Health
AHS Expanding Pertussis Program In Central Zone
By Sheldon Spackman
Sustained high rates of pertussis in Alberta Health Service’s Central Zone has led officials to expand their routine pertussis immunization program.
As of November 1st, women in their third trimester of pregnancy, regardless of previous pertussis immunization, can now get the pertussis vaccine.
In a release, AHS officials say offering vaccine to women in the third trimester of pregnancy is an important step in protecting infants, who are the most vulnerable to developing severe complications from pertussis.
Dr. Digby Horne is the Medical Officer of Health for the Central Zone and says “Immunization is not only safe and protective for pregnant women, it provides immunity to their infants after birth, protecting these infants before they’re old enough to be immunized themselves.”
Women in Central Zone who are 26 or more weeks pregnant are encouraged to call their local community health centre to book an appointment for this immunization. It’s also important to note that the pertussis vaccine will not be offered through influenza immunization clinics that are currently underway.
Pertussis is a bacterial infection that causes severe coughing that lasts for weeks and can lead to pneumonia, convulsions, brain damage and even death.
Health
RFK Jr. promises to identify cause of autism ‘epidemic’ by September

From LifeSiteNews
Robert F. Kennedy Jr. explained that autism rates continue to climb, and are now expected to impact 1 in 31 children, up from ‘1 in 10,000 when I was a kid.’
Health and Human Services (HHS) Secretary Robert F. Kennedy Jr. said that his agency has undertaken a multinational study involving “hundreds of scientists around the world” to identify the causes of the growing incidence of autism in children.
“We’ve launched a massive testing and research effort that’s going to involve hundreds of scientists from around the world,” Kennedy told President Trump during Thursday’s White House Cabinet meeting. “By September, we will know what has caused the autism epidemic, and we’ll be able to eliminate those exposures.”
Kennedy explained that autism rates continue to climb, and are now expected to impact 1 in 31 children, up from “1 in 10,000 when I was a kid.”
“It’s a horrible statistic,” Trump said of the latest autism rate figures. “There’s got to be something artificial out there that’s doing this.”
“There will be no bigger news conference than when you come up with that answer,” predicted the president.
As recently as 2000, Centers for Disease Control and Prevention (CDC) research showed that 1 in 150 children were diagnosed with autism.
While many mainstream autism researchers adhere to theories that the rising rate of autism is due to “increased awareness” and an evolving, broadening definition of autism, Kennedy holds to that belief that the cause will be found primarily in environmental factors, eating habits, and currently accepted standard medical protocols.
“We’re going to look at vaccines, but we’re going to look at everything. Everything is on the table, our food system, our water, our air, different ways of parenting, all the kind of changes that may have triggered this epidemic,” the HHS head told Fox News.
“It is an epidemic,” Kennedy insisted. “Epidemics are not caused by genes. Genes can provide a vulnerability, but you need an environmental toxin.”
“We know that it is an environmental toxin that is causing this cataclysm,” said Kennedy, “and we are going to identify it.”
Kennedy is known for vehemently opposing vaccines, a stance he adopted after the mothers of vaccine-injured children implored him to look into the research linking thimerosal to neurological injuries, including autism. He went on to found Children’s Health Defense, an organization with the stated mission of “ending childhood health epidemics by eliminating toxic exposure,” largely through vaccines.
The federal government spent more than $300 million on autism research in 2023, according to a report by The Hill.
Health
RFK Jr. Shuts Down Measles Scare in His First Network Interview as HHS Secretary

 The Vigilant Fox
The Vigilant Fox
CBS’s Jon LaPook tried to hype the measles panic, but Kennedy calmly dismantled the narrative and set the record straight.
The following is a streamlined and editorialized version of a thread that originally appeared on the American Values X page. It was edited and republished with permission. Click here to read the original thread.
HHS Secretary RFK Jr. recently set the record straight in an interview with CBS News’ chief medical correspondent, Dr. Jon LaPook. He pushed back on the claim that a second child had died from measles, exposing the narrative as not just misleading, but flat-out false.
But before that happened, Kennedy addressed the current measles outbreak and ongoing concerns about vaccine safety. He revealed that new safety trials are finally in motion.
“We don’t know the risks of many of these products,” he said. “They’re not adequately safety-tested.” He explained that “many of the vaccines are tested for only 3-4 days with NO placebo group.”
Kennedy made it clear this isn’t about banning vaccines—it’s about transparency. “I’ve always said … I’m not gonna take people’s vaccines away from them,” he said. “I’m gonna make sure that we have good science so that people can make an informed choice.” He added, “We are doing that science today.”
Kennedy was asked about Daisy Hildebrand, the young girl in Texas whose funeral he attended. Her death had been cited in headlines as proof of a growing measles crisis.
“It was very nice to be able to meet the parents in person and spend the whole day with them and share their lives with them and get to know their community,” he said. “The community was very welcoming and loving towards me.”
Kennedy described the experience warmly: “The Mennonite community was beautiful to me.” He added, “I went to a large lunch with the whole community and you had boys and girls sitting together and nobody was on a cell phone.”
That’s when Kennedy dropped the real bombshell: the child didn’t die from measles.
“The child whose funeral I attended this week was hospitalized three times from other illnesses,” he said. “She got measles and she got over the measles, according to her parents.” He added, “I saw the medical report on it today and the thing that killed her was not the measles, but it was a bacteriological infection.”
And it wasn’t the first time the media misled the public. Last month, another child’s death was falsely blamed on measles. But the truth is that it was a case of catastrophic medical error.
“Her death is the result of an egregious medical error,” CHD’s Mary Holland told Steve Bannon. “This girl wound up in the hospital because she did have some difficulty breathing, and instead of giving her breathing care, you’ll understand from the specialists with me that she got inaccurate, wrong-headed medical care, and that’s why she died.”
She added, “She did not die from measles. She died from a medical error, the third leading cause of death in this country.”
Thanks for reading. If you value the work being published here, upgrading your subscription is the most powerful way to support it. The more this Substack earns, the more we can expand the team, improve quality, and create the best reader experience possible.
For the full experience, upgrade your subscription.
-

 Business2 days ago
Business2 days agoStocks soar after Trump suspends tariffs
-
 COVID-192 days ago
COVID-192 days agoBiden Admin concealed report on earliest COVID cases from 2019
-

 Business2 days ago
Business2 days agoScott Bessent Says Trump’s Goal Was Always To Get Trading Partners To Table After Major Pause Announcement
-

 2025 Federal Election1 day ago
2025 Federal Election1 day agoResearchers Link China’s Intelligence and Elite Influence Arms to B.C. Government, Liberal Party, and Trudeau-Appointed Senator
-
 Business1 day ago
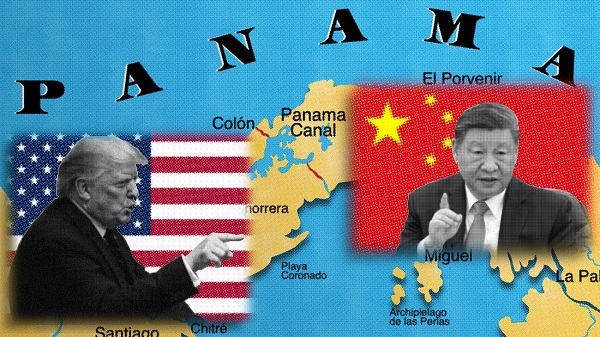
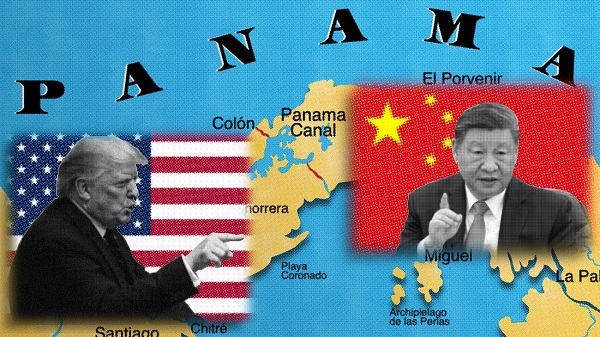
Business1 day agoTimeline: Panama Canal Politics, Policy, and Tensions
-

 COVID-191 day ago
COVID-191 day agoFauci, top COVID officials have criminal referral requests filed against them in 7 states
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoRCMP memo warns of Chinese interference on Canadian university campuses to affect election
-

 2025 Federal Election2 days ago
2025 Federal Election2 days agoThe status quo in Canadian politics isn’t sustainable for national unity









