deaths” Were Not Due to COVID-19 – Scientific Reports Journal
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoPoilievre Campaigning To Build A Canadian Economic Fortress
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoThe Cost of Underselling Canadian Oil and Gas to the USA



