MAiD
Skiing down euthanasia’s slippery slope

From the Macdonald Laurier Institute
By John Keown
Canada is on track to surpass the Netherlands.
When the Canadian Parliament legalized voluntary euthanasia (VE) and physician-assisted suicide (PAS) in 2016, at the behest of the Supreme Court, supporters of legalization doubtless hoped the new law and its operation would prove something of a poster child for the compassionate and controlled medical ending of life. Its critics, however, might now describe it as less like a poster child and more like the picture of Dorian Gray.
Whether the law should permit VE and PAS is one of the most important questions of social policy in developed countries. Here we will eschew the tendentious and misleading euphemisms “assisted dying” and “medical assistance in dying.” The law and professional medical ethics have always allowed doctors and nurses to “help people to die” by palliating symptoms, even if so doing foreseeably shortens life. What the new law permits is radically different: the intentional killing of patients and intentionally assisting them to kill themselves.
Moreover, the euthanasia law does not require that patients be “dying” or “terminally ill” in order (to employ further euphemisms) to be given the “medication” for such “treatment.” Policy makers should not disguise, or be complicit in disguising, the foundational nature of this moral, legal, medical, and social paradigm shift.
The Canadian experience with VE and PAS is of major relevance to the international debate. Does it support the assurances of legalization campaigners that these practices can be effectively controlled by the law and provide a “last resort” in the sort of “hard cases” involving patients who are (or who fear) dying in severe pain or discomfort – patients who are so regularly paraded before us by the mass media?
Or does it support the counter-argument that the appropriate answer to such pain and discomfort is the wider availability of quality palliative care, and that a relaxed law would not only fail to prevent mistake or abuse but would also prove a first step on a precipitous “slippery slope” to VE and PAS in an ever-widening range of cases?
The best body of evidence concerning the effects of legalization comes from the Netherlands, whose experience I have studied for 35 years.
The Dutch Supreme Court declared VE and PAS lawful in 1984. To justify this change, the Dutch invoked the doctor’s duty to relieve suffering, and the focus of discussion was the physical suffering of the dying. However, in 1994 the same court held that the requirement of “unbearable suffering” could be satisfied by an illness that was neither terminal nor even physical and was solely mental. (Whether the patient’s suffering was “unbearable” remains very largely a subjective matter decided by the patient.)
In 2016 the Dutch government proposed a further legal extension: to elderly folk with a “completed” life. And, if some patients still do not manage to meet the lax legal criteria for VE and PAS their doctors can, and do, advise them that there is the option of being medically palliated while they dehydrate themselves to death.
Lethal injections have even been extended to patients who are incapable of making a request. In 1996 the Dutch courts declared it lawful intentionally to kill disabled infants, such as those with spina bifida. And only last year, the government announced that euthanasia would be allowed for children between one and 12. In short, over the past 40 years the Dutch have clearly tumbled down euthanasia’s slippery slope. Their Belgian neighbours, who followed them in 2002 (the same year that Dutch legislation enshrining the pre-existing legal criteria came into force) are also on the skids.
Why does this happen? There are two explanations, one empirical, the other logical. The empirical explanation is that relaxed laws cannot effectively control VE and PAS in practice because the challenges of formulating, drafting, and enforcing proper safeguards are intractable. Common media references to “strict safeguards” in places like the Netherlands and Canada reflect journalistic ignorance rather than social reality.
The second explanation is logical. VE and PAS are, campaigners tell us, justified by (i) respect for patient autonomy and (ii) by the duty to relieve suffering. But if one buys their argument, euthanasia is also justified for competent patients who are suffering from chronic, not merely terminal, illness, and whether their suffering is physical or mental. Suffering is suffering, whether from terminal cancer or chronic arthritis or depression. Indeed, suffering from chronic illness, physical or mental, may last a lifetime, not merely a few weeks or months. And why exclude the perduring existential suffering that tragically blights the lives of so many lonely, elderly folk?
Why, moreover, exclude euthanasia for suffering patients such as infants who are incapable of requesting death (non-voluntary euthanasia or NVE)? The absence of patient autonomy does not cancel the doctor’s duty of beneficence.
The Dutch have, then, proved nothing if not logical, and it is surely only a matter of time until their law is formally extended to embrace the elderly who are “tired of life.”
And so, to Canada. It leaped onto the slope as a result of the Supreme Court’s ruling in Carter v. Canada in 2015, in which the court overruled its previous decision in Rodriguez v. British Columbia in 1993. Rodriguez was soundly reasoned, and its reasoning remains in line with the rejection of a right to VE and PAS by the highest courts in other common law jurisdictions including the United States, the United Kingdom, and Ireland. By contrast (as I explain in Euthanasia, Ethics and Public Policy), Carter may strike some as reading more like rationalization than reasoning and as an exercise in judicial activism that stains Canadian jurisprudence.
Here we will mention just one of its flaws: its endorsement of the crucial finding of the trial judge that the evidence from jurisdictions with VE and/or PAS showed that the risks of legalization can be very largely avoided by carefully designed, well-monitored safeguards. This finding bristled with problems, not least of which was that no jurisdiction had (or has) carefully designed, well-monitored safeguards.
In a subsequent and similar case in Ireland, three senior judges carefully reviewed the judgment of the trial judge in Carter. They unanimously rejected her finding, not least in view of the (undisputed) evidence from the Netherlands and Belgium of the striking extent of medical euthanasia without any explicit request from the patient.
I was called as an expert witness in Carter by the Attorney General of Canada. At the end of my day-long cross-examination in Vancouver by the late Joseph Arvay, Q.C., counsel for those challenging the law against VE and PAS, the judge asked me to reprise both the practical and logical slippery slope arguments that I have outlined above. I did so, using the evidence from the Netherlands, Belgium, and Oregon to demonstrate the lack of effective legal control, and the Dutch endorsement of infanticide to illustrate the logical slippery slope. (Indeed, the two leading ethics experts called by Mr Arvay had endorsed both voluntary and non-voluntary euthanasia in their published work.)
The judge nevertheless concluded that the evidence showed that VE and PAS could safely be legalized. As for the logical argument, she dismissed it as involving “speculation” and because the legal challenge was only to the legal prohibition as it affected competent patients! Her failure to join the dots was noteworthy. (My 2022 paper in the Cambridge Law Journal confirms the real, not speculative, nature of the logical argument.) The Supreme Court endorsed the judge’s several errors. It did so, moreover, without even the fig leaf of a single dissenting judgment.
And what have we (all too predictably) witnessed since 2016, when legislation accommodated the Supreme Court’s ruling? Even leaving aside the steep yearly increases in the number of medical killings, we have seen that the statutory requirement that the patient’s death be “reasonably foreseeable” need no longer be met; that euthanasia where the sole cause of suffering is mental illness has been approved (though its implementation has been delayed until 2027 to allow preparations to be made), and that further expansion of the law to include “mature” minors, and requests for euthanasia written in advance of incompetence, is on the cards. Not to mention the several reported cases involving vulnerable patients that raise unsettling questions about the operation of the law.
In 1994 a distinguished House of Lords Select Committee on Medical Ethics unanimously concluded that English law should not permit VE or PAS. The committee observed that the criminal law’s prohibition on intentional killing was the “cornerstone of law and of social relationships” that “protects each one of us impartially, embodying the belief that all are equal.”
The experience in Canada uncomfortably confirms what happens once a society abandons that historic, bright-line prohibition in favour of the competing and arbitrary notion that whereas some people have lives that are “worth living,” others would be “better off dead” and it is right to grant their request to be killed or to help them kill themselves.
It is surely only a matter of time until calls are made for the “benefit” of a hastened death to be conferred on people who are incapable of requesting it. Why “discriminate” against people who are suffering with, say, advanced dementia merely because they are incapable of requesting a lethal injection? Why deny them their rights under the Canadian Charter of Rights and Freedoms? The enormous cost savings will lurk supportively behind the argument, like a gangster’s heavy.
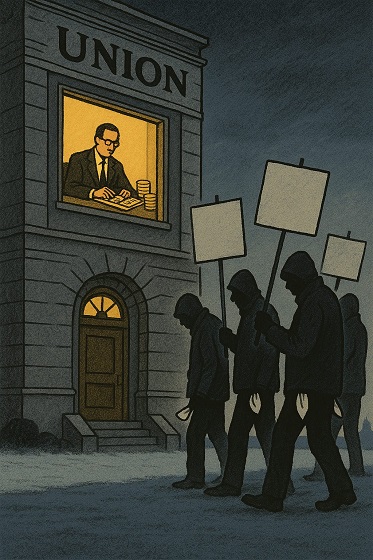
In the Netherlands, euthanasia has been normalized to a significant degree. Far from being an exceptional practice in “hard cases” of “last resort,” it has come to be regarded largely as another healthcare option. Canada appears to be following suit. Professor Trudo Lemmens, the eminent Canadian health lawyer, has noted the “troubling normalization” of euthanasia in Canada where, he adds, “rights rhetoric” surrounding the issue has replaced evidence-based debate.
Thankfully, the concerning developments in Canada are now being ventilated in the public domain: in the media, both in Canada and abroad; in journals of law, medicine and bioethics, and by the UN rapporteur on the rights of people with disabilities. It is telling that in the UK even campaigners for legalization are straining to distance themselves from the Canadian precedent.
In 40 years, the Dutch have slid down the slippery slope. In fewer than 10, Canada appears to be veritably skiing.
John Keown DCL (Oxon) is the Rose F. Kennedy Professor of Christian Ethics in the Kennedy Institute of Ethics at Georgetown University in Washington, DC. He previously taught medical law at the University of Cambridge. The second edition of his book Euthanasia, Ethics and Public Policy: An Argument Against Legalisation, described as “magisterial” by Lord Judge, the former Lord Chief Justice of England and Wales, was published by Cambridge University Press in 2018.
Great Reset
EXCLUSIVE: The Nova Scotia RCMP Veterans’ Association IS TARGETING VETERANS with Euthanasia

I just received an email from a retired member of the RCMP…
“I served for 32 years on the West Coast and retired in 2019. As a Christian and a retired member of the RCMP I wanted to share this with you. I’m trying to wrap my head around this shocking email. I’m shocked it’s come to this.” – L.K
SATURDAY, NOV. 22, 2025
1:30-3:00 PM CHURCH HALL, OLD SACKVILLE ROAD, MIDDLE SACVILLE, NS, B4E 1R3.
On November 20th, an email quietly dropped into the inboxes of Nova Scotia RCMP veterans. Standard, polite and in true Canadian fashion formal and sanitized. This was no mistake, this wasn’t information. This was something different.
This was grooming.
Yes I said it, coercion.
The “opportunity” was a “Medical Assistance in Dying (MAID) Program in Nova Scotia”
This is a state-aligned institutions normalizing death as a service to the very people they already failed to support in life .This was a information session, to “educate” veterans who’s rates of PTSD and suicidality were already sky hight. How they can apply or use MAID.
The invited speaker?
Dr. Gordon Gubitz
Location? None other than a place of worship, a church hall. The target audience?
VETERANS.
This is what I’ve been talking about, welcome to the soft-coercive stage of Canada’s MAID regime.
Let’s meet Dr. Gordon Gubitz. The same Dr. Gubitz whois a MAID assessor and provider (killer) is the Clinical Lead for MAID in Nova Scotia, which means MAID is his not only his passion but spends his work focused on ending lives. This “Dr” sits on the board of CAMAP, the pro death organization that creates all the pathways for Canadians to be killed while manipulating the court systems in their favour. More death to them is the goal. This “Dr” helped write the national MAID curriculum and trains doctors on how to present MAID as a “care option.” This guy is literally a death pusher and peddler of the dark.
Think of him a the drug dealer for death.
They didn’t invite a trauma specialist.
They didn’t invite a palliative expert.
They didn’t invite a police mental-health advocate.
They didn’t invite a mental health expert
They didn’t invite a Dr who looks at psychedelic assisted therapy
They didn’t invite hope. They only invited death.
Kelsi Sheren is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Nova Scotia RCMP veterans invited a man whose job is to facilitate, provide and promote nothing but death, and whose organization teaches clinicians how to introduce MAID (assisted SUICIDE) to patients who didn’t ask for it, bring it up or want it in their life.
Let me explain something, If you’re a veteran dealing with PTSD, chronic pain, TBI, disability, or bureaucracy-induced despair, this isn’t “education.”
This is targeted psychological pressure.
Coercion, CAMAP and Dying with Dignity’s claim to fame.
No one will say the words out loud. No one will write “we think some of you should consider dying.”
They don’t need to, when just dangling the carrot is good enough to get the job done.
Coercion today is subtle, normalized in the community. It’s dressed up like Christmas cookies in a church call, framed as loving “support” being held by one of the most prolific death pushers in the game.
Simply funnelling veterans into the system one “information session” at a time. Like cattle through the gates of hell, with CAMAP waiting in the shadows. This time not with a bold gun. They would see that as “too humane”, but with a pen, check list, a needle and a paralytic.
Canada already proved it’s willing to dangle MAID (assisted suicide, murder, early death) in front of struggling veterans. I helped break these stories and bring our veterans stories to the masses. I’m interviewing more by the day, who’ve been offered death over life illegally.
VAC employees got caught offering MAID to veterans who never asked for it, including one trying to get a wheelchair ramp, my friend Christine.
So do me a favour spare us the “this is innocent” act.
Veterans have been coerced before, and it’s happening again right in front of your faces. Now the RCMP Veterans’ Association is rolling out the red carpet for the prevailers of death. The dark ones who feed on the souls of those who couldn’t bare to take another breath.
This is not an “opportunity.”
This is a sales pitch.
And the product is your death.
People keep asking me why veterans are being targeting? Because they’re the perfect targets, don’t you see?
Kelsi Sheren is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Veterans, on the daily are dealing with chronic pain, combat trauma, moral injury, sanctuary trauma, disability, suicidality, lack of services, financial strain, bureaucratic obstruction and the government doesn’t just know know it, it caused it and it supports it and so do the MAID, pro death cult architects.
The MAID lobby knows veterans are “high-yield” candidates, and not because they want to die, but because the system has already worn them down, like water slowly dripping over the rocks. The Liberal government just cut OVER 4 BILLION in care for veterans. Veterans aren’t being shown the full picture, they aren’t given any hope. They’re being shown the early exit. What we call in some circles, being shown the path to “self-selection.”
This RCMP veterans email is a soft-touch version of coercion if I’ve ever seen one.
“We’re not telling you to choose MAID… we’re just putting the idea on the table, in a friendly community space, with a trusted expert who helps design the national MAID system.” Who’s job is to provide you with all the pathways to wanting to kill yourself.
That’s how you manipulate a vulnerable population without leaving fingerprints.
Dr. Gubitz isn’t neutral. He is the system.
Gubitz isn’t walking into that church as an independent medical educator.
He is walking in as the clinical gatekeeper for MAID in Nova Scotia, IE. HELL. He’s nothing more than one of the ideological engines behind national MAID training. A CAMAP insider, the organization pushing to expand and normalize MAID (assisted SUICIDE) at every level of “healthcare,” if you can even call it that anymore. CAMAP literally publishes guidance on how clinicians should bring up MAID as a care option. Not reactively. Proactively.
When you pair a vulnerable group with a man trained to present MAID as “equitable access,” your “information session” becomes a recruitment funnel.
HOW IS EVERYONE OK WITH THIS?
You are directly influencing and priming veterans for death under the banner of “support.” It’s an illusion, it’s predatory behaviour! It’s not informed consent in any way. It’s manipulation.
And holding it in a church? That’s strategic psychological laundering.
Churches are trusted spaces. They lower defences, help you to open your mind. Churches to most signal moral legitimacy so hosting a MAID talk in a church hall tells veterans “your community approves. Your faith approves this is acceptable, this is dignified, you don’t have to fight or feel guilty, ”
It cloaks a controversial, ethically fraught practice in community warmth. It’s taking advantage of the safety and sanctity of church.
That’s not an accident.
It’s a tactic.
This wreaks of propaganda wrapped in hospitality.
This is the playbook of a system that wants to solve suffering by eliminating the sufferer.
Canada won’t fix the care gaps. It won’t fix the mental-health crisis. It won’t fix VAC’s failures and it sure as hell won’t fix disability supports.
But it will happily fund a national MAID curriculum, expand eligibility, remove guardrails, and now apparently send MAID providers on a tour of vulnerable communities.
Veterans have always been canaries in Canada’s moral coal mine.
If the state can normalize MAID to the people who wore its uniform, it can normalize it to anyone. And that’s the point.
This story isn’t about one email. It’s about a culture shift engineered from the top down.
This is how you create acceptance – – >
First, make MAID look compassionate.
Then, bring it into community spaces.
Then, present to vulnerable groups.
Then, call it “support.”
Then, remove the stigma.
Then, remove the safeguards.
Then, expand eligibility.
Then, tell the public: “People are choosing MAID because it’s dignified.”
They leave out the part where the system helped manufacture despair.
Veterans deserve better than an invitation to die.
They deserve care, treatment, advocacy, and someone who doesn’t treat their suffering as a problem to be erased.
Not a church basement with coffee and a state-aligned MAID architect explaining their “options.”
This email isn’t benign.
It is a warning, one Canada should have heeded years ago.
If the country is comfortable offering death to the people who served it, it’s comfortable offering it to anyone.
And that’s exactly what’s happening.
Please feel free to call or email them and let them know how this makes you feel.
KELSI SHEREN
– – – – – – – – – – – – –
One Time Donation! – Paypal – https://paypal.me/
Buy me a coffee! – https://buymeacoffee.com/
Youtube – https://www.youtube.com/@
Substack: https://substack.com/@
TikTok – https://x.com/KelsiBurns
Listen on Spotify:
|
|
The Kelsi Sheren Perspective
Kelsi Sheren Podcast |
SUPPORT OUR SPONSORS
– – – – – – – – – – – –
Ketone IQ- 30% off with code KELSI – https://ketone.com/KELSI
Good Livin – 20% off with code KELSI – https://www.itsgoodlivin.com/?
Brass & Unity – 20% off with code UNITY – http://brassandunity.com
Kelsi Sheren is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Health
Disabled Canadians petition Parliament to reverse MAiD for non-terminal conditions

From LifeSiteNews
Canadians with disabilities have demanded that legislators stop treating their lives as ‘dispensable’ by banning non-terminal ‘Track 2’ assisted suicide.
Conservative Member of Parliament Garnett Genuis has presented a petition from Canadians with disabilities warning against euthanasia expansion.
During a November 19 session in the House of Commons, Genuis delivered a petition to end Track 2 Medical Assistance in Dying (MAiD) request, which allow doctors to end the lives of those who are not terminally ill but have lost the will to live due to their having chronic health problems.
“The petitioners state that it is unacceptable for Canadians to choose medical assistance in dying due to a lack of available services or treatments,” Genuis told the House of Commons. “This is not a real choice. They point out that allowing MAiD for people with disabilities or chronic non-terminal illnesses devalues their lives. It sends the dangerous message that life with a disability is optional.”
People with Disabilities are Speaking Out On Euthanasia/MAiD
So-called “Track 2 MAiD” has transformed the experience of people with disabilities when accessing the healthcare system.
These petitioners want it reversed. pic.twitter.com/n3izpAQI2T
— Garnett Genuis (@GarnettGenuis) November 17, 2025
Genuis cited a recent article in Le Soleil which recounted the troubling case of a sick Canadian man who was essentially encouraged by a social worker to stop fighting and opt for death by lethal injection.
“That is not compassion. It is a betrayal of our duty to protect human dignity,” he declared.
The petition pointed out that “allowing medical assistance in dying for those with disabilities or chronic illness who are not dying devalues their lives, tacitly endorsing the notion that life with disability is optional, and by extension, dispensable.”
It also pointed out that making MAiD available to individuals with disabilities or chronic illnesses diminishes the motivation to develop better treatments and provide higher quality care for those living with such conditions.
In conclusion, the petition called on the Canadian government to “protect all Canadians whose natural death is not reasonably foreseeable by prohibiting medical assistance in dying for those whose prognosis for natural death is more than six months.”
A few days earlier, on November 17, Liberals responded to the petition by claiming that they have implemented “safeguards” to assess if someone is eligible to receive MAiD.
“These safeguards aim to address the risks associated with diverse sources of suffering and vulnerability, that could lead someone not close to death to seek MAiD,” Liberals wrote. “The safeguards examine whether their suffering results from factors other than the medical condition and whether there are ways of addressing their suffering other than through MAiD.”
However, this is not the first time that Canadians have petitioned to protect vulnerable Canadians from the ever-growing euthanasia regime.
As LifeSiteNews reported in October, Inclusion Canada CEO Krista Carr told Parliament that many disabled Canadians are being pressured to end their lives with euthanasia during routine medical appointments.
Similarly, internal documents from Ontario doctors in 2024 that revealed Canadians are choosing euthanasia because of poverty and loneliness, not as a result of an alleged terminal illness.
In one case, an Ontario doctor revealed that a middle-aged worker, whose ankle and back injuries had left him unable to work, felt that the government’s insufficient support was “leaving (him) with no choice but to pursue” euthanasia.
Other cases included an obese woman who described herself as a “useless body taking up space,” which one doctor argued met the requirements for assisted suicide because obesity is “a medical condition which is indeed grievous and irremediable.”
At the same time, the Liberal government has worked to expand euthanasia 13-fold since it was legalized, making it the fastest growing euthanasia program in the world.
Currently, wait times to receive actual health care in Canada have increased to an average of 27.7 weeks, leading some Canadians to despair and opt for euthanasia instead of waiting for assistance. At the same time, sick and elderly Canadians who have refused to end their lives have reported being called “selfish” by their providers.
The most recent reports show that euthanasia is the sixth highest cause of death in Canada; however, it was not listed as such in Statistics Canada’s top 10 leading causes of death from 2019 to 2022.
Asked why it was left off the list, the agency said that it records the illnesses that led Canadians to choose to end their lives via euthanasia, not the actual cause of death, as the primary cause of death.
According to Health Canada, 13,241 Canadians died by euthanasia lethal injections in 2022, accounting for 4.1 percent of all deaths in the country that year, a 31.2 percent increase from 2021.
-

 Energy2 days ago
Energy2 days agoCarney bets on LNG, Alberta doubles down on oil
-

 Alberta2 days ago
Alberta2 days agoAlberta on right path to better health care
-

 Indigenous2 days ago
Indigenous2 days agoTop constitutional lawyer slams Indigenous land ruling as threat to Canadian property rights
-

 Alberta2 days ago
Alberta2 days agoAlberta Emergency Alert test – Wednesday at 1:55 PM
-

 Alberta2 days ago
Alberta2 days agoCarney government’s anti-oil sentiment no longer in doubt
-
 Alberta1 day ago
Alberta1 day ago‘Weird and wonderful’ wells are boosting oil production in Alberta and Saskatchewan
-

 Health2 days ago
Health2 days agoSPARC Kindness Tree: A Growing Tradition in Capstone
-

 Business1 day ago
Business1 day agoCanada is failing dismally at our climate goals. We’re also ruining our economy.