Brownstone Institute
Eye Protection Wasn’t Misdirection
From the Brownstone Institute
BY
“If you have goggles or an eye shield, you should use it.” ~ Anthony Fauci, July 30th, 2020
We had heard enough from Fauci by the time this comment was made in mid-2020 to begin automatically tuning out his frequently contradictory advice. What if we had given weight to this comment and explored why he began recommending goggles (yet never donned them himself)?
While I’m not surprised that the inner anatomy of the face including ocular ducts and connectivity within structures aren’t common knowledge, I expected more of a reaction from the medical community regarding Fauci’s push for eye protection. Not only do medical professionals take extensive coursework on human anatomy — they are required to meet annually with an Industrial Hygienist for fit tested, hazard-specific kit for each exposure setting , including ocular protection. This testing process requires going into detail about each exposure setting and required donning and donning practices within the scope of their professional duties.
Instead of elaborating on his recommendation, Fauci just publicly hushed on the issue and folks carried on, obediently masked up yet entirely neglectful of their nasolacrimal ducts. Shame, shame.

These are the structures of the lacrimal apparatus connecting ocular and nasal pathways. Basically, the eye drains into the nasal cavity. None of the talking heads of the medical community ever seem to bring up that these parts of the body connect with one another, and while we hear about masks ad nauseam three entire years after the onset of the SARS-CoV-2 pandemic, no one is arguing with strangers on the internet about goggles.
Bernie Sanders was recently praised for being the only person at the February, 2023 State of the Union donning a (sub-grade, non-mitigating) respirator, but eye spy something fishy. It was noted that he kept removing his glasses, as they were fogging up.

Those who have donned respirators have experienced that exhale emissions are generally redirected out of the nose bridge (or out of side gaps if improperly sealed). This is the exhale emission plume create by a fitted, unvalved N95 respirator:

This plume of warm, moist respiratory emissions is what causes glasses to fog. This is precisely why I continue to argue that masks are NOT source control for respiratory aerosols, because these apparatuses are not designed nor intended to protect others from your emissions, but solely for protection of the wearer. The ASTM agrees with me on this matter:
The American Society for Testing and Materials (ASTM) Standard Specification for Barrier Face Coverings F3502-21 Note 2 states, “There are currently no established methods for measuring outward leakage from a barrier face covering, medical mask, or respirator. Nothing in this standard addresses or implies a quantitative assessment of outward leakage and no claims can be made about the degree to which a barrier face covering reduces emission of human-generated particles.”
Additionally, Note 5 states, “There are currently no specific accepted techniques that are available to measure outward leakage from a barrier face covering or other products. Thus, no claims may be made with respect to the degree of source control offered by the barrier face covering based on the leakage assessment.”
So does it matter if your neighbor’s exhale emissions are directed in your face for the duration of your 6-hour flight?

Absolutely. Imagine sitting between these two fine fellas with your eyes exposed, and their emission plumes directed right in your face.
In mitigation of aerosol hazards, eye protection is a standard part of required kit, because those from the correct domain of expertise, Industrial Hygiene, know enough about human anatomy to remember the interconnectivity of facial structures.
Ocular transmission of SARS-CoV-2
There has been a great deal of focus on respiratory protection since the start of the pandemic, but ocular transmission was already established for SARS-CoV-1.
“SARS-CoV-1 has been shown to be transmitted through direct contact or with droplet or aerosolized particle contact with the mucous membranes of the eyes, nose and mouth. Indeed, during the 2003 SARS-CoV-1 outbreak in Toronto, health care workers who failed to wear eye protection in caring for patients infected with SARS-CoV-1 had a higher rate of seroconversion.”
We are beginning to see mounting research on ocular transmission for SARS-CoV-2 emerge, as well, traveling through the nasolacrimal duct from the eye, draining into the sinus cavity.
“There is evidence that SARS-CoV-2 may either directly infect cells on the ocular surface, or virus can be carried by tears through the nasolacrimal duct to infect the nasal or gastrointestinal epithelium.”
“The nasolacrimal system provides an anatomic connection between the ocular surface and the upper respiratory tract. When a drop is instilled into the eye, even though some of it is absorbed by the cornea and the conjunctiva, most of it is drained into the nasal cavity through the nasolacrimal canal and is subsequently transferred to the upper respiratory or the gastrointestinal tract.”
“SARS-CoV-2 on the ocular surface can be transferred to different systems along with tears through the nasolacrimal route.”
Seldom did ocular exposure result in eye infection, while systemic infections occurred regularly. Ocular exposure cannot always be determined as the point of contact for this reason, as an eye infection does not always coincide with systemic infection.
The nasolacrimal duct is often discussed in ocular transmission research, but this is not the sole ocular transmission pathway discussed.
“There are two pathways by which ocular exposure could lead to systemic transmission of the SARS-CoV-2 virus. (1) Direct infection of ocular tissues including cornea, conjunctiva, lacrimal gland, meibomian glands from virus exposure and (2) virus in the tears, which then goes through the nasolacrimal duct to infect the nasal or gastrointestinal epithelium.”
Additionally, research is being conducted on the usage of ocular secretions in transmitting SARS-CoV-2.
“Then here comes the question, whether SARS-CoV-2 detected in conjunctival secretions and tears is an infectious virus? Colavita et al inoculated Vero E6 cells with the first RNA positive ocular sample obtained from a COVID-19 patient. Cytopathic effect was observed 5 days post-inoculation, and viral replication was confirmed by real-time RT-PCR in spent cell medium. Hui et al also isolated SARS-CoV-2 virus from a nasopharyngeal aspirate specimen and a throat swab of a COVID-19 patient. The isolated virus not only infected human conjunctival explants but also infected more extensively and reached higher infectious viral titers than SARS-CoV.”
According to this study, ocular secretions were highly infectious.
“The ocular surface can serve as a reservoir and source of contagion for SARS-CoV-2. SARS-CoV-2 can be transmitted to the ocular surface through hand-eye contact and aerosols, and then transfer to other systems through nasolacrimal route and hematogenous metastasis. The possibility of ocular transmission of SARS-CoV-2 cannot be ignored.”
This paper also has a focus on aerosols coming into contact with ocular mucosa.
“Once aerosols form, SARS-CoV-2 can bind to the ACE2 on the exposed ocular mucosa to cause infection. In order to prevent aerosols from contacting the eye surface, eye protection cannot be ignored.”
An additional area explored in this analysis discusses rhesus macaques wherein solely those inoculated through the ocular route became infected.
“If the ocular surface is the portal for SARS-CoV-2 to enter, where does the virus transfer after entering? An animal experiment reveals the possible nasolacrimal routes of SARS-CoV-2 transfer from the ocular surface. Five rhesus macaques were inoculated with 1×106 50% tissue-culture infectious doses of SARS-CoV-2. Only in the conjunctival swabs of rhesus macaques inoculated via conjunctival route could the SARS-CoV-2 be detected. Conjunctival swabs of the rhesus macaques that were inoculated via intragastric or intratracheal route were negative. Three days post conjunctival inoculation, rhesus macaques presented mild interstitial pneumonia. Autopsies showed that SARS-CoV-2 was detectable in the nasolacrimal system tissues, including the lacrimal gland, conjunctiva, nasal cavity, and throat, which connected the eyes and respiratory tract on anatomy.”
An additional macaque study had similar findings.
“Deng et al. showed that SARS-CoV-2 infection could be induced by ocular surface inoculation in an experimental animal model using macaques. Although the researchers detected the virus in conjunctival swabs only on the first day after inoculation, they continued to detect it in nasal and throat swabs 1-7 days after the inoculation. Their findings demonstrated that the viral load in the airway mucosa was much higher than that in the ocular surface. They euthanized and necropsied one of the conjunctival inoculated-animals and found that the virus had spread to the nasolacrimal system and ocular tissue, nasal cavity, pharynx, trachea, tissues in the oral cavity, tissues in the lower-left lobe of the lung, inguinal and perirectal lymph node, stomach, duode-num, cecum, and ileum. They also found a specific IgG antibody, indicating that the animal was infected with SARS-CoV-2 via the ocular surface route.”
While the nasolacrimal route is the primary focus in most current research, the blood-retinal barrier (BRB) is also discussed as a possible pathway.
“Once it reaches the ocular surface, SARS-CoV-2 could invade the conjunctiva and iris under the mediation of ACE2 and CD147, another possible receptor for SARS-CoV-2 on host cells. De Figueiredo et al described the following possible pathways. After reaching blood capillaries and then choroid plexus, the virus reaches the blood-retinal barrier (BRB), which expresses both ACE2 and CD147 in retinal pigment epithelial cells and blood vessel endothelial cells. Since CD147 mediates the breakdown of neurovascular blood barriers, the virus can cross the BRB and enter into blood.”
RSV
There has been a push recently to bring back masks for Respiratory Syncytial Virus (RSV), especially in schools, as this pathogen largely impacts youth populations, yet ocular transmission is a proven method of infectivity for RSV.
In this paper, intranasal dosing of the given pathogen resulted in onset of illness for nearly all respiratory pathogens studied. It reviews transmission routes and minimum infective dose for Influenza, Rhinovirus, Coxsackievirus, Adenovirus, RSV, Enteric Viruses, Rotavirus, Norovirus, and Echovirus, including ocular transmission.
“The infective doses of rhinoviruses in the nose and eyes are thought to be comparable because the virus does not infect the eyes but appears to travel from the eyes to the nasal mucosa via the tear duct.”
“Hall et al. (1981) investigated the infectivity of RSV A2 strain administered by nose, eye, and mouth in adult volunteers. They reported that the virus may infect by eye or nose and both routes appear to be equally sensitive. A dose of 1.6 × 105 TCID50 infected three of the four volunteers given either into the eyes or nose while only one out of the eight were infected via mouth inoculation, and this was thought to be due to secondary spread of the virus.”
“RSV A2 had poor infectivity when administered via the mouth but was shown to infect by eye and nose and both routes appear to be equally sensitive to the virus.”
“Bynoe et al. (1961) found that colds could be produced almost as readily by applying virus by nasal and conjunctival swabs as by giving nasal drops to volunteers.”
Would masks save schools from RSV circulation? Most kids have robust immune systems, with a very, very small percentage of the youth population undergoing chemotherapy or taking immunosuppressives, who usually are not on campus for in-person learning. But for those seeming protection and in-person instruction, we must not set them up for immune bombardment by offering a false sense of security while feigning ignorance of other viable transmission routes. Masks are not the answer.
Summary
Ocular transmission of respiratory pathogens hasn’t been a focal point of study, but with other pathogens and mounting research on SARS-CoV-2 showing such ease of systemic onset for this transmission route, more attention should be given to this area of research.
Consider all of the people you’ve seen donning masks or respirators over these past three years, assured in the merit of their virtue. How many still got sick? Did you ever once see someone donning goggles? Are we ever going to get around to discussing exhaustion of the hierarchy of controls, or are actual mitigating measures too taboo, too fringe?
TLDR: Ocular transmission is a viable method of transmission for SARS-CoV-2. Masks are not source control. Even N95s aren’t going to fix this. And all child masks are unregulated, untested, unethical, and unsafe, with zero efficacy, fit, term of wear, or medical clearance standards, and with ocular transmission being a proven route of transmission for RSV, masks aren’t going to fix that issue, either.
Brownstone Institute
The Unmasking of Vaccine Science

From the Brownstone Institute
By
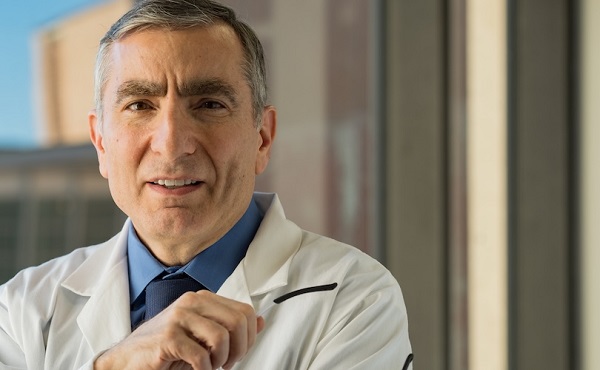
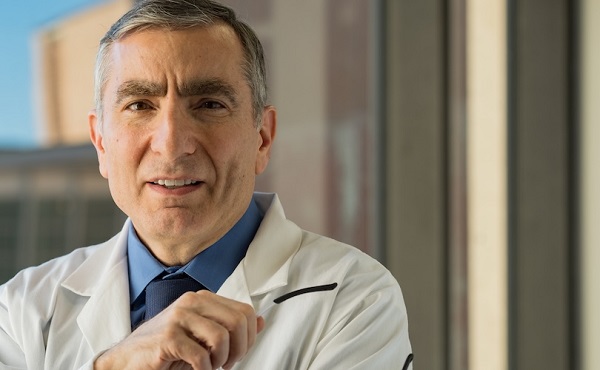
I recently purchased Aaron Siri’s new book Vaccines, Amen. As I flipped though the pages, I noticed a section devoted to his now-famous deposition of Dr Stanley Plotkin, the “godfather” of vaccines.
I’d seen viral clips circulating on social media, but I had never taken the time to read the full transcript — until now.
Siri’s interrogation was methodical and unflinching…a masterclass in extracting uncomfortable truths.
A Legal Showdown
In January 2018, Dr Stanley Plotkin, a towering figure in immunology and co-developer of the rubella vaccine, was deposed under oath in Pennsylvania by attorney Aaron Siri.
The case stemmed from a custody dispute in Michigan, where divorced parents disagreed over whether their daughter should be vaccinated. Plotkin had agreed to testify in support of vaccination on behalf of the father.
What followed over the next nine hours, captured in a 400-page transcript, was extraordinary.
Plotkin’s testimony revealed ethical blind spots, scientific hubris, and a troubling indifference to vaccine safety data.
He mocked religious objectors, defended experiments on mentally disabled children, and dismissed glaring weaknesses in vaccine surveillance systems.
A System Built on Conflicts
From the outset, Plotkin admitted to a web of industry entanglements.
He confirmed receiving payments from Merck, Sanofi, GSK, Pfizer, and several biotech firms. These were not occasional consultancies but long-standing financial relationships with the very manufacturers of the vaccines he promoted.
Plotkin appeared taken aback when Siri questioned his financial windfall from royalties on products like RotaTeq, and expressed surprise at the “tone” of the deposition.
Siri pressed on: “You didn’t anticipate that your financial dealings with those companies would be relevant?”
Plotkin replied: “I guess, no, I did not perceive that that was relevant to my opinion as to whether a child should receive vaccines.”
The man entrusted with shaping national vaccine policy had a direct financial stake in its expansion, yet he brushed it aside as irrelevant.
Contempt for Religious Dissent
Siri questioned Plotkin on his past statements, including one in which he described vaccine critics as “religious zealots who believe that the will of God includes death and disease.”
Siri asked whether he stood by that statement. Plotkin replied emphatically, “I absolutely do.”
Plotkin was not interested in ethical pluralism or accommodating divergent moral frameworks. For him, public health was a war, and religious objectors were the enemy.
He also admitted to using human foetal cells in vaccine production — specifically WI-38, a cell line derived from an aborted foetus at three months’ gestation.
Siri asked if Plotkin had authored papers involving dozens of abortions for tissue collection. Plotkin shrugged: “I don’t remember the exact number…but quite a few.”
Plotkin regarded this as a scientific necessity, though for many people — including Catholics and Orthodox Jews — it remains a profound moral concern.
Rather than acknowledging such sensitivities, Plotkin dismissed them outright, rejecting the idea that faith-based values should influence public health policy.
That kind of absolutism, where scientific aims override moral boundaries, has since drawn criticism from ethicists and public health leaders alike.
As NIH director Jay Bhattacharya later observed during his 2025 Senate confirmation hearing, such absolutism erodes trust.
“In public health, we need to make sure the products of science are ethically acceptable to everybody,” he said. “Having alternatives that are not ethically conflicted with foetal cell lines is not just an ethical issue — it’s a public health issue.”
Safety Assumed, Not Proven
When the discussion turned to safety, Siri asked, “Are you aware of any study that compares vaccinated children to completely unvaccinated children?”
Plotkin replied that he was “not aware of well-controlled studies.”
Asked why no placebo-controlled trials had been conducted on routine childhood vaccines such as hepatitis B, Plotkin said such trials would be “ethically difficult.”
That rationale, Siri noted, creates a scientific blind spot. If trials are deemed too unethical to conduct, then gold-standard safety data — the kind required for other pharmaceuticals — simply do not exist for the full childhood vaccine schedule.
Siri pointed to one example: Merck’s hepatitis B vaccine, administered to newborns. The company had only monitored participants for adverse events for five days after injection.
Plotkin didn’t dispute it. “Five days is certainly short for follow-up,” he admitted, but claimed that “most serious events” would occur within that time frame.
Siri challenged the idea that such a narrow window could capture meaningful safety data — especially when autoimmune or neurodevelopmental effects could take weeks or months to emerge.
Siri pushed on. He asked Plotkin if the DTaP and Tdap vaccines — for diphtheria, tetanus and pertussis — could cause autism.
“I feel confident they do not,” Plotkin replied.
But when shown the Institute of Medicine’s 2011 report, which found the evidence “inadequate to accept or reject” a causal link between DTaP and autism, Plotkin countered, “Yes, but the point is that there were no studies showing that it does cause autism.”
In that moment, Plotkin embraced a fallacy: treating the absence of evidence as evidence of absence.
“You’re making assumptions, Dr Plotkin,” Siri challenged. “It would be a bit premature to make the unequivocal, sweeping statement that vaccines do not cause autism, correct?”
Plotkin relented. “As a scientist, I would say that I do not have evidence one way or the other.”
The MMR
The deposition also exposed the fragile foundations of the measles, mumps, and rubella (MMR) vaccine.
When Siri asked for evidence of randomised, placebo-controlled trials conducted before MMR’s licensing, Plotkin pushed back: “To say that it hasn’t been tested is absolute nonsense,” he said, claiming it had been studied “extensively.”
Pressed to cite a specific trial, Plotkin couldn’t name one. Instead, he gestured to his own 1,800-page textbook: “You can find them in this book, if you wish.”
Siri replied that he wanted an actual peer-reviewed study, not a reference to Plotkin’s own book. “So you’re not willing to provide them?” he asked. “You want us to just take your word for it?”
Plotkin became visibly frustrated.
Eventually, he conceded there wasn’t a single randomised, placebo-controlled trial. “I don’t remember there being a control group for the studies, I’m recalling,” he said.
The exchange foreshadowed a broader shift in public discourse, highlighting long-standing concerns that some combination vaccines were effectively grandfathered into the schedule without adequate safety testing.
In September this year, President Trump called for the MMR vaccine to be broken up into three separate injections.
The proposal echoed a view that Andrew Wakefield had voiced decades earlier — namely, that combining all three viruses into a single shot might pose greater risk than spacing them out.
Wakefield was vilified and struck from the medical register. But now, that same question — once branded as dangerous misinformation — is set to be re-examined by the CDC’s new vaccine advisory committee, chaired by Martin Kulldorff.
The Aluminium Adjuvant Blind Spot
Siri next turned to aluminium adjuvants — the immune-activating agents used in many childhood vaccines.
When asked whether studies had compared animals injected with aluminium to those given saline, Plotkin conceded that research on their safety was limited.
Siri pressed further, asking if aluminium injected into the body could travel to the brain. Plotkin replied, “I have not seen such studies, no, or not read such studies.”
When presented with a series of papers showing that aluminium can migrate to the brain, Plotkin admitted he had not studied the issue himself, acknowledging that there were experiments “suggesting that that is possible.”
Asked whether aluminium might disrupt neurological development in children, Plotkin stated, “I’m not aware that there is evidence that aluminum disrupts the developmental processes in susceptible children.”
Taken together, these exchanges revealed a striking gap in the evidence base.
Compounds such as aluminium hydroxide and aluminium phosphate have been injected into babies for decades, yet no rigorous studies have ever evaluated their neurotoxicity against an inert placebo.
This issue returned to the spotlight in September 2025, when President Trump pledged to remove aluminium from vaccines, and world-leading researcher Dr Christopher Exley renewed calls for its complete reassessment.
A Broken Safety Net
Siri then turned to the reliability of the Vaccine Adverse Event Reporting System (VAERS) — the primary mechanism for collecting reports of vaccine-related injuries in the United States.
Did Plotkin believe most adverse events were captured in this database?
“I think…probably most are reported,” he replied.
But Siri showed him a government-commissioned study by Harvard Pilgrim, which found that fewer than 1% of vaccine adverse events are reported to VAERS.
“Yes,” Plotkin said, backtracking. “I don’t really put much faith into the VAERS system…”
Yet this is the same database officials routinely cite to claim that “vaccines are safe.”
Ironically, Plotkin himself recently co-authored a provocative editorial in the New England Journal of Medicine, conceding that vaccine safety monitoring remains grossly “inadequate.”
Experimenting on the Vulnerable
Perhaps the most chilling part of the deposition concerned Plotkin’s history of human experimentation.
“Have you ever used orphans to study an experimental vaccine?” Siri asked.
“Yes,” Plotkin replied.
“Have you ever used the mentally handicapped to study an experimental vaccine?” Siri asked.
“I don’t recollect…I wouldn’t deny that I may have done so,” Plotkin replied.
Siri cited a study conducted by Plotkin in which he had administered experimental rubella vaccines to institutionalised children who were “mentally retarded.”
Plotkin stated flippantly, “Okay well, in that case…that’s what I did.”
There was no apology, no sign of ethical reflection — just matter-of-fact acceptance.
Siri wasn’t done.
He asked if Plotkin had argued that it was better to test on those “who are human in form but not in social potential” rather than on healthy children.
Plotkin admitted to writing it.
Siri established that Plotkin had also conducted vaccine research on the babies of imprisoned mothers, and on colonised African populations.
Plotkin appeared to suggest that the scientific value of such studies outweighed the ethical lapses—an attitude that many would interpret as the classic ‘ends justify the means’ rationale.
But that logic fails the most basic test of informed consent. Siri asked whether consent had been obtained in these cases.
“I don’t remember…but I assume it was,” Plotkin said.
Assume?
This was post-Nuremberg research. And the leading vaccine developer in America couldn’t say for sure whether he had properly informed the people he experimented on.
In any other field of medicine, such lapses would be disqualifying.
A Casual Dismissal of Parental Rights
Plotkin’s indifference to experimenting on disabled children didn’t stop there.
Siri asked whether someone who declined a vaccine due to concerns about missing safety data should be labelled “anti-vax.”
Plotkin replied, “If they refused to be vaccinated themselves or refused to have their children vaccinated, I would call them an anti-vaccination person, yes.”
Plotkin was less concerned about adults making that choice for themselves, but he had no tolerance for parents making those choices for their own children.
“The situation for children is quite different,” said Plotkin, “because one is making a decision for somebody else and also making a decision that has important implications for public health.”
In Plotkin’s view, the state held greater authority than parents over a child’s medical decisions — even when the science was uncertain.
The Enabling of Figures Like Plotkin
The Plotkin deposition stands as a case study in how conflicts of interest, ideology, and deference to authority have corroded the scientific foundations of public health.
Plotkin is no fringe figure. He is celebrated, honoured, and revered. Yet he promotes vaccines that have never undergone true placebo-controlled testing, shrugs off the failures of post-market surveillance, and admits to experimenting on vulnerable populations.
This is not conjecture or conspiracy — it is sworn testimony from the man who helped build the modern vaccine program.
Now, as Health Secretary Robert F. Kennedy, Jr. reopens long-dismissed questions about aluminium adjuvants and the absence of long-term safety studies, Plotkin’s once-untouchable legacy is beginning to fray.
Republished from the author’s Substack
Brownstone Institute
Bizarre Decisions about Nicotine Pouches Lead to the Wrong Products on Shelves

From the Brownstone Institute
A walk through a dozen convenience stores in Montgomery County, Pennsylvania, says a lot about how US nicotine policy actually works. Only about one in eight nicotine-pouch products for sale is legal. The rest are unauthorized—but they’re not all the same. Some are brightly branded, with uncertain ingredients, not approved by any Western regulator, and clearly aimed at impulse buyers. Others—like Sweden’s NOAT—are the opposite: muted, well-made, adult-oriented, and already approved for sale in Europe.
Yet in the United States, NOAT has been told to stop selling. In September 2025, the Food and Drug Administration (FDA) issued the company a warning letter for offering nicotine pouches without marketing authorization. That might make sense if the products were dangerous, but they appear to be among the safest on the market: mild flavors, low nicotine levels, and recyclable paper packaging. In Europe, regulators consider them acceptable. In America, they’re banned. The decision looks, at best, strange—and possibly arbitrary.
What the Market Shows
My October 2025 audit was straightforward. I visited twelve stores and recorded every distinct pouch product visible for sale at the counter. If the item matched one of the twenty ZYN products that the FDA authorized in January, it was counted as legal. Everything else was counted as illegal.
Two of the stores told me they had recently received FDA letters and had already removed most illegal stock. The other ten stores were still dominated by unauthorized products—more than 93 percent of what was on display. Across all twelve locations, about 12 percent of products were legal ZYN, and about 88 percent were not.
The illegal share wasn’t uniform. Many of the unauthorized products were clearly high-nicotine imports with flashy names like Loop, Velo, and Zimo. These products may be fine, but some are probably high in contaminants, and a few often with very high nicotine levels. Others were subdued, plainly meant for adult users. NOAT was a good example of that second group: simple packaging, oat-based filler, restrained flavoring, and branding that makes no effort to look “cool.” It’s the kind of product any regulator serious about harm reduction would welcome.
Enforcement Works
To the FDA’s credit, enforcement does make a difference. The two stores that received official letters quickly pulled their illegal stock. That mirrors the agency’s broader efforts this year: new import alerts to detain unauthorized tobacco products at the border (see also Import Alert 98-06), and hundreds of warning letters to retailers, importers, and distributors.
But effective enforcement can’t solve a supply problem. The list of legal nicotine-pouch products is still extremely short—only a narrow range of ZYN items. Adults who want more variety, or stores that want to meet that demand, inevitably turn to gray-market suppliers. The more limited the legal catalog, the more the illegal market thrives.
Why the NOAT Decision Appears Bizarre
The FDA’s own actions make the situation hard to explain. In January 2025, it authorized twenty ZYN products after finding that they contained far fewer harmful chemicals than cigarettes and could help adult smokers switch. That was progress. But nine months later, the FDA has approved nothing else—while sending a warning letter to NOAT, arguably the least youth-oriented pouch line in the world.
The outcome is bad for legal sellers and public health. ZYN is legal; a handful of clearly risky, high-nicotine imports continue to circulate; and a mild, adult-market brand that meets European safety and labeling rules is banned. Officially, NOAT’s problem is procedural—it lacks a marketing order. But in practical terms, the FDA is punishing the very design choices it claims to value: simplicity, low appeal to minors, and clean ingredients.
This approach also ignores the differences in actual risk. Studies consistently show that nicotine pouches have far fewer toxins than cigarettes and far less variability than many vapes. The biggest pouch concerns are uneven nicotine levels and occasional traces of tobacco-specific nitrosamines, depending on manufacturing quality. The serious contamination issues—heavy metals and inconsistent dosage—belong mostly to disposable vapes, particularly the flood of unregulated imports from China. Treating all “unauthorized” products as equally bad blurs those distinctions and undermines proportional enforcement.
A Better Balance: Enforce Upstream, Widen the Legal Path
My small Montgomery County survey suggests a simple formula for improvement.
First, keep enforcement targeted and focused on suppliers, not just clerks. Warning letters clearly change behavior at the store level, but the biggest impact will come from auditing distributors and importers, and stopping bad shipments before they reach retail shelves.
Second, make compliance easy. A single-page list of authorized nicotine-pouch products—currently the twenty approved ZYN items—should be posted in every store and attached to distributor invoices. Point-of-sale systems can block barcodes for anything not on the list, and retailers could affirm, once a year, that they stock only approved items.
Third, widen the legal lane. The FDA launched a pilot program in September 2025 to speed review of new pouch applications. That program should spell out exactly what evidence is needed—chemical data, toxicology, nicotine release rates, and behavioral studies—and make timely decisions. If products like NOAT meet those standards, they should be authorized quickly. Legal competition among adult-oriented brands will crowd out the sketchy imports far faster than enforcement alone.
The Bottom Line
Enforcement matters, and the data show it works—where it happens. But the legal market is too narrow to protect consumers or encourage innovation. The current regime leaves a few ZYN products as lonely legal islands in a sea of gray-market pouches that range from sensible to reckless.
The FDA’s treatment of NOAT stands out as a case study in inconsistency: a quiet, adult-focused brand approved in Europe yet effectively banned in the US, while flashier and riskier options continue to slip through. That’s not a public-health victory; it’s a missed opportunity.
If the goal is to help adult smokers move to lower-risk products while keeping youth use low, the path forward is clear: enforce smartly, make compliance easy, and give good products a fair shot. Right now, we’re doing the first part well—but failing at the second and third. It’s time to fix that.
-

 Digital ID1 day ago
Digital ID1 day agoCanadian government launches trial version of digital ID for certain licenses, permits
-

 Alberta1 day ago
Alberta1 day agoAlberta Next Panel calls to reform how Canada works
-

 Agriculture1 day ago
Agriculture1 day agoEnd Supply Management—For the Sake of Canadian Consumers
-

 International1 day ago
International1 day agoGeorgia county admits illegally certifying 315k ballots in 2020 presidential election
-

 Business1 day ago
Business1 day agoThe “Disruptor-in-Chief” places Canada in the crosshairs
-

 Artificial Intelligence1 day ago
Artificial Intelligence1 day agoUK Police Pilot AI System to Track “Suspicious” Driver Journeys
-

 Energy1 day ago
Energy1 day ago‘The electric story is over’
-
 International1 day ago
International1 day agoWorld-leading biochemist debunks evolutionary theory










