Alberta
Healthcare Overhaul – Services to be provided by nurses in their own clinics

Strengthening primary care with nurse practitioners
Alberta’s government is expanding opportunities for nurse practitioners to give Albertans greater access to a regular primary care provider when and where they need one.
Too many Albertans cannot find a regular family doctor or have trouble getting an appointment with the one they have. Alberta’s government continues to support and stabilize primary health care across the province by enabling nurse practitioners to open their own clinics, take on patients and offer services based on their scope of practice, training and expertise. Typically nurse practitioners can provide about 80 per cent of the medical services a family physician provides, and this will be reflected in the compensation model when it’s finalized.
Nurse practitioners have completed graduate studies and are regulated by the College of Registered Nurses of Alberta. Like other regulated professions, all nurse practitioners must meet minimum requirements to practise and follow standards set by their regulatory college.
“Nurse practitioners are highly trained and valued medical professionals. By enabling them to open their own clinics, we are ensuring Albertans can more easily access the care they need. This is a significant improvement in our primary health care system that will benefit patients and help improve the overall health and health outcomes of Alberta families.”
As the province enables nurse practitioners to do more of the work they are trained to do, a new compensation model will be created to encourage them to operate independently, adding much-needed capacity to Alberta’s primary care system. Nurse practitioners are extensively trained in their graduate studies to assess, diagnose, treat, order and interpret diagnostic tests, prescribe medications, make referrals to a specialist and manage a person’s overall care.
In addition, through a $2-million grant over the next three years, the Nurse Practitioner Association of Alberta will help to implement a compensation model, recruit other nurse practitioners to participate and provide supports as they work to set up their own clinics.
“There is no doubt about it, we need more health professionals providing primary health care to Albertans. Nurse practitioners are skilled health care professionals who play vital roles in modern health care. This model has the potential to add capacity in communities across the province and help so many Albertans gain access to a regular primary care provider.”
The new compensation model will be phased in and is expected to launch in early 2024 when nurse practitioners who want to go into independent practice will be asked to submit expressions of interest. The model is expected to include payment for a specified number of clinical hours and other commitments, such as caring for a certain number of patients.
“The Nurse Practitioner Association of Alberta is thrilled for the opportunity to support Albertans across the province in accessing a care provider in all health care environments, not just primary care. With this announcement and this grant, the association will be perfectly positioned to ensure that our members will be fully prepared to meet the needs of Albertans in both urban and rural communities. Until now, accessing a nurse practitioner has been challenging. This announcement ends those challenges. The NPAA looks forward to working with Alberta Health to get clinics open and to support NPs in being able to do the work that they are trained to do.”
Nurse practitioners who opt into the compensation model will also qualify for caseload supports once their patient caseloads are established, as announced on Oct. 18. The three-year $57-million support program will help primary health care providers manage an increasing number of patients. Each provider has the potential to receive up to $10,000 annually.
“The shortage of health care professionals in rural communities has always been a challenge that required innovative solutions. The new nurse practitioner model actively addresses this need by enhancing and expanding rural health care deliveries. This new initiative will enable rural Albertans to have better access to primary health care close to home.”
Alberta’s government will continue working with the Nurse Practitioner Association of Alberta and the College of Registered Nurses of Alberta as the compensation model is implemented.
Related information
Related news
- Strengthening health care: Improving access for all (Oct 18, 2023)
Alberta
Alberta takes big step towards shorter wait times and higher quality health care

From the Fraser Institute
On Monday, the Smith government announced that beginning next year it will change the way it funds surgeries in Alberta. This is a big step towards unlocking the ability of Alberta’s health-care system to provide more, better and faster services for the same or possibly fewer dollars.
To understand the significance of this change, you must understand the consequences of the current (and outdated) approach.
Currently, the Alberta government pays a lump sum of money to hospitals each year. Consequently, hospitals perceive patients as a drain on their budgets. From the hospital’s perspective, there’s little financial incentive to serve more patients, operate more efficiently and provide superior quality services.
Consider what would happen if your local grocery store received a giant bag of money each year to feed people. The number of items would quickly decline to whatever was most convenient for the store to provide. (Have a favourite cereal? Too bad.) Store hours would become less convenient for customers, alongside a general decline in overall service. This type of grocery store, like an Alberta hospital, is actually financially better off (that is, it saves money) if you go elsewhere.
The Smith government plans to flip this entire system on its head, to the benefit of patients and taxpayers. Instead of handing out bags of money each year to providers, the new system—known as “activity-based funding”—will pay health-care providers for each patient they treat, based on the patient’s particular condition and important factors that may add complexity or cost to their care.
This turns patients from a drain on budgets into a source of additional revenue. The result, as has been demonstrated in other universal health-care systems worldwide, is more services delivered using existing health-care infrastructure, lower wait times, improved quality of care, improved access to medical technologies, and less waste.
In other words, Albertans will receive far better value from their health-care system, which is currently among the most expensive in the world. And relief can’t come soon enough—for example, last year in Alberta the median wait time for orthopedic surgeries including hip and knee replacements was 66.8 weeks.
The naysayers argue this approach will undermine the province’s universal system and hurt patients. But by allowing a spectrum of providers to compete for the delivery of quality care, Alberta will follow the lead of other more successful universal health-care systems in countries such as Australia, Germany, the Netherlands and Switzerland and create greater accountability for hospitals and other health-care providers. Taxpayers will get a much better picture of what they’re paying for and how much they pay.
Again, Alberta is not exploring an untested policy. Almost every other developed country with universal health care uses some form of “activity-based funding” for hospital and surgical care. And remember, we already spend more on health care than our counterparts in nearly all of these countries yet endure longer wait times and poorer access to services generally, in part because of how we pay for surgical care.
While the devil is always in the details, and while it’s still possible for the Alberta government to get this wrong, Monday’s announcement is a big step in the right direction. A funding model that puts patients first will get Albertans more of the high-quality health care they already pay for in a timelier fashion. And provide to other provinces an example of bold health-care reform.
Alberta
Alberta’s embrace of activity-based funding is great news for patients

 From the Montreal Economic Institute
From the Montreal Economic Institute
Alberta’s move to fund acute care services through activity-based funding follows best practices internationally, points out an MEI researcher following an announcement made by Premier Danielle Smith earlier today.
“For too long, the way hospitals were funded in Alberta incentivized treating fewer patients, contributing to our long wait times,” explains Krystle Wittevrongel, director of research at the MEI. “International experience has shown that, with the proper funding models in place, health systems become more efficient to the benefit of patients.”
Currently, Alberta’s hospitals are financed under a system called “global budgeting.” This involves allocating a pre-set amount of funding to pay for a specific number of services based on previous years’ budgets.
Under the government’s newly proposed funding system, hospitals receive a fixed payment for each treatment delivered.
An Economic Note published by the MEI last year showed that Quebec’s gradual adoption of activity-based funding led to higher productivity and lower costs in the province’s health system.
Notably, the province observed that the per-procedure cost of MRIs fell by four per cent as the number of procedures performed increased by 22 per cent.
In the radiology and oncology sector, it observed productivity increases of 26 per cent while procedure costs decreased by seven per cent.
“Being able to perform more surgeries, at lower costs, and within shorter timelines is exactly what Alberta’s patients need, and Premier Smith understands that,” continued Mrs. Wittevrongel. “Today’s announcement is a good first step, and we look forward to seeing a successful roll-out once appropriate funding levels per procedure are set.”
The governments expects to roll-out this new funding model for select procedures starting in 2026.
* * *
The MEI is an independent public policy think tank with offices in Montreal, Ottawa, and Calgary. Through its publications, media appearances, and advisory services to policymakers, the MEI stimulates public policy debate and reforms based on sound economics and entrepreneurship.
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoHarper Endorses Poilievre at Historic Edmonton Rally: “This Crisis Was Made in Canada”
-
 2025 Federal Election2 days ago
2025 Federal Election2 days agoMark Carney’s radical left-wing, globalist record proves he is Justin Trudeau 2.0
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoAn In-Depth Campaign Trail “Interview” With Pierre Poilievre
-
 conflict2 days ago
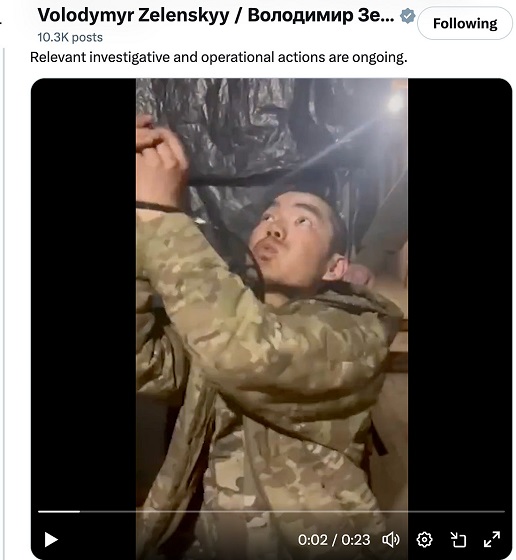
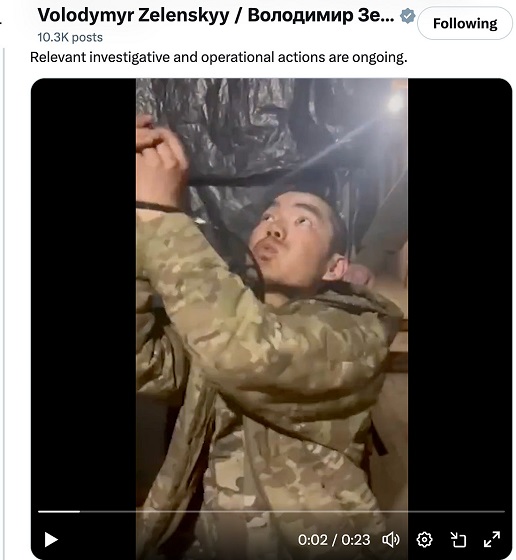
conflict2 days agoZelensky Alleges Chinese Nationals Fighting for Russia, Calls for Global Response
-

 Business2 days ago
Business2 days agoTrump’s tariff plan replaces free trade with balanced trade. Globalists hate that.
-

 2025 Federal Election17 hours ago
2025 Federal Election17 hours agoConservative Party urges investigation into Carney plan to spend $1 billion on heat pumps
-

 Censorship Industrial Complex2 days ago
Censorship Industrial Complex2 days agoScott Atlas: COVID lockdowns, censorship have left a ‘permanent black mark on America’
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoDon’t double-down on net zero again